Abstract
Infections due to Scedosporium/Pseudallescheria species are increasingly recognized in both immunocompromised and immunocompetent hosts. Patients with organ and stem cell transplants and malignancy are at high risk for infection. Infection is also acquired through trauma and near-drowning incidents. Scedosporium apiospermum complex and Lomentospora prolificans (previously Scedosporium prolificans) account for most infections. Increasing use of sequencing-based molecular tools to identify these fungi has enabled better understanding of species-specific differences in geographical distribution, clinical epidemiology and presentation. S. apiospermum complex infections occur worldwide, affect diverse host groups and has protean clinical manifestations. L. prolificans typically causes infection in immunocompromised patients and is associated with disseminated infection and high mortality. S. aurantiacum (a member of S. apiospermum complex) has a propensity to be isolated from patients with cystic fibrosis and other chronic lung disease. Case clusters of L. prolificans infection have occurred. Appreciation of epidemiology is important to inform rapid diagnostics and antifungal therapy.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Harun A, Gilgado F, Chen SC, Meyer W. Abundance of Pseudallescheria/Scedosporium species in the Australian urban environment suggests a possible source for scedosporiosis including the colonization of airways in cystic fibrosis. Med Mycol. 2010;48 Suppl 1:S70–6. doi:10.3109/13693786.2010.515254.
Kaltseis J, Rainer J, De Hoog GS. Ecology of Pseudallescheria and Scedosporium species in human-dominated and natural environments and their distribution in clinical samples. Med Mycol. 2009;47(4):398–405. doi:10.1080/13693780802585317.
Cortez KJ, Roilides E, Quiroz-Telles F, Meletiadis J, Antachopoulos C, Knudsen T, et al. Infections caused by Scedosporium spp. Clin Microbiol Rev. 2008;21(1):157–97. doi:10.1128/CMR.00039-07.
Grenouillet F, Botterel F, Crouzet J, Larosa F, Hicheri Y, Forel JM, et al. Scedosporium prolificans: an emerging pathogen in France? Med Mycol. 2009;47(4):343–50. doi:10.1080/13693780802454761.
Heath CH, Slavin MA, Sorrell TC, Handke R, Harun A, Phillips M, et al. Population-based surveillance for scedosporiosis in Australia: epidemiology, disease manifestations and emergence of Scedosporium aurantiacum infection. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis. 2009;15(7):689–93. doi:10.1111/j.1469-0691.2009.02802.x.
Issakainen J, Salonen JH, Anttila VJ, Koukila-Kähkölä P, Castrén M, Liimatainen O, et al. Deep, respiratory tract and ear infections caused byPseudallescheria (Scedosporium) and Microascus(Scopulariopsis) in Finland. A 10-year retrospective multi-center study. Med Mycol. 2010;48(3):458–65. doi:10.3109/13693780903161208.
Rodriguez-Tudela JL, Berenguer J, Guarro J, Kantarcioglu AS, Horre R, de Hoog GS, et al. Epidemiology and outcome of Scedosporium prolificans infection, a review of 162 cases. Med Mycol. 2009;47(4):359–70. doi:10.1080/13693780802524506.
Heng SC, Slavin MA, Chen SC, Heath CH, Nguyen Q, Billah B, et al. Hospital costs, length of stay and mortality attributable to invasive scedosporiosis in haematology patients. J Antimicrob Chemother. 2012;67(9):2274–82. doi:10.1093/jac/dks210. This Australian study demonstrated that invasive scedosporiosis in haematology patients is associated with prolonged hospitalisation, excess hospital costs and mortality compared to control patients.
Troke P, Aguirrebengoa K, Arteaga C, Ellis D, Heath CH, Lutsar I, et al. Treatment of scedosporiosis with voriconazole: clinical experience with 107 patients. Antimicrob Agents Chemother. 2008;52(5):1743–50. doi:10.1128/AAC.01388-07.
Lackner M, Hagen F, Meis JF, van den Ende AH G, Vu D, Robert V, et al. Susceptibility and diversity in the therapy-refractory genus scedosporium. Antimicrob Agents Chemother. 2014;58(10):5877–85. doi:10.1128/AAC.03211-14. In this study, genetic diversity between Scedosporium species were analysed to establish distribution of resistance between species and strains.
Lackner M, de Hoog GS, Yang L, Moreno LF, Ahmed SA, Andreas F, et al. Proposed nomenclature for Pseudallescheria, Scedosporium and related genera. Fungal Divers. 2014;67(1):1–10. This paper explains the current nomenclature of species within the genus Scedosporium.
Blyth CC, Middleton PG, Harun A, Sorrell TC, Meyer W, Chen SC. Clinical associations and prevalence of Scedosporium spp. in Australian cystic fibrosis patients: identification of novel risk factors? Med Mycol. 2010;48 Suppl 1:S37–44. doi:10.3109/13693786.2010.500627.
Lackner M, Rezusta A, Villuendas MC, Palacian MP, Meis JF, Klaassen CH. Infection and colonisation due to scedosporium in Northern Spain. An in vitro antifungal susceptibility and molecular epidemiology study of 60 isolates. Mycoses. 2011;54 Suppl 3:12–21. doi:10.1111/j.1439-0507.2011.02110.x.
Song MJ, Lee JH, Lee NY. Fatal Scedosporium prolificans infection in a paediatric patient with acute lymphoblastic leukaemia. Mycoses. 2011;54(1):81–3. doi:10.1111/j.1439-0507.2009.01765.x.
Tintelnot K, Just-Nubling G, Horre R, Graf B, Sobottka I, Seibold M, et al. A review of German Scedosporium prolificans cases from 1993 to 2007. Med Mycol. 2009;47(4):351–8. doi:10.1080/13693780802627440.
Ramsperger M, Duan S, Sorrell TC, Meyer W, Chen SC-A. The genus Scedosporium and Pseudallescheria: current challenges in laboratory diagnosis. Curr Clin Microbiol Rep. 2014;1(1–2):27–36. This review article summarises the current culture and molecular based laboratory methods for identification of Scedosporium spp. including use of selective media, DNA sequencing, pan-fungal PCR and restriction fragment length polymorphism.
Lu Q, van den Ende AH G, Bakkers JM, Sun J, Lackner M, Najafzadeh MJ, et al. Identification of Pseudallescheria and Scedosporium species by three molecular methods. J Clin Microbiol. 2011;49(3):960–7. doi:10.1128/JCM.01813-10.
Delhaes L, Harun A, Chen SC, Nguyen Q, Slavin M, Heath CH, et al. Molecular typing of Australian Scedosporium isolates showing genetic variability and numerous S. aurantiacum. Emerg Infect Dis. 2008;14(2):282–90. doi:10.3201/eid1402.070920.
Gilgado F, Cano J, Gene J, Guarro J. Molecular phylogeny of the Pseudallescheria boydii species complex: proposal of two new species. J Clin Microbiol. 2005;43(10):4930–42. doi:10.1128/JCM.43.10.4930-4942.2005.
Gilgado F, Cano J, Gene J, Sutton DA, Guarro J. Molecular and phenotypic data supporting distinct species statuses for Scedosporium apiospermum and Pseudallescheria boydii and the proposed new species Scedosporium dehoogii. J Clin Microbiol. 2008;46(2):766–71. doi:10.1128/JCM.01122-07.
Cooley L, Spelman D, Thursky K, Slavin M. Infection with Scedosporium apiospermum and S. prolificans, Australia. Emerg Infect Dis. 2007;13(8):1170–7. doi:10.3201/eid1308.060576.
Bhagavatula S, Vale L, Evans J, Carpenter C, Barnes RA. Scedosporium prolificans osteomyelitis following penetrating injury: a case report. Med Mycol Case Rep. 2014;4:26–9. doi:10.1016/j.mmcr.2014.03.002.
Guarro J, Kantarcioglu AS, Horre R, Rodriguez-Tudela JL, Cuenca Estrella M, Berenguer J, et al. Scedosporium apiospermum: changing clinical spectrum of a therapy-refractory opportunist. Med Mycol. 2006;44(4):295–327. doi:10.1080/13693780600752507.
de Hoog GS, Marvin-Sikkema FD, Lahpoor GA, Gottschall JC, Prins RA, Gueho E. Ecology and physiology of the emerging opportunistic fungi Pseudallescheria boydii and Scedosporium prolificans. Mycoses. 1994;37(3–4):71–8.
del Palacio A, Garau M, Amor E, Martinez-Alonso I, Calvo T, Carrillo-Munoz A, et al. Case reports. Transient colonization with Scedosporium prolificans. Report of four cases in Madrid. Mycoses. 2001;44(7–8):321–5.
Idigoras P, Perez-Trallero E, Pineiro L, Larruskain J, Lopez-Lopategui MC, Rodriguez N, et al. Disseminated infection and colonization by Scedosporium prolificans: a review of 18 cases, 1990–1999. Clin Infect Dis. 2001;32(11):E158–65. doi:10.1086/320521.
Feltkamp MC, Kersten MJ, van der Lelie J, Burggraaf JD, de Hoog GS, Kuijper EJ. Fatal Scedosporium prolificans infection in a leukemic patient. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. 1997;16(6):460–4.
Husain S, Munoz P, Forrest G, Alexander BD, Somani J, Brennan K, et al. Infections due to Scedosporium apiospermum and Scedosporium prolificans in transplant recipients: clinical characteristics and impact of antifungal agent therapy on outcome. Clin Infect Dis. 2005;40(1):89–99. doi:10.1086/426445.
Johnson LS, Shields RK, Clancy CJ. Epidemiology, clinical manifestations, and outcomes of Scedosporium infections among solid organ transplant recipients. Transpl Infect Dis Off J Transplant Soc. 2014;16(4):578–87. doi:10.1111/tid.12244. A single centre large retrospective study from the USA that evaluated clinical epidemiology and outcomes of patients with invasive scedosporiosis among the solid organ transplant recipients.
Kooijman CM, Kampinga GA, de Hoog GS, Goudswaard WB, Reijnen MM. Successful treatment of Scedosporium aurantiacum osteomyelitis in an immunocompetent patient. Surg Infect. 2007;8(6):605–10. doi:10.1089/sur.2006.038.
Nakamura Y, Suzuki N, Nakajima Y, Utsumi Y, Murata O, Nagashima H, et al. Scedosporium aurantiacum brain abscess after near-drowning in a survivor of a tsunami in Japan. Respir Investig. 2013;51(4):207–11. doi:10.1016/j.resinv.2013.07.001.
Borghi E, Iatta R, Manca A, Montagna MT, Morace G. Chronic airway colonization by Scedosporium apiospermum with a fatal outcome in a patient with cystic fibrosis. Med Mycol. 2010;48 Suppl 1:S108–13. doi:10.3109/13693786.2010.504239.
Ginter G, de Hoog GS, Pschaid A, Fellinger M, Bogiatzis A, Berghold C, et al. Arthritis without grains caused by Pseudallescheria boydii. Mycoses. 1995;38(9–10):369–71.
Montejo M, Muniz ML, Zarraga S, Aguirrebengoa K, Amenabar JJ, Lopez-Soria L, et al. Case reports. Infection due to Scedosporium apiospermum in renal transplant recipients: a report of two cases and literature review of central nervous system and cutaneous infections by Pseudallescheria boydii/Sc. apiospermum. Mycoses. 2002;45(9–10):418–27.
Marques DS, Pinho Vaz C, Branca R, Campilho F, Lamelas C, Afonso LP, et al. Rhizomucor and scedosporium infection post hematopoietic stem-cell transplant. Case Rep Med. 2011;2011:830769. doi:10.1155/2011/830769.
Burns JL, Rolain JM. Culture-based diagnostic microbiology in cystic fibrosis: can we simplify the complexity? J Cyst Fibros Off J Eur Cyst Fibros Soc. 2014;13(1):1–9. doi:10.1016/j.jcf.2013.09.004.
O’Sullivan BP, Freedman SD. Cystic fibrosis. Lancet. 2009;373(9678):1891–904. doi:10.1016/S0140-6736(09)60327-5.
Horre R, Marklein G, Siekmeier R, Reiffert SM. Detection of hyphomycetes in the upper respiratory tract of patients with cystic fibrosis. Mycoses. 2011;54(6):514–22. doi:10.1111/j.1439-0507.2010.01897.x.
Pihet M, Carrere J, Cimon B, Chabasse D, Delhaes L, Symoens F, et al. Occurrence and relevance of filamentous fungi in respiratory secretions of patients with cystic fibrosis—a review. Med Mycol. 2009;47(4):387–97. doi:10.1080/13693780802609604.
Cimon B, Carrere J, Vinatier JF, Chazalette JP, Chabasse D, Bouchara JP. Clinical significance of Scedosporium apiospermum in patients with cystic fibrosis. Eur J Clin Microbiol Infect Dis Off Publ Eur Soc Clin Microbiol. 2000;19(1):53–6.
Morio F, Horeau-Langlard D, Gay-Andrieu F, Talarmin JP, Haloun A, Treilhaud M, et al. Disseminated Scedosporium/Pseudallescheria infection after double-lung transplantation in patients with cystic fibrosis. J Clin Microbiol. 2010;48(5):1978–82. doi:10.1128/JCM.01840-09.
Luijk B, Ekkelenkamp MB, De Jong PA, Kwakkel-van Erp JM, Grutters JC, van Kessel DA, et al. Effective prolonged therapy with voriconazole in a lung transplant recipient with Spondylodiscitis induced by Scedosporium apiospermum. Case Rep Infect Dis. 2011;2011:460313. doi:10.1155/2011/460313.
Musk M, Chambers D, Chin W, Murray R, Gabbay E. Successful treatment of disseminated scedosporium infection in 2 lung transplant recipients: review of the literature and recommendations for management. J Heart Lung Transplant Off Publ Int Soc Heart Transplant. 2006;25(10):1268–72. doi:10.1016/j.healun.2006.06.002.
Rolfe NE, Haddad TJ, Wills TS. Management of Scedosporium apiospermum in a pre- and post-lung transplant patient with cystic fibrosis. Med Mycol Case Rep. 2013;2:37–9. doi:10.1016/j.mmcr.2013.01.002.
Blyth CC, Harun A, Middleton PG, Sleiman S, Lee O, Sorrell TC, et al. Detection of occult Scedosporium species in respiratory tract specimens from patients with cystic fibrosis by use of selective media. J Clin Microbiol. 2010;48(1):314–6. doi:10.1128/JCM.01470-09.
Sayah DM, Schwartz BS, Kukreja J, Singer JP, Golden JA, Leard LE. Scedosporium prolificans pericarditis and mycotic aortic aneurysm in a lung transplant recipient receiving voriconazole prophylaxis. Transplant Infectious Dis Off J Transplant Soc. 2013;15(2):E70–4. doi:10.1111/tid.12056.
Badiee P, Alborzi A. Invasive fungal infections in renal transplant recipients. Exp Clin Transplant Off J Middle East Soc Organ Transplant. 2011;9(6):355–62.
Shoham S, Marr KA. Invasive fungal infections in solid organ transplant recipients. Future Microbiol. 2012;7(5):639–55. doi:10.2217/fmb.12.28.
Pappas PG, Alexander BD, Andes DR, Hadley S, Kauffman CA, Freifeld A, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin Infect Dis. 2010;50(8):1101–11. doi:10.1086/651262.
Larbcharoensub N, Chongtrakool P, Wirojtananugoon C, Watcharananan SP, Sumethkul V, Boongird A, et al. Treatment of a brain abscess caused by Scedosporium apiospermum and Phaeoacremonium parasiticum in a renal transplant recipient. Southeast Asian J Trop Med Public health. 2013;44(3):484–9.
Tamm M, Malouf M, Glanville A. Pulmonary scedosporium infection following lung transplantation. Transplant Infect Dis Off J Transplant Soc. 2001;3(4):189–94.
Maslen M, Peel M. Human and animal isolates of Pseudallescheria boydii and Scedosporium species, from Melbourne, Australia, 1977–1995. Mycoses. 2011;54(5):442–9. doi:10.1111/j.1439-0507.2010.01875.x.
Tammer I, Tintelnot K, Braun-Dullaeus RC, Mawrin C, Scherlach C, Schluter D, et al. Infections due to Pseudallescheria/Scedosporium species in patients with advanced HIV disease—a diagnostic and therapeutic challenge. Int J Infect Dis. 2011;15(6):e422–9. doi:10.1016/j.ijid.2011.03.004.
Jabado N, Casanova JL, Haddad E, Dulieu F, Fournet JC, Dupont B, et al. Invasive pulmonary infection due to Scedosporium apiospermum in two children with chronic granulomatous disease. Clin Infect Dis. 1998;27(6):1437–41.
Gompels MM, Bethune CA, Jackson G, Spickett GP. Scedosporium apiospermum in chronic granulomatous disease treated with an HLA matched bone marrow transplant. J Clin Pathol. 2002;55(10):784–6.
Santos PE, Oleastro M, Galicchio M, Zelazko M. Fungal infections in paediatric patients with chronic granulomatous disease. Rev Iberoam Micol. 2000;17(1):6–9.
Katragkou A, Dotis J, Kotsiou M, Tamiolaki M, Roilides E. Scedosporium apiospermum infection after near-drowning. Mycoses. 2007;50(5):412–21. doi:10.1111/j.1439-0507.2007.01388.x.
Buzina W, Feierl G, Haas D, Reinthaler FF, Holl A, Kleinert R, et al. Lethal brain abscess due to the fungus Scedosporium apiospermum (teleomorph Pseudallescheria boydii) after a near-drowning incident: case report and review of the literature. Med Mycol. 2006;44(5):473–7. doi:10.1080/13693780600654588.
Angelini A, Drago G, Ruggieri P. Post-tsunami primary Scedosporium apiospermum osteomyelitis of the knee in an immunocompetent patient. Int J Infect Dis. 2013;17(8):e646–9. doi:10.1016/j.ijid.2013.02.011.
Kim SH, Ha YE, Youn JC, Park JS, Sung H, Kim MN, et al. Fatal scedosporiosis in multiple solid organ allografts transmitted from a nearly-drowned donor. Am J Transplant Off J Am Soc Transplant Am Soc Transplant Surg. 2015;15(3):833–40. doi:10.1111/ajt.13008.
McGinnis MR, Fader RC. Mycetoma: a contemporary concept. Infect Dis Clin N Am. 1988;2(4):939–54.
Gammel JA. The etiology of maduromycosis: with a mycologic report on two new species observed in the United States. Arch Dermatol Syphilol. 1927;15(3):241–84.
Gulati V, Bakare S, Tibrewal S, Ismail N, Sayani J, Baghla DP. A rare presentation of concurrent Scedosporium apiospermum and Madurella grisea Eumycetoma in an immunocompetent host. Case reports Pathol. 2012;2012:154201. doi:10.1155/2012/154201.
Pistono PG, Rapetti I, Stacchini E, Guasco C. Clinical case of mycetoma caused by Scedosporium apiospermum. G Batteriol Virol Immunol. 1989;82(1–12):88–91.
Wethered DB, Markey MA, Hay RJ, Mahgoub ES, Gumaa SA. Ultrastructural and immunogenic changes in the formation of mycetoma grains. J Med Vet Mycol Bi-monthly Publ Int Soc Human Anim Mycol. 1987;25(1):39–46.
Studahl M, Backteman T, Stalhammar F, Chryssanthou E, Petrini B. Bone and joint infection after traumatic implantation of Scedosporium prolificans treated with voriconazole and surgery. Acta Paediatr. 2003;92(8):980–2.
Hell M, Neureiter J, Wojna A, Presterl E, Willinger B, de Hoog GS, et al. Post-traumatic Pseudallescheria apiosperma osteomyelitis: positive outcome of a young immunocompetent male patient due to surgical intervention and voriconazole therapy. Mycoses. 2011;54 Suppl 3:43–7. doi:10.1111/j.1439-0507.2011.02106.x.
Tirado-Miranda R, Solera-Santos J, Brasero JC, Haro-Estarriol M, Cascales-Sanchez P, Igualada JB. Septic arthritis due to Scedosporium apiospermum: case report and review. J Infect. 2001;43(3):210–2. doi:10.1053/jinf.2001.0866.
Le Gouill S, Morineau N, Miegeville M, Milpied N, Harousseau J, Moreau P. Pseudallescheria boydii osteoarthritis in a patient with acute lymphoblastic leukemia: a case report. La Revue de Medecine interne/fondee par la Societe nationale francaise de medecine interne. 1999;20(5):434–8.
Lackner M, De Man FH, Eygendaal D, Wintermans RG, Kluytmans JA, Klaassen CH, et al. Severe prosthetic joint infection in an immunocompetent male patient due to a therapy refractory Pseudallescheria apiosperma. Mycoses. 2011;54 Suppl 3:22–7. doi:10.1111/j.1439-0507.2011.02107.x.
Figueroa MS, Fortun J, Clement A, De Arevalo BF. Endogenous endophthalmitis caused by Scedosporium apiospermum treated with voriconazole. Retina. 2004;24(2):319–20.
McKelvie PA, Wong EY, Chow LP, Hall AJ. Scedosporium endophthalmitis: two fatal disseminated cases of Scedosporium infection presenting with endophthalmitis. Clin Exp Ophthalmol. 2001;29(5):330–4.
Guerrero A, Torres P, Duran MT, Ruiz-Diez B, Rosales M, Rodriguez-Tudela JL. Airborne outbreak of nosocomial Scedosporium prolificans infection. Lancet. 2001;357(9264):1267–8. doi:10.1016/S0140-6736(00)04423-8.
Alvarez M, Lopez Ponga B, Rayon C, Garcia Gala J, Roson Porto MC, Gonzalez M, et al. Nosocomial outbreak caused by Scedosporium prolificans (inflatum): four fatal cases in leukemic patients. J Clin Microbiol. 1995;33(12):3290–5.
Lamaris GA, Chamilos G, Lewis RE, Safdar A, Raad II, Kontoyiannis DP. Scedosporium infection in a tertiary care cancer center: a review of 25 cases from 1989–2006. Clin Infect Dis. 2006;43(12):1580–4. doi:10.1086/509579.
Park BJ, Pappas PG, Wannemuehler KA, Alexander BD, Anaissie EJ, Andes DR, et al. Invasive non-Aspergillus mold infections in transplant recipients, United States, 2001–2006. Emerg Infect Dis. 2011;17(10):1855–64. doi:10.3201/eid1710.110087. A multi-centre study from the USA that evaluated epidemiology and outcomes of solid organ and haematopoeitic stem cell transplant patients with non-aspergillus invasive mould infection, whereby Scedosporium species accounted for 16% of all infections.
Acknowledgments
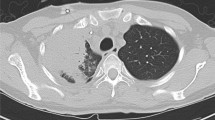
We thank Dr. Sarah Kidd for permission to reproduce Fig. 1a from www.mycologyonline.edu.au/
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
The authors declare that they have no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Epidemiology of Fungal Infections
Rights and permissions
About this article
Cite this article
Subedi, S., Chen, S.CA. Epidemiology of Scedosporiosis. Curr Fungal Infect Rep 9, 275–284 (2015). https://doi.org/10.1007/s12281-015-0243-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-015-0243-0