Abstract
The purpose of the present study is to introduce a novel methodology for adapting and upgrading decision-making strategies concerning mechanical ventilation with respect to different disease states into our fuzzy-based expert system, AUTOPILOT-BT. The special features are: (1) Extraction of clinical knowledge in analogy to the daily routine. (2) An automated process to obtain the required information and to create fuzzy sets. (3) The controller employs the derived fuzzy rules to achieve the desired ventilation status. For demonstration this study focuses exclusively on the control of arterial CO2 partial pressure (paCO2). Clinical knowledge from 61 anesthesiologists was acquired using a questionnaire from which different disease-specific fuzzy sets were generated to control paCO2. For both, patients with healthy lung and with acute respiratory distress syndrome (ARDS) the fuzzy sets show different shapes. The fuzzy set “normal”, i.e., “target paCO2 area”, ranges from 35 to 39 mmHg for healthy lungs and from 39 to 43 mmHg for ARDS lungs. With the new fuzzy sets our AUTOPILOT-BT reaches the target paCO2 within maximal three consecutive changes of ventilator settings. Thus, clinical knowledge can be extended, updated, and the resulting mechanical ventilation therapies can be individually adapted, analyzed, and evaluated.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
1 Introduction
Any decision in mechanical ventilation therapy is based on the analysis of several physiological parameters (e.g., paO2, paCO2), a collection of clinical facts, statistical data, physiologic cause-and-effect relationships and human experience [2]. While it is the task of the physician to obtain a rational understanding by finding a relation between all these knowledge sources and modalities, it is the task of the engineer to translate the medical expert’s knowledge into the language of control engineering. For quite some years knowledge engineers have been trying to acquire, aggregate and represent expert knowledge in the field of mechanical ventilation management in intensive care medicine in order to standardize respiratory therapy [9, 20, 21, 23–25]. For most of these knowledge-based systems, clinical experts generate sets of objectives (set-point values), sets of ventilator settings and rules to connect the two sets [4]. In the 1980s first rule-based systems for mechanical ventilation therapy were developed [25]. In 1989 an expert system called KUSIVAR was presented [18]. Its knowledge base included both qualitative rule-based knowledge and quantitative knowledge expressed by means of statistical models to predict patient responses to different ventilator settings. Dojat et al. designed in 1992 a knowledge-based system for the management of patients receiving respiratory support and implemented a weaning protocol. This system, called GANESH, was rule-based and used respiratory frequency, tidal volume and end-tidal CO2 concentration to ensure the “respiratory comfort” of the patient [5]. Additional studies about this approach were subsequently published [3, 6–8, 14].
Some knowledge-based systems incorporate imprecise controlling concepts like “if the patient is slightly hypoventilated, then increase the ventilatory frequency a bit” using fuzzy-logic: In 1994, Sun et al. introduced a fuzzy-control system for the adjustment of the inspiration oxygen fraction (FiO2). The controller utilizes set-points and rules provided by neonatologists [22]. Schäublin et al. [19] published the evaluation of another computerized rule-based system with fuzzy-logic in 1996. This fuzzy controller is based on recommendations of Kacmarek and Venegas [12] to achieve and maintain arterial partial pressure of carbon dioxide at a desired level (set-point) by changing respiratory rate and tidal volume. In 2003, Kwok et al. [13] introduced another rule-based system to adjust the FiO2 based on the current paO2 level. They evaluated the change of FiO2 settings advised by eight clinical experts responding to 71 clinical scenarios. Nemoto et al. [17] developed a fuzzy-logic-based approach to the automatic control of mechanical ventilation using the expert knowledge from a small number of clinical experts. All the systems mentioned above lack flexibility, because they use fixed rules exclusively implementing the clinical knowledge of some experts.
In 1985 Miller et al. [16] introduced a system, called VQ-ATTENDING, that evaluated ventilator settings proposed by clinicians. In a previous study from our group [15], it was corroborated that ventilator settings proposed by clinicians are mostly suboptimal with respect to precision and adaptation time to reach the optimal ventilation state. Tong suggested separating strategic knowledge about treatment goals from tactical knowledge about management options to reach those goals [26]. Advancing this latter approach, the AUTOPILOT-BT system leaves strategic decisions to the clinician but automatically realizes a disease specific, fast, and robust control on the “tactical” level. In consequence a knowledge-based therapy system was designed asking the intensivist exclusively two types of questions: (i) which are the physiological targets of the therapy, and (ii) which are the control parameters for reaching these physiological targets. The decision, when and how to change ventilator settings to reach those goals, is left to the control system of the AUTOPILOT-BT. “Optimal” may differ from intensive care unit to intensive care unit, even from intensivist to intensivist. Consequently, our control system is designed to be adaptive to: (1) the disease state and (2) personal therapeutic preferences of the intensivist or the therapeutic guidelines of an intensive care unit. This allows our system to be extended and individually adapted if required.
2 Methods
In the present study, knowledge acquisition for the fuzzy controller proceeded as follows: (i) 61 anesthesiologists of the University Medical Centre of Freiburg exclusively provided the desired disease-specific set-points for mechanical ventilation, (ii) these set-points were transferred into fuzzy membership functions, fuzzy rules were created and the output values were calculated so that the system obtained the capability to reach the desired set-point values within a few consecutive adaptations of ventilator settings. We have investigated a method how knowledge from clinical experts can be extracted in analogy to their daily clinical routine. Subsequently, the obtained expert knowledge can be translated automatically into a system of disease-specific set-point values and transformed into a fuzzy-logic-based control system.
The knowledge acquisition (and therefore the AUTOPILOT-BT system) is currently constrained to 5 different disease states: CCI (cranio cerebral injury), ARDS (acute respiratory distress syndrome), COPD (chronic obstructive pulmonary disease), fibrosis, and “healthy lung”. Five different respiratory parameters were employed to characterize the acute patient state: arterial carbon dioxide partial pressure (paCO2), arterial oxygen partial pressure (paO2), arterial oxygen saturation (SpO2), respiratory system compliance (Crs), and airway plateau pressure (Pplat).
In order to demonstrate the principles of this approach, we focus on the arterial carbon dioxide partial pressure (paCO2) and its control via closed-loop setting of the respiratory rate, both for patients without pulmonary disease (“healthy”) and for ARDS (acute respiratory distress syndrome) patients. During anaesthesia procedures, mechanical ventilation must be controlled continuously and adjusted in order to maintain parameters of gas exchange such as paCO2 in their physiologic or therapeutic range. This setting is corrected according to periodic measurements of arterial blood gas concentrations or by using capnometry, or both [19].
Figure 1 shows schematically the steps of the present study: The dotted labeling field represents the part where the intensivists were involved insofar as they classified given paCO2 values. With respect to the pulmonary status they decided if these values were adequate targets for a ventilation controller. Then the paCO2 set-points defined by the intensivists were translated into membership functions (fuzzification of the input). Afterwards fuzzy rules were defined, e.g., for the change of the respiratory rate to achieve a normal ventilation status. The fuzzy system with fuzzy inputs and fuzzy rules was implemented into the automatic control system AUTOPILOT-BT. The performance of the control system was evaluated with a physical lung model based on a passive mechanical lung simulator (Model 5600i, Michigan Instruments, Grand Rapids, MI) [15].
Progression of the study: (1) A questionnaire was used to acquire the desired set-points for the ventilation therapy from physicians. (2) A fuzzy system was created according to these set-points. (3) The new fuzzy system was implemented into the AUTOPILOT-BT system. (4) The system was evaluated in an experimental trial. (5) The results were reported
Figure 2 illustrates the design procedure from the acquisition of set-points for paCO2 as specified by the intensivists until fuzzification of the paCO2. (1) Using a specially developed questionnaire the paCO2 set-point values were acquired from intensivists with respect to pulmonary disease. (2) The results obtained from the questionnaires (n = 61) were evaluated using histograms. (3) Characteristic “defining points” were extracted to define the fuzzy membership functions. (4) Depending on those evaluations the shape of the membership function was determined and parameterized.
Design procedure of fuzzy sets based on clinical expert knowledge for ventilatory therapy of ARDS patients: (1) Knowledge acquisition: Questionnaire to acquire set-point values. (2) Generation of histograms: The histogram represents the distribution of the classified values over ventilation categories. The black dot displays the median of the distribution. (3) Extraction of “defining points”, which define the shape of the corresponding fuzzy set. (4) Definition of fuzzy sets: seven fuzzy sets representing seven ventilation states
2.1 Knowledge acquisition/Questionnaire
Whereas knowledge acquisition typically tries to query experts to formulate logical rules, we have interviewed 61 intensivists using a questionnaire by asking them to perform diagnostic evaluation as in daily clinical routine. The query was realized within the daily meeting with a time limit of 45 min. The questionnaire was distributed as hard copy with the intention that all 61 intensivists could answer the query simultaneously under supervision.
A given paCO2 value had to be assigned to a specific ventilation status of a hypothetical patient. The offered scale of the assignment ranged from “extreme hypoventilation” (left end of the scale) over “strong hypoventilation”, “moderate hypoventilation”, “normal ventilation”, “moderate hyperventilation”, “strong hyperventilation” until “extreme hyperventilation” (right end of the scale).
A time frame of 20 seconds was allotted to classify each given value by marking a position on the given scale with a vertical bar as shown in Fig. 2 part 1. To synchronize the clinicians each value to be classified was projected for this time frame on a screen by the supervisor. The questioning was repeated under consideration of different pulmonary disease states of the hypothetical patient. The questionnaire was unknown to the experts prior to the interview.
Eight paCO2 values, 20, 35, 39, 43, 49, 54, 70, and 80 mmHg had to be classified by the clinicians. The objective was to cover the maximal paCO2-range for the five exposed disease states in the given interview time of 45 min. For example in Fig. 2(1) one intensivist classified paCO2 = 54 mmHg between moderate hypoventilation and normal ventilation for ARDS patients.
2.1.1 Histogram generation
Histograms were generated to derive a compact and synoptic numerical and graphical presentation (see Fig. 2(2)) of experts’ cognitive concepts concerning the situation of mechanical ventilation. The histograms display how many from the 61 intensivists classified a given paCO2 value at the same position of the ventilation scale (between extreme hypoventilation and extreme hyperventilation). Sixteen histograms were created: eight for healthy lung status and eight for ARDS status according to the eight paCO2 values offered to the intensivists. For each paCO2 value, results are expressed as median (IQR: interquartile range) in both “healthy lungs” and ARDS. The x-axis displays the membership level μ from 0 to 1 which corresponds to one or two different states of the ventilation (μ_normal, μ_mod-hypo), and the y-axis depicts the number of intensivists whose answer fell in the same x-category. Using the example of paCO2 = 54 mmHg, the median of the distribution (black dot) corresponds to a membership grade of μ_normal = 0.2 in the normal ventilation and μ_mod hypo = 0.8 in the moderate hypoventilation status for ARDS patients.
2.2 Fuzzy system generator
2.2.1 Definition of fuzzy sets for arterial CO2 partial pressure
Every value in the scale corresponds to one or two membership levels from one or two fuzzy sets, respectively. Each “defining point” represents one paCO2 value and its membership level within a fuzzy set. All “defining points” of a fuzzy set were used to define the shape of the respective fuzzy membership function. Depending on the selected functional class of the membership function (e.g., trapezoidal, Gaussian) a fitting process optimized the shape of the membership function by minimizing the difference between defining points and membership function. The outcome, e.g., was a trapezoidal shape with a constant section at membership level = 1 for paCO2 values between 39 and 43 mmHg as shown in Fig. 2(3). Figure 2(4) displays the seven extracted fuzzy sets corresponding to ARDS patients, i.e., the fuzzy set “normal” has the shape as illustrated in Fig. 2(3).
2.2.2 Fuzzy rules and defuzzification
Arterial CO2 partial pressure as input parameter and respiratory rate as output parameter were interrelated using fuzzy rules. These fuzzy rules determined the impact of the change in respiratory rate which ranges from “decrease a lot”, over “decrease”, “decrease a bit”, “no change”, “increase a bit”, “ increase” until “increase a lot” and are constructed in the standard declarative form: IF situation THEN action:
-
1.
if paCO2 is “extreme hyperventilation” then respiratory rate is “decrease a lot”.
-
2.
if paCO2 is “strong hyperventilation” then respiratory rate is “decrease”.
-
3.
if paCO2 is “moderate hyperventilation” then respiratory rate is “decrease a bit”.
-
4.
if paCO2 is “normal ventilation” then respiratory rate is “no change”.
-
5.
if paCO2 is “moderate hypoventilation” then respiratory rate is “increase a bit”.
-
6.
if paCO2 is “strong hypoventilation” then respiratory rate is “increase”.
-
7.
if paCO2 is “extreme hypoventilation” then respiratory rate is “increase a lot”.
2.2.3 Automation of the process
The process described above including questionnaire-based interview of intensivists, generation of histograms, extraction of defining points, definition of fuzzy sets, and finally application of fuzzy rules for defuzzification was completely automated using the software programs LabView (Vers.8.0 National Instruments, Austin, TX, USA) and Matlab. (Vers. 7.2.0 The MathWorks Inc., Natick, MA, USA). A user interface was realized with LabView: Users are asked to mark a ventilation status of a patient to classify a given paCO2 value. For example an intensivist classified a given paCO2 = 54 mmHg for ARDS between “moderate hypoventilation” and “normal ventilation”. To confirm the assignment the clinician had to press an “ENTER” button. With a “CANCEL” button the clinician could correct the input if necessary.
The analysis of the questionnaires was performed using a MatLab program: The marks set by the clinicians were allocated to one of seven categories of ventilation status. The distribution over the categories was determined and the defining points extracted. These points were fitted using the Matlab toolbox “Curve fitting” to obtain the fuzzy sets: “Extreme hyperventilation”, “strong hyperventilation”, “moderate hyperventilation”, “normal ventilation”, “moderate hypoventilation”, “strong hypoventilation,” and “extreme hypoventilation”. The Matlab toolbox “Fuzzy Logic” completed the program integrating the new fuzzy membership functions creating rules and calculating the ventilator settings.
2.3 Implementation into the AUTOPILOT-BT and experimental evaluation
The disease-specific fuzzy sets have been implemented into the paCO2 controller of the AUTOPILOT-BT system. The performance of the fuzzy control system was tested using a previously developed physical lung simulator. As reported in a previous study [15] and represented in Fig. 3, different CO2 metabolic production rates were simulated using a pulmonary system model. We used a gas source to deliver CO2 with a concentration of 99%. The CO2 metabolic rate was adjusted by closing or opening valves. Two rotameters measured the metabolic rates before they were fed into a passive mechanical lung simulator (Model 5600i, Michigan Instruments, Grand Rapids, MI). This lung simulator was mechanically ventilated using the Evita 4 ventilator (Dräger Medical, Lübeck, Germany), which was controlled by our automated “closed-loop” ventilation system AUTOPILOT-BT [15]. The end-tidal CO2 partial pressure was measured on a breath-by-breath basis (Capno Plus-extension to Evita XL, Dräger Medical, Lübeck, Germany). A number of test series was performed with a combination of different, CO2 metabolic rates, start-respiratory rates, and the corresponding paCO2 start-values, to check the performance of the AUTOPILOT-BT system for “healthy lungs” and “ARDS”.
Experimental set up to analyze the performance of the AUTOPILOT-BT ventilation controller system. A pulmonary system model allows the simulation of CO2 metabolic production rates. CO2 delivered from a gas source is metered by means of manual valves and rotameters. The metered CO2 gas flow enters a mechanical lung simulator which is ventilated during the experiment. The ventilator is under control of the AUTOPILOT-BT. A clinician supervises the control system via a user interface. The end-tidal CO2 concentration is measured in the expiratory limb of the respiratory tubing
3 Results
The acquired knowledge of 61 intensivists was represented by histograms. Most of the experts agreed upon the classification of the paCO2 values for “healthy lungs” with respect to different ventilation.
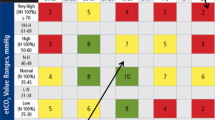
Figure 4 shows the distribution of the paCO2 value = 80 mmHg for “healthy lungs” (gray bars): 35 of the interviewed intensivists assigned this paCO2 value to the “extreme hypoventilation” status.
In order to demonstrate the methods of translating intensivist knowledge into disease-specific fuzzy sets, “normal ventilation” was exemplarily chosen. To identify the “defining points” of the membership function related to the eight paCO2 values, the corresponding membership levels in the “normal ventilation” fuzzy set were determined. PaCO2 values of 35 and 39 mmHg fell into the category of a membership level μ_normal = 1.0 for “healthy lungs” (Table 1).
The classification of the paCO2 values of 43 and 49 mmHg was somewhat ambiguous: they may belong either to “normal” or to “moderate hypoventilation”. paCO2 = 43 mmHg was found in the category “μ_normal = 0.6”. The membership level in the “normal” fuzzy set for 49 mmHg was even smaller (μ_normal = 0.2) and paCO2 values of 20, 54, 70, and 80 mmHg were for healthy lung patients considered definitely as NOT normal “μ_normal = 0”.
After fitting a trapezoidal function to “the defining points” the different shapes of the fuzzy sets for “healthy lungs” in the “normal ventilation” area were represented in gray in Fig. 5: The plateau indicates the range of paCO2 values defined as unquestionably normal, i.e., μ = 1. This plateau ranged from 35 to 39 mmHg for “healthy lungs”.
However, the distribution of paCO2 values for ARDS patients indicated a higher cognitive vagueness among the interviewed intensivists. The black bars depicted in Fig. 4 show that only 11 of the interviewed physicians associated a paCO2 of 80 mmHg with an “extreme hypoventilation” status in ARDS patients and there was a strong tendency to classify this value also as “moderate hypoventilation”.
For ARDS patients “defining points” were identified, which were different from those found in “healthy lungs” patients: A paCO2 of 35 mmHg was associated to “normal ventilation” with a membership level μ_normal = 0.6 and to “moderate hyperventilation” with level μ_mod hyper = 0.4. PaCO2 values of 39 and 43 mmHg were unequivocally found in the “normal ventilation” range (μ_normal = 1). PaCO2 of 49 mmHg had a membership level in “normal” (μ_normal = 0.6) and in “moderate hypoventilation” (μ_mod hypo:0.4). 54 mmHg belonged to “normal ventilation” only with μ_normal = 0.2 and μ_mod hypo = 0.8 corresponded to “moderate hypoventilation”. PaCO2 = 20, 70, and 80 mmHg were definitely considered as NOT “normal”.
The shape of the fuzzy sets for “ARDS” in the “normal ventilation” area is represented in black lines in Fig. 5. The plateau ranged from 39 to 43 mmHg for ARDS lungs.
The same methodology was applied to design the remaining six fuzzy sets. Figure 5 represents the seven fuzzy sets for “healthy lungs” and for “ARDS lungs”. The fuzzy control systems for “healthy lungs” and “ARDS” were created automatically by applying the same inference rules based on different membership functions.
Since diagnosis dependent membership functions were applied, the control of the AUTOPILOT-BT system changed with respect to the diagnosis. The AUTOPILOT-BT system was able to reach the target area of “normal ventilation” within maximal three consecutive steps, whatever disease pattern was assumed, either “healthy lungs” or “ARDS”. In Table 2, the results of the test series are shown. As a typical result Fig. 6 summarizes the test case characterized by a preset CO2 metabolic rate of 0.4 l/min, a respiratory rate of 16/min and a paCO2 start-value of 62 mmHg which was classified as “strong hypoventilation” in healthy lungs and “moderate hypoventilation” in ARDS lungs.
Performance of fuzzy control system for a “healthy” and b “ARDS” in case of a CO2 production rate of \( V_{{{\text{CO}}_{2} }}^{\prime } \) = 0.4 l/min. Three time intervals of 3 min each are plotted against the x-axis. The y-axis represents the paCO2 (left axis) and the respiratory rate (right axis), respectively. The target range of paCO2 is displayed as grey area
4 Discussion
The main results of the present investigation are: (i) The proposed methodology allows to automatically translate human decision-making strategies into a fuzzy-based ventilation system (AUTOPILOT-BT). (ii) With the incorporation of disease-specific therapy guidelines, the AUTOPILOT-BT adapts the ventilator control to the disease entity to which the patient belongs. (iii) In an experimental setup simulating different metabolic CO2 production rates the AUTOPILOT-BT system was evaluated. It reached the target “normal ventilation” area in maximal three consecutive controller cycles.
4.1 Methodology
At a first glance the proposed method how to acquire physician’s decision-making strategies and how to translate expert knowledge into fuzzy sets seems to be rather complex. However, the design of our questionnaire reflects the situation of decision making of the clinician at the bedside much better than conventional knowledge engineering approaches do: Instead of asking the clinicians, e.g., for the definition of the “normal” range of paCO2 [1] in a certain clinical setting, they are queried to classify paCO2-values that are presented in the same way as a bedside monitor does. The clinicians have to decide whether the given paCO2-values are acceptable, too low or too high from a clinical point of view. Prior to the query, clinicians are provided with information about the pulmonary condition of the patient. This way the situation at the bedside is mimicked allowing the clinician to evaluate the presented paCO2-value against the background of information about the diagnosis of the patient. In addition to paCO2 the interviewed intensivists were also asked to clinically classify arterial oxygen partial pressure (paO2), arterial oxygen saturation (SpO2), respiratory system compliance (Crs), and airway plateau pressure (Pplat) with respect to the given ventilation status. The expert knowledge of the clinicians was then directly translated into fuzzy sets showing, e.g., different patterns for lung healthy patients compared to ARDS patients. This translation was solely performed for paCO2. The same methodology of translation will be applied in the future for other physiological parameters. Thanks to this principle, the AUTOPILOT-BT is an open system for mechanical ventilation support being able to capture new strategies of lung protective mechanical ventilation therapy in a flexible way. The AUTOPILOT-BT system is able to implement automatically these guidelines and create the rules to control the ventilator anytime on demand of the authorized clinician. However, there are several limitations: (1) To answer the questionnaire is a time consuming process. The 61 intensivists participating in this study were simultaneously answering the questionnaire within 45 min. (2) This questionnaire was limited to several defining set-points which were presented in the context of 5 different pulmonary disease states. Thus, in the paper-based form just a rather coarse grained sampling (8 out of 100) of the knowledge of the intensivists was possible. However, more disease states could be incorporated and demand-driven sampling could be implemented in an on-line questionnaire that is to be developed. (3) This approach allows any clinician to tailor the control system according to his/her clinical preferences. What seems to be an advantage on one side may be viewed as an important disadvantage on the other hand. If really open for all clinicians the system would behave differently in every different environment, preventing any guarantee of clinical performance. Safety features should be implemented, so that only authorized clinicians are allowed to activate the input process.
4.2 Disease-specific control
In its actual status of development the system incorporates a total of three independent controllers: (i) a first controller for automatically setting the respiratory rate in order to control the CO2 excretion such as described in the present study, (ii) a second controller for setting the inspiratory oxygen fraction (FiO2) to control oxygenation and (iii) a third controller for setting tidal volume (V t) and positive end-expiratory pressure (PEEP) to control the transfer of mechanical energy between ventilator and lungs based on the analysis of respiratory mechanics considering the mechanics of the artificial airways such as the endotracheal tube [10]. Since the ventilatory parameters cannot be controlled independently, the output of these basic controllers is manipulated in the optimization unit before being transmitted to the ventilator [15]. All controllers are adapted in a disease-specific way. The information of disease-specific control of mechanical ventilation is directly supplied by the intensivist, who has to take into consideration the pathology of the patient insofar it is relevant for the ventilatory treatment. Currently five different clinical categories are differentiated: healthy (without pulmonary disease), CCI (cranio cerebral injury), ARDS (acute respiratory distress syndrome), COPD (chronic obstructive pulmonary disease), and fibrosis.
In automatic control engineering the controller dynamics is typically specified and used as a criterion of quality; in other words, the faster the controller achieves the control variable to reach its preset target value, the better is the controller. In contrast, the AUTOPILOT-BT controllers were not tuned to work as fast as possible, but rather to work with physiological and patient-adapted latency time, which is defined as the time interval between a controlling step and the achievement of a new steady state by the patient [11].
4.3 Experimental evaluation
The behavior of the paCO2-controller for “healthy lungs” and ARDS patients has been tested in an experimental setting as described in Sect. 2. The pulmonary system model was able to simulate pulmonary mechanics and gas exchange (elimination of CO2) evidencing, however, following limitations: (1) The experiments focused exclusively on the respiratory rate; any other physiological parameters, that could affect the CO2 gas exchange were not included. (2) Some of the simulated minute ventilation values (see Table 2) were included into the evaluation of the control system, though they were not physiological values. They should demonstrate the robustness and effectiveness of the system.
In several cases—as shown in Table 2—the fuzzy control system required multiple changes of the respiratory rate setting to reach the desired target range. The necessity of two or even more changes of the respiratory rate arises because of an initial overshoot of the control system. Figure 6a/b depicts the behavior of the control system in case “trial 11” in Table 2. With a start paCO2 value of 62 mmHg and a respiratory rate (RR) of 16/min for both “healthy lungs” and ARDS, Fig. 6a/b shows that the paCO2-target ranges derived from the questionnaire are different for “healthy” and ARDS as well as the controlling behavior associated with the applied rules of the corresponding membership functions. In Fig. 6 the first change of respiratory rate is less pronounced for “ARDS lungs” than for “healthy lungs”, which is caused by the fuzzy rules (see Sect. 2.2.2) that just allows the respiratory rate to increase “a bit” if the paCO2 value belongs to “moderate hypoventilation” (in ARDS). However, if the patient is in the “strongly hypoventilated” state the difference to “normal ventilation” is bigger therefore the respiratory rate must “increase” (in “healthy lungs”), which in this case provokes an overshoot. In order to reduce this kind of errors we could enlarge the rule table to relate more and finer grained membership functions to the change of respiratory rate. Thus, more membership functions have to be derived from the classification of paCO2. We could also enhance the control system with physiological models that may either be used for direct optimization or for performing a patient-specific rule adaptation. Further clinical trials will test the actual clinical efficiency of the paCO2 controller, and additional patient data will allow finer tuning of the fuzzy control parameters.
The AUTOPILOT-BT system is able to automatically convert expert knowledge, therapy guidelines as well as individual preferences of intensivists into automatic control of mechanical ventilation. The resulting strategy of controlling mechanical ventilation is mainly influenced by the expertise, experience and demands of the clinician. Due to its modular architecture the disease-specific AUTOPILOT-BT system can be extended by additional components. A further extension may incorporate other controllers to control, e.g., I:E ratio, duration of end-inspiratory pause (EIP), peak inspiratory airway pressure (Ppeak) as well as the expiratory flow pattern.
Another important aspect of the AUTOPILOT-BT system is that the intensivist is always in complete control of the system. It is not intended to substitute the physician, but the system serves the intensivists’ requirements. For a limited time interval and according to prescribed goals of the clinician, the system optimizes the ventilator settings with a fast sequence of control steps. Thus, the intensivist is relieved from detailed and time consuming tasks leaving more time for him/her to reason on the best therapeutical strategy for the individual patient.
We conclude that the AUTOPILOT-BT has the potential to automatically control mechanical ventilation according to established guidelines or to adapt the controlling system to modified ventilation therapies.
References
Bates JH, Young MP (2003) Applying fuzzy logic to medical decision making in the intensive care unit. Am J Respir Crit Care Med 167(7):948–952
Boegl K, Adlassnig KP, Hayashi Y, Rothenfluh TE, Leitich H (2004) Knowledge acquisition in the fuzzy knowledge representation framework of a medical consultation system. Artif Intell Med 30(1):1–26
Bouadma L, Lellouche F, Cabello B, Taille S, Mancebo J, Dojat M, Brochard L (2005) Computer-driven management of prolonged mechanical ventilation and weaning: a pilot study. Intensive Care Med 31(10):1446–1450
Carlo WA, Pacifico L, Chatburn RL, Fanaroff AA (1986) Efficacy of computer-assisted management of respiratory failure in neonates. Pediatrics 78(1):139–143
Dojat M, Brochard L, Lemaire F, Harf A (1992) A knowledge-based system for assisted ventilation of patients in intensive care units. Int J Clin Monit Comput 9(4):239–250
Dojat M, Harf A, Touchard D, Laforest M, Lemaire F, Brochard L (1996) Evaluation of a knowledge-based system providing ventilatory management and decision for extubation. Am J Respir Crit Care Med 153(3):997–1004
Dojat M, Pachet F, Guessoum Z, Touchard D, Harf A, Brochard L (1997) NeoGanesh: a working system for the automated control of assisted ventilation in ICUs. Artif Intell Med 11(2):97–117
Dojat M, Harf A, Touchard D, Lemaire F, Brochard L (2000) Clinical evaluation of a computer-controlled pressure support mode. Am J Respir Crit Care Med 161(4 Pt 1):1161–1166
Hernandez-Sande C, Moret-Bonillo V, Alonso-Betanzos A (1989) ESTER: an expert system for management of respiratory weaning therapy. IEEE Trans Biomed Eng 36(5):559–564
Jandre FC, Modesto FC, Carvalho AR, Giannella-Neto A (2008) The endotracheal tube biases the estimates of pulmonary recruitment and overdistension. Med Biol Eng Comput 46(1):69–73
Jensen M, Lozano S, Gottlieb D, Guttmann J, Möller K (2008) An evaluation of end-tidal CO2 change following alterations in ventilation frequency. In: Vander Sloten J, Verdonck P, Nyssen M, Haueisen J (eds) Proceedings of ECIFMBE 2008, IFMBE, 22
Kacmarek RM, Venegas J (1987) Mechanical ventilatory rates and tidal volumes. Respir Care 32:466–478
Kwok HF, Linkens DA, Mahfouf M, Mills GH (2003) Rule-base derivation for intensive care ventilator control using ANFIS. Artif Intell Med 29(3):185–201
Lellouche F, Mancebo J, Jolliet P, Roeseler J, Schortgen F, Dojat M, Cabello B, Bouadma L, Rodriguez P, Maggiore S, Reynaert M, Mersmann S, Brochard L (2006) A multicenter randomized trial of computer-driven protocolized weaning from mechanical ventilation. Am J Respir Crit Care Med 174(8):894–900
Lozano S, Möller K, Brendle A, Gottlieb D, Schumann S, Stahl CA, Guttmann J (2008) AUTOPILOT-BT: a system for knowledge and model based mechanical ventilation. Technol Health Care 16(1):1–11
Miller PL (1985) Goal-directed critiquing by computer: ventilator management. Comput Biomed Res 18(5):422–438
Nemoto T, Hatzakis GE, Thorpe CW, Olivenstein R, Dial S, Bates JH (1999) Automatic control of pressure support mechanical ventilation using fuzzy logic. Am J Respir Crit Care Med 160(2):550–556
Rudowski R, Frostell C, Gill H (1989) A knowledge-based support system for mechanical ventilation of the lungs. The KUSIVAR concept and prototype. Comput Methods Programs Biomed 30(1):59–70
Schaublin J, Derighetti M, Feigenwinter P, Petersen-Felix S, Zbinden AM (1996) Fuzzy logic control of mechanical ventilation during anaesthesia. Br J Anaesth 77(5):636–641
Shahsavar N, Ludwigs U, Blomqvist H, Gill H, Wigertz O, Matell G (1995) Evaluation of a knowledge-based decision-support system for ventilator therapy management. Artif Intell Med 7(1):37–52
Sittig DF, Pace NL, Gardner RM, Beck E, Morris AH (1989) Implementation of a computerized patient advice system using the HELP clinical information system. Comput Biomed Res 22(5):474–487
Sun Y, Kohane I, Stark AR (1994) Fuzzy logic assisted control of inspired oxygen in ventilated newborn infants. Proc Annu Symp Comput Appl Med Care: 757–761
Tehrani FT (2008) Automatic control of mechanical ventilation. Part 1: theory and history of the technology. J Clin Monit Comput 22(6):409–415
Tehrani FT (2008) Automatic control of mechanical ventilation. Part 2: the existing techniques and future trends. J Clin Monit Comput 22(6):417–424
Tehrani FT, Roum JH (2008) Intelligent decision support systems for mechanical ventilation. Artif Intell Med 44(3):171–182
Tong DA (1991) Weaning patients from mechanical ventilation. A knowledge-based system approach. Comput Methods Programs Biomed 35(4):267–278
Acknowledgments
This work was supported by Bundesministerium für Bildung und Forschung (Grant 1781X08 MOTiF-A), and Dräger Medical, Lübeck.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lozano-Zahonero, S., Gottlieb, D., Haberthür, C. et al. Automated mechanical ventilation: adapting decision making to different disease states. Med Biol Eng Comput 49, 349–358 (2011). https://doi.org/10.1007/s11517-010-0712-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-010-0712-0