Abstract
Organophosphate (OP) intoxication remains a serious worldwide health concern, and many patients with acute OP intoxication have also consumed alcohol. Therefore, we evaluated the association of blood alcohol concentration (BAC) with mortality among patients with OP intoxication. We retrospectively reviewed records from 135 patients who were admitted to an emergency department (ED) for OP intoxication between January 2000 and December 2012. Factors that were associated with patient survival were identified via receiver operating characteristic curve, multiple logistic regression, and Kaplan–Meier survival analyses. Among 135 patients with acute OP poisoning, 112 patients survived (overall mortality rate: 17 %). The non-survivors also exhibited a significantly higher BAC, compared to the survivors [non-survivors: 192 mg/dL, interquartile range (IQR) 97–263 mg/dL vs. survivors: 80 mg/dL, IQR 0–166.75 mg/dL; p < 0.001]. A BAC cut-off value of 173 mg/dL provided an area under the curve of 0.744 [95 % confidence interval (CI) 0.661–0.815], a sensitivity of 65.2 %, and a specificity of 81.2 %. A BAC of >173 mg/dL was associated with a significantly increased risk of 6-month mortality in the multiple logistic regression model (odds ratio 4.92, 95 % CI 1.45–16.67, p = 0.001). The Cox proportional hazard model revealed that a BAC of >173 mg/dL provided a hazard ratio of 3.07 (95 % CI 1.19–7.96, p = 0.021). A BAC of >173 mg/dL is a risk factor for mortality among patients with OP intoxication.
Similar content being viewed by others
Introduction
Organophosphates (OPs) are found in pesticides, garden sheds, surface and room sprays, baits for cockroaches and other insects, and shampoos that target head lice [1]. Unfortunately, >873,000 people die every year due to OP poisoning, with a worldwide overall mortality rate of 15–30 % [2, 3], Therefore, it is important to identify the factors that are related to the deaths of these individuals.
OPs exert their acute toxicity by inhibiting cholinesterases, which include acetylcholinesterase (AChE) and butyrylcholinesterase, and cause symptoms that include anxiety, miosis, increased bronchial and tear secretion, and bradycardia [4]. In serious cases, OP poisoning may cause death via respiratory failure and shock, and requires rapid intervention and admission to an intensive care unit [3]. Respiratory failure occurs in 43 % of patients with OP poisoning [5], and Grmec et al. report that respiratory failure often occurs in patients with a reduced level of consciousness [6]. Furthermore, the prognosis of patients with OP intoxication is predicted by their Acute Physiology and Chronic Health Evaluation II (APACHE II) score, vital signs, white blood cell count, pH, serum creatinine levels, and Glasgow coma scale (GCS) score [7].
Interestingly, many poisoning deaths among Asian patients involve the co-ingestion of alcohol [8]. Our clinical experience also suggests that alcohol intoxication complicates the management of patients with OP intoxication, which may occur via exacerbation of the OP’s suppressive effects on the patient’s level of consciousness and respiratory drive. Eddleston et al. report a significant association between blood alcohol concentration (BAC) and serum levels of dimethoate, which is a type of OP [9]. However, to the best of our knowledge, no studies have examined the influence of BAC on the mortality rate after OP poisoning. Therefore, we designed the present study to examine the association of BAC with survival among patients who were admitted to an ED for OP poisoning. Because OP insecticide, being lipophilic, may accumulate in various tissues and organs after poisoning, and subsequently, be released into the bloodstream, chronic tissue damage due to oxidation and inflammation and neurologic sequelae can occur, which can increase the long-term mortality risk. The study by Huang et al. also shows an increase in mortality for up to 6 months [10]. Therefore, 6-month mortality was used as the primary outcome in this study.
Methods
Study design
This retrospective cohort study examined patients with OP poisoning who were admitted to 5 EDs in the Republic of Korea between January 2000 and December 2012. We identified cases of OP poisoning via a poisoning registry, and only included registered patients who were poisoned with a single OP agent. This study’s design was approved by the institutional ethics committees of our hospitals.
Subject and data collection
We retrospectively examined data in handwritten charts and electronic medical records from cases of acute OP poisoning, which was defined based on the history of exposure to a single OP agent. The exclusion criteria were age of <18 years, an unclear history of exposure, multiple drug exposures, the presence of terminal malignancy, and missing data. Data regarding the patients’ general characteristics included age, gender, vital signs, volume of poison, reason for poisoning, APACHE II score, intubation in the ED, and GCS score. The GCS score evaluates coma severity based on ocular, verbal, and motor criteria (mild: GCS of 14–15; moderate: GCS of 9–13; severe: GCS of 3–8) [11], and is used by clinicians to rapidly identify cases of severe OP poisoning in the ED [12]. The ingested amount of liquid OP was calculated via the number of mouthfuls that were ingested (1 mouthful = 20 mL), as recalled by the patient or as calculated from the remaining amount in the chemical bottle [13].
Laboratory results regarding pH, arterial gases (PaCO2, PaO2, HCO3, and O2 saturation) and the levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), blood urea nitrogen (BUN), creatinine, amylase, and arterial lactate were evaluated using blood samples that were obtained at the time of admission. The same blood samples were also used to measure BAC and serum cholinesterase concentrations.
Blood alcohol measurement via gas chromatography
BAC was measured via chromatography using a Dimension Vista® 1500 System (Siemens, Munich, Germany).
Pseudocholinesterase levels and poisoning severity
OP poisoning is generally confirmed via a reduction in pseudocholinesterase (serum cholinesterase, SChE) activity, which is an enzyme that is present in the bloodstream and hydrolyzes acetylcholine less rapidly than AChE [14]. Blood cholinesterase concentration was measured via pseudocholinesterase activity using a colorimetric assay, and the Dimension Vista® 1500 System was used for the absorption measurements. Each hospital independently conducted the assay. Based on the measured serum levels, the severity of poisoning was defined using the Namba classification: poisoning (Namba I: no clinical manifestation, SChE reduced to 90–50 % of normal), mild poisoning (Namba II: fatigue, headache, nausea and vomiting, abdominal pain, diarrhea, excessive sweating and salivation, and SChE reduced to 50–20 % of normal), moderate poisoning (Namba III: generalized weakness, difficulty in speech, muscular fasciculations, miosis, and SChE reduced to 20–10 % of normal), and severe poisoning (Namba IV: unconsciousness, pinpoint pupils and loss of light reflex, muscular fasciculations, secretions from the mouth and nose, rales in the lungs, respiratory difficulty, and SChE reduced to <10 % of normal) [15–21].
Data analysis
Two emergency medical technicians (EMTs) blindly reviewed the charts. Patients were divided into two groups: survivors and non-survivors at 6 months. Continuous variables were expressed as mean ± standard deviation or median with interquartile range (IQR). Categorical data were reported as percentage. Differences between the survivor and non-survivor groups were evaluated using the independent two sample t test, the Mann–Whitney U test, the Chi-square test, or Fisher’s exact test. Differences with a p value of <0.05 were considered statistically significant, and variables with a p value of <0.05 in the univariate analyses were evaluated for potential multicollinearity. Next, the continuous variables were dichotomized according to cut-off points that were determined via receiver operating characteristic (ROC) curve analyses, and then incorporated into the logistic model. For the multiple logistic regression analysis, we included arterial pH, lactate, HCO3, BAC, APACHE II score, GCS score, intubation in the ED, and ingested amount of OP. Survival curves were generated using the Kaplan–Meier method and compared using the log-rank test. A Cox proportional hazards model was used to estimate the adjusted hazard ratio (HR), and the adjusted odds ratios (OR) and hazard ratios (HR) with 95 % confidence intervals (95 % CI) were calculated to evaluate the relationship between the covariates and outcomes. Analyses were performed using SPSS software (version 18.0; SPSS Inc., Chicago, Ill, USA), MedCalc software (version 11.6; MedCalc Ltd., Mariakerke, Belgium), or SAS software (version 9.1; SAS Inc., Cary, NC, USA).
Results
Between January 2000 and December 2012, 171 patients were admitted to the five participating EDs with OP poisoning. Hospital A is an urban hospital, which admits 80,000 patients to the ED annually. Out of 85 patients, only 71 patients were included in the study, after the exclusion of 14 patients. Hospital B, as an urban hospital, admits 35,000 patients to the ED annually. Out of 46 patients, 8 were excluded, and only 38 patients were included in the study. Hospital C, as an urban hospital, admits 75,000 patients to the ED annually. Out of 19 patients, only 11 patients were included, after the exclusion of 8 patients. Hospital D, as an urban hospital, admits 95,000 patients to the ED annually. Out of 12 patients, only 9 patients were included, after the exclusion of 3 patients. Hospital E is an urban hospital and admits 45,000 patients to the ED annually. Out of 9 patients, only 6 patients were included, after the exclusion of 3 patients. There were no statistically significant differences in demographic characteristics among the hospitals. We excluded 6 patients for being <18 years old, 12 patients due to an unclear history of exposure, 10 patients due to multiple drug exposures, 2 patients due to a history of terminal malignancy, and 6 patients due to missing data. Therefore, the medical records from 135 patients were included in the final analyses (Fig. 1).
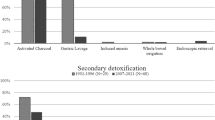
Table 1 shows the general characteristics of the survivors and non-survivors of acute OP poisoning. Among the 135 included patients, 112 patients survived (an overall survival rate of 83 %). The patients were generally middle-aged (range 42–71 years) with a normal body temperature and slightly elevated MAP, heart rate, and respiratory rate. Most patients had ingested the pesticide during a suicide attempt, and treatment using gastric emptying or activated charcoal did not affect their chances of survival. Compared to the survivor group, the non-survivor group had ingested a threefold greater volume of OP (100 vs. 300 mL, p < 0.001). In the non-survivor group, 65.2 % of the patients were diagnosed with decreased levels of consciousness (a GCS of <8), compared to only 17 % in the survivor group (p <0.001). The APACHE II scores were modestly but significantly associated with survival (p = 0.019). Intubation in the ED was observed for 60.7 % of the patients in the survivor group and 82.6 % of the patients in the non-survivor group (p = 0.046).
Laboratory analyses revealed that the patients who died due to OP poisoning had a twofold greater BAC, compared to the survivors (median 192 mg/dL, IQR 97–263 mg/dL vs. median 80 mg/dL, IQR 0–166.75 mg/dL; p < 0.001 (Table 2). Survival was also associated with higher blood pH and HCO3 levels, and with lower levels of lactate. However, survival was not associated with the enzyme markers of liver (AST, ALT), pancreas (amylase), or kidney (BUN and creatinine) function. In addition, the absence of an association between survival and the blood gases was consistent with the near normal cardiac and respiratory functions of the patients in both groups.
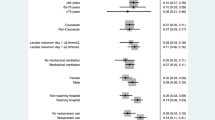
Multiple regression analysis was performed using a model that included all factors that were significant in the univariate analyses (Tables 1, 2). The only factors that were associated with a significantly higher risk of death were a BAC of >173 mg/dL (OR 4.92, 95 % CI 1.45–16.67, p = 0.01) and ingested amount of OP (OR 10.23, 95 % CI 1.16–90.01, p = 0.04) (Table 3). Furthermore, the ingested amount of OP was significantly correlated with BAC (Spearman’s ρ = 0.548; p < 0.001) (Fig. 2). The ROC curve analysis for BAC indicated that a cut-off value of 173 mg/dL provided an area under the ROC curve of 0.744 (95 % CI 0.661–0.815), a sensitivity of 65.2 %, and a specificity of 81.2 % (Fig. 3). We also constructed Kaplan–Meier curves for the survivor and non-survivor groups at 6 months after their admission (Fig. 4). Cox regression analyses revealed that the hazard ratio for a BAC of >173 mg/dL was 3.07 (95 % CI 1.19–7.96, p = 0.021).
Kaplan–Meier survival analysis after organophosphate poisoning according to alcohol consumption. The survival probabilities calculated for the high BAC (>173 mg/dL) (dashed line) and low BAC (solid lines) groups up to 6 months after the poisoning even. The log-rank test reveals a significant difference between the two groups (p < 0.01), and the hazard ratio for a blood alcohol concentration of >173 mg/dL is 3.07 (95 % confidence interval 1.19–7.96, p = 0.021) using the Cox proportional hazard model
Discussion
In the present study, we find that a BAC of >173 mg/dL is a significant risk factor for OP poisoning related mortality. In this context, OPs inhibit AChE, which converts acetylcholine into choline and acetic acid in the cholinergic synapses. Furthermore, AChE is present in the central nervous system, peripheral nervous system, neuromuscular junction, and erythrocytes. Therefore, poisoning with AChE inhibitors (e.g. OPs) leads to overstimulation of both the nicotinic and muscarinic receptors [22]. Muscarinic stimulation causes defecation, urination, miosis, bradycardia, bronchorrhea, bronchospasm, emesis, lacrimation, and salivation. Moreover, stimulation of the nicotinic receptors in the sympathetic ganglia and neuromuscular junction causes mydriasis, tachycardia, weakness, hypertension, and fasciculations [23]. The effects on the central nervous system (CNS) include headache, dizziness, restless, anxiety, insomnia, confusion, tremor, dysarthria, ataxia, seizures, coma, and central respiratory depression [24].
Eddleston et al. report that a high BAC at admission is associated with high OP concentrations, which is probably due to larger ingestion volumes [9]. Furthermore, after adjusting for gender and age, they report that the alcohol ingestion group exhibits a fourfold higher mortality rate, although the increased risk of death is not significant after controlling for dimethoate use (OR 0.3, 95 % CI 0.0–8.8). In contrast, our findings reveal that the survivors exhibit a significantly lower median BAC, compared to that among the non-survivors (80 vs. 192 mg/dL; p < 0.001), and BAC is significantly correlated with the ingested amount of OP (Spearman’s ρ = 0.548). Interestingly, our non-survivor group exhibits a twofold greater BAC, compared to the non-survivors in Eddleston et al.’s study, although the two survivor groups exhibit similar BACs. These findings indicate that the overall BAC is relatively high in the present study, which motivated us to identify the optimal cut-off value for BAC in predicting mortality risk (173 mg/dL).
Respiratory depression is one of the leading causes of death due to acute intoxication [25, 26], and alcohol is one of the most commonly abused drugs that can induce respiratory failure. Among adults, respiratory failure can occur in a dose-dependent fashion, as ethanol affects the respiratory center in the medulla oblongata [27]. Furthermore, Adinoff et al. report that a BAC as low as 100 mg/dL can significantly affect adolescents and alcohol-naive adults, and can induce severe toxicities [28]. Moreover, our optimal cut-off for BAC (173 mg/dL) is sufficient to negatively affect an individual’s consciousness. In Eddleston et al.’s study, the effect of alcohol was abolished by controlling for the use of dimethoate. Nevertheless, by controlling for other factors (including amount), our findings reveal that a higher BAC (>173 mg/dL) is associated with a three- to fourfold higher risk of 6-month mortality (OR 4.92, 95 % CI 1.45–16.67; HR 3.07, 95 % CI 1.19–7.96). There are two possible explanations for this discrepancy. First, the overall BAC is higher in the present study, compared to the findings of Eddleston et al., and this higher BAC may have aggravated the effects of OP on the CNS, which might increase CNS depression and lead to respiratory failure [6, 29]. Interestingly, we found that the non-survivor group has a greater decrease in their level of consciousness, and requires more frequent intubation, compared to the survivor group. Second, Eddleston et al. included all patients who had consumed alcohol in the alcohol ingestion group, regardless of the absolute amount that was consumed. Thus, it is possible that their results were underestimated due to the inclusion of patients with a very low BAC, which might limit the adverse effects of alcohol ingestion. In contrast, we categorized patients into low and high levels of alcohol ingestion, to examine the association of ingesting a large amount of alcohol with the patient’s survival.
In this study, 8 patients died >15 days after exposure to OP; OPs cause vomiting, increased secretions, loss of consciousness, and loss of airway protection. Patients can also aspirate after gastric lavage or forced emesis [30]. Aspiration increases length of hospital stay, morbidity. Aspiration pneumonia was reported in 82 % (27/33) of OP insecticide–poisoned patients admitted to a German ICU [31]. Our eight patients were treated with a ventilator and had severe aspiration pneumonia. All of these patients failed to wean from the ventilator and all deceased patients had severe respiratory muscle weakness. OP-induced delayed polyneuropathy can cause respiratory failure through phrenic nerve involvement [32]. This may explain why our patients failed to wean from the ventilator and died after 15 days.
This study has several limitations that warrant consideration when interpreting our findings. First, the ingested amount of OP may not be entirely accurate, as the amount for each case was calculated based on the patient’s recall or the volume that remained in the container. Second, the sample size was relatively small, despite the fact that we included patients from five separate EDs. Nevertheless, this study provides useful data, as our findings reveal that a BAC of >173 mg/dL can negatively affect the long-term survival rate among patients with OP intoxication. Third, this study was a retrospective study, and instruments that can measure the OP concentration were not available at the five institutions participating in this study.
Conclusion
In conclusion, our results reveal that a BAC of >173 mg/dL during OP poisoning is a major risk factor for mortality among patients with OP intoxication.
References
Roberts DM, Aaron CK (2007) Management of acute organophosphorus pesticide poisoning. BMJ 334(7594):629–634
Gunnell D, Eddleston M, Phillips MR, Konradsen F (2007) The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health 7:357 (Epub 2007/12/25)
Eddleston M, Buckley NA, Eyer P, Dawson AH (2008) Management of acute organophosphorus pesticide poisoning. Lancet 371(9612):597–607 (Epub 2007/08/21)
Kwong TC (2002) Organophosphate pesticides: biochemistry and clinical toxicology. Ther Drug Monit 24(1):144–149 (Epub 2002/01/24)
Tsao TC, Juang YC, Lan RS, Shieh WB, Lee CH (1990) Respiratory failure of acute organophosphate and carbamate poisoning. Chest 98(3):631–636
Grmec S, Mally S, Klemen P (2004) Glasgow Coma Scale score and QTc interval in the prognosis of organophosphate poisoning. Acad Emerg Med 11(9):925–930
Ke X, Zhi S, Zheng D, Hong G, Zhao G, Li M et al (2015) Analyses on relevant factors of the prognosis of patients with acute organophosphate poisoning. Zhonghua lao dong wei sheng zhi ye bing za zhi = Zhonghua laodong weisheng zhiyebing zazhi. Chin J Indus Hygiene Occup Dis 33(3):186–189 (Epub 2015/04/29)
van der Hoek W, Konradsen F (2005) Risk factors for acute pesticide poisoning in Sri Lanka. Trop Med Int Health 10(6):589–596 (Epub 2005/06/09)
Eddleston M, Gunnell D, von Meyer L, Eyer P (2009) Relationship between blood alcohol concentration on admission and outcome in dimethoate organophosphorus self-poisoning. Br J Clin Pharmacol 68(6):916–919
Huang HS, Hsu CC, Weng SF, Lin HJ, Wang JJ, Su SB et al (2015) Acute anticholinesterase pesticide poisoning caused a long-term mortality increase: a nationwide population-based cohort study. Medicine 94(30):e1222 (Epub 2015/07/30)
Mena JH, Sanchez AI, Rubiano AM, Peitzman AB, Sperry JL, Gutierrez MI et al (2011) Effect of the modified Glasgow Coma Scale Score criteria for mild traumatic brain injury on mortality prediction: comparing classic and modified Glasgow Coma Scale Score Model Scores of 13. J Trauma 71(5):1185–1193
Akdur O, Durukan P, Ozkan S, Avsarogullari L, Vardar A, Kavalci C et al (2010) Poisoning severity score, Glasgow coma scale, corrected QT interval in acute organophosphate poisoning. Hum Exp Toxicol 29(5):419–425
Lee J-W, Hwang I-W, Kim J-W, Moon H-J, Kim K-H, Park S et al (2015) Common pesticides used in suicide attempts following the 2012 Paraquat Ban in Korea. J Korean Med Sci 30(10):1517–1521
Chaudhary SC, Singh K, Sawlani KK, Jain N, Vaish AK, Atam V et al (2013) Prognostic significance of estimation of pseudocholinesterase activity and role of pralidoxime therapy in organophosphorous poisoning. Toxicol Int 20(3):214–217
Namba T, Nolte CT, Jackrel J, Grob D (1971) Poisoning due to organophosphate insecticides: acute and chronic manifestations. Am J Med 50(4):475–492
Chuang FR, Jang SW, Lin JL, Chern MS, Chen JB, Hsu KT (1996) QTc prolongation indicates a poor prognosis in patients with organophosphate poisoning. Am J Emerg Med 14(5):451–453 (Epub 1996/09/01)
Yilmazlar A, Ozyurt G (1997) Brain involvement in organophosphate poisoning. Environ Res 74(2):104–109 (Epub 1997/01/01)
Oh BJ, Hwang SO, Lee KH, Hong ES, Lim JC, Kim H et al (1998) Different clinical features of organophosphate insecticides intoxication according to the route of administration: disparity between clinical severity and plasma cholinesterase level. J Korean Soc Emerg Med 9(1):135–141
Khan S, Hemalatha R, Jeyaseelan L, Oommen A, Zachariah A (2001) Neuroparalysis and oxime efficacy in organophosphate poisoning: a study of butyryicholinesterase. Hum Exp Toxicol 20(4):169–174
Özyurt G, Bilgin H, Kutsal MG (2003) Atropine aerosol spray (AAS) by nasal application in organophosphate poisoning. J Med Chem Def 1:1–10
Cha Y, Kim H, Go J, Kim T, Kim O, Cha K et al (2014) Features of myocardial injury in severe organophosphate poisoning. Clin Toxicol 52(8):873–879
Chowdhary S, Bhattacharyya R, Banerjee D (2014) Acute organophosphorus poisoning. Clin Chim Acta 431:66–76
King AM, Aaron CK (2015) Organophosphate and carbamate poisoning. Emerg Med Clin North Am 33(1):133–151 (Epub 2014/12/03)
Asari Y, Kamijyo Y, Soma K (2004) Changes in the hemodynamic state of patients with acute lethal organophosphate poisoning. Vet Hum Toxicol 46(1):5–9 (Epub 2004/01/30)
Centers for Disease Control and Prevention (CDC) (2011) Drug overdose deaths–Florida, 2003–2009. MMWR. Morb Mortal Wkly Rep 60(26):869–872 (Epub 2011/07/08)
Paulozzi LJ, Centers for Disease Control and Prevention (CDC) (2011) Drug-induced deaths—United States, 2003–2007. Morbidity and mortality weekly report Surveillance summaries (Washington, DC: 2002) 60(Suppl 60–61) (Epub 2011/03/25)
Wilson KC, Saukkonen JJ (2004) Acute respiratory failure from abused substances. J Intensive Care Med 19(4):183–193
Adinoff B, Bone GH, Linnoila M (1988) Acute ethanol poisoning and the ethanol withdrawal syndrome. Med Toxicol Adverse Drug Exp 3(3):172–196
Eizadi-Mood N, Saghaei M, Alfred S, Zargarzadeh AH, Huynh C, Gheshlaghi F et al (2009) Comparative evaluation of Glasgow Coma Score and gag reflex in predicting aspiration pneumonitis in acute poisoning. J Crit Care 24(3):470 e9–15 (Epub 2009/03/31)
Eddleston M, Haggalla S, Reginald K, Sudarshan K, Senthilkumaran M, Karalliedde L et al (2007) The hazards of gastric lavage for intentional self-poisoning in a resource poor location. Clin Toxicol 45(2):136–143 (Epub 2007/03/17)
Hrabetz H, Thiermann H, Felgenhauer N, Zilker T, Haller B, Nahrig J et al (2013) Organophosphate poisoning in the developed world—a single centre experience from here to the millennium. Chem Biol Interact 206(3):561–568 (Epub 2013/05/21)
Rivett K, Potgieter PD (1987) Diaphragmatic paralysis after organophosphate poisoning. A case report. S Afr Med J = Suid-Afrikaanse tydskrif vir geneeskunde 72(12):881–882 (Epub 1987/12/19)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human and animal rights
This study was approved by the institutional review board (CR315049-002).
Informed consent
No informed consent since it was a retrospective observational study.
Additional information
Young Hwan Lee and Young Taeck Oh equally contributed.
Rights and permissions
About this article
Cite this article
Lee, Y.H., Oh, Y.T., Lee, W.W. et al. The association of alcohol consumption with patient survival after organophosphate poisoning: a multicenter retrospective study. Intern Emerg Med 12, 519–526 (2017). https://doi.org/10.1007/s11739-016-1484-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11739-016-1484-9