Abstract
Background
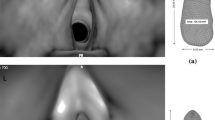
Human snores are caused by vibrating anatomical structures in the upper airway. The glottis is a highly variable structure and a critical organ regulating inhaled flows. However, the effects of the glottis motion on airflow and breathing sound are not well understood, while static glottises have been implemented in most previous in silico studies. The objective of this study is to develop a computational acoustic model of human airways with a dynamic glottis and quantify the effects of glottis motion and tidal breathing on airflow and sound generation.
Methods
Large eddy simulation and FW-H models were adopted to compute airflows and respiratory sounds in an image-based mouth-lung model. User-defined functions were developed that governed the glottis kinematics. Varying breathing scenarios (static vs. dynamic glottis; constant vs. sinusoidal inhalations) were simulated to understand the effects of glottis motion and inhalation pattern on sound generation. Pressure distributions were measured in airway casts with different glottal openings for model validation purpose.
Results
Significant flow fluctuations were predicted in the upper airways at peak inhalation rates or during glottal constriction. The inhalation speed through the glottis was the predominating factor in the sound generation while the transient effects were less important. For all frequencies considered (20–2500 Hz), the static glottis substantially underestimated the intensity of the generated sounds, which was most pronounced in the range of 100–500 Hz. Adopting an equivalent steady flow rather than a tidal breathing further underestimated the sound intensity. An increase of 25 dB in average was observed for the life condition (sine-dynamic) compared to the idealized condition (constant-rigid) for the broadband frequencies, with the largest increase of approximately 40 dB at the frequency around 250 Hz.
Conclusion
Results show that a severely narrowing glottis during inhalation, as well as flow fluctuations in the downstream trachea, can generate audible sound levels.













Similar content being viewed by others
References
Dalmasso F, Prota R (1996) Snoring: analysis, measurement, clinical implications and applications. Eur Respir J 9:146–159
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Lindberg E, Elmasry A, Gislason T, Janson C, Bengtsson H, Hetta J, Nettelbladt M, Boman G (1999) Evolution of sleep apnea syndrome in sleepy snorers—a population-based prospective study. Am J Respir Crit Care Med 159:2024–2027
Key APF, Molfese DL, O’Brien L, Gozal D (2009) Sleep-disordered breathing affects auditory processing in 5–7-year-old children: evidence from brain recordings. Dev Neuropsychol 34:615–628
Lee Y-H, Kweon S-S, Choi BY, Kim MK, Chun B-Y, Shin DH, Shin M-H (2014) Self-reported snoring and carotid atherosclerosis in middle-aged and older adults: the Korean Multi-Rural Communities Cohort Study. J Epidemiol 24:281–286
Touboul PJ, Grobbee DE, den Ruijter H (2012) Assessment of subclinical atherosclerosis by carotid intima media thickness: technical issues. Eur J Prev Cardiol 19:18–24
Abeyratne UR, Karunajeewa AS, Hukins C (2007) Mixed-phase modeling in snore sound analysis. Med Biol Eng Comput 45:791–806
Abo-Khatwa MM, Osman EZ, Hill PD, Lee BWV, Osborne JE (2008) Objective evaluation of tongue base snoring after the use of an oral appliance: a prospective case series. Clin Otolaryngol 33:592–595
Agrawal S, Stone P, McGuinness K, Morris J, Camilleri AE (2002) Sound frequency analysis and the site of snoring in natural and induced sleep. Clin Otolaryngol 27:162–166
Beck R, Odeh M, Oliven A, Gavriely N (1995) The acoustic properties of snores. Eur Respir J 8:2120–2128
Beninati W, Harris CD, Herold DL, Shepard JW (1999) The effect of snoring and obstructive sleep apnea on the sleep quality of bed partners. Mayo Clin Proc 74:955–958
Caffier PP, Berl JC, Muggli A, Reinhardt A, Jakob A, Moeser M, Fietze I, Scherer H, Hoelzl M (2007) Snoring noise pollution—the need for objective quantification of annoyance, regulatory guidelines and mandatory therapy for snoring. Physiol Meas 28:25–40
Emoto T, Abeyratne UR, Akutagawa M, Konaka S, Kinouchi Y (2011) High frequency region of the snore spectra carry important information on the disease of sleep apnoea. J Med Eng Technol 35:425–431
Gavriely N, Jensen O (1993) Theory and measurements of snores. J Appl Physiol 74:2828–2837
Hara H, Murakami N, Miyauchi Y, Yamashita H (2006) Acoustic analysis of snoring sounds by a multidimensional voice program. Laryngoscope 116:379–381
Hill PD, Osman EZ, Osborne JE, Lee BWV (2000) Changes in snoring during natural sleep identified by acoustic crest factor analysis at different times of night. Clin Otolaryngol 25:507–510
Jones TM, Ho MS, Earis JE, Swift AC, Charters P (2006) Acoustic parameters of snoring sound to compare natural snores with snores during “steady-state” propofol sedation. Clin Otolaryngol 31:46–52
Lofaso F, Coste A, d’Ortho MP, Zerah-Lancner F, Delclaux C, Goldenberg F, Harf A (2000) Nasal obstruction as a risk factor for sleep apnoea syndrome. Eur Respir J 16:639–643
Atkins M, Taskar V, Clayton N, Stone P, Woodcock A (1994) Nasal resistance in obstructive sleep apnea. Chest 105:1133–1135
Xu HJ, Huang WN, Yu LS, Chen L (2010) Sound spectral analysis of snoring sound and site of obstruction in obstructive sleep apnea syndrome. Acta Otolaryngol 130:1175–1179
Quinn SJ, Huang L, Ellis PD, Williams JEF (1996) The differentiation of snoring mechanisms using sound analysis. Clin Otolaryngol 21:119–123
Saunders NC, Tassone P, Wood G, Norris A, Harries M, Kotecha B (2004) Is acoustic analysis of snoring an alternative to sleep nasendoscopy? Clin Otolaryngol 29:242–246
Miyazaki S, Itasaka Y, Ishikawa K, Togawa K (1998) Acoustic analysis of snoring and the site of airway obstruction in sleep related respiratory disorders. Acta Otolaryngol 537:47–51
Harper VP, Pasterkamp H, Kiyokawa H, Wodicka GR (2003) Modeling and measurement of flow effects on tracheal sounds. IEEE Trans Biomed Eng 50:1–10
Mihaescu M, Murugappan S, Kalra M, Khosla S, Gutmark E (2008) Large eddy simulation and Reynolds-averaged Navier-Stokes modeling of flow in a realistic pharyngeal airway model: an investigation of obstructive sleep apnea. J Biomech 41:2279–2288
Mihaescu M, Mylavarapu G, Gutmark EJ, Powell NB (2011) Large eddy simulation of the pharyngeal airflow associated with obstructive sleep apnea syndrome at pre and post-surgical treatment. J Biomech 44:2221–2228
Powell NB, Mihaescu M, Mylavarapu G, Weaver EM, Guilleminault C, Gutmark E (2011) Patterns in pharyngeal airflow associated with sleep-disordered breathing. Sleep Med 12:966–974
Sittitavornwong S, Waite PD, Shih AM, Koomullil R, Ito Y, Cheng GC, Wang D (2009) Evaluation of obstructive sleep apnea syndrome by computational fluid dynamics. Semin Orthod 15:105–131
Xu C, Sin S, McDonough JM, Udupa JK, Guez A, Arens R, Wootton DM (2006) Computational fluid dynamics modeling of the upper airway of children with obstructive sleep apnea syndrome in steady flow. J Biomech 39:2043–2054
Yu CC, Hsiao HD, Tseng TI, Lee LC, Yao CM, Chen NH, Wang CJ, Chen YR (2012) Computational fluid dynamics study of the inspiratory upper airway and clinical severity of obstructive sleep apnea. J Craniofac Surg 23:401–405
Xi J, Si X, Kim J, Su G, Dong H (2014) Modeling the pharyngeal anatomical effects on breathing resistance and aerodynamically generated sound. Med Biol Eng Comput 52:567–577
Lin C-L, Tawhai MH, McLennan G, Hoffman EA (2007) Characteristics of the turbulent laryngeal jet and its effect on airflow in the human intra-thoracic airways. Respir Physiol Neurobiol 157:295–309
Xi J, Longest PW, Martonen TB (2008) Effects of the laryngeal jet on nano- and microparticle transport and deposition in an approximate model of the upper tracheobronchial airways. J Appl Phys 104:1761–1777
Daily DJ, Thomson SL (2013) Acoustically-coupled flow-induced vibration of a computational vocal fold model. Comput Struct 116:50–58
Khosla S, Muruguppan S, Gutmark E, Scherer R (2007) Vortical flow field during phonation in an excised canine larynx model. Ann Otol Rhinol Laryngol 116:217–228
Khosla S, Murugappan S, Lakhamraju R, Gutmark E (2008) Using particle imaging velocimetry to measure anterior-posterior velocity gradients in the excised canine larynx model. Ann Otol Rhinol Laryngol 117:134–144
Khosla S, Murugappan S, Gutmark E (2008) What can vortices tell us about vocal fold vibration and voice production. Curr Opin Otolaryngol Head Neck Surg 16:183–187
Olney DR, Greinwald JH Jr, Smith RJ, Bauman NM (1999) Laryngomalacia and its treatment. Laryngoscope 109:1770–1775
Awan S, Saleheen D, Ahmad Z (2004) Laryngomalacia: an atypical case and review of the literature. Ear Nose Throat J 83(334):336–338
Xi J, Longest PW (2008) Evaluation of a drift flux model for simulating submicrometer aerosol dynamics in human upper tracheobronchial airways. Ann Biomed Eng 36:1714–1734
Xi J, Longest PW (2007) Transport and deposition of micro-aerosols in realistic and simplified models of the oral airway. Ann Biomed Eng 35:560–581
Cohen BS, Sussman RG, Lippmann M (1990) Ultrafine particle deposition in a human tracheobronchial cast. Aerosol Sci Technol 12:1082–1093
Scheinherr A, Bailly L, Boiron O, Lagier A, Legou T, Pichelin M, Caillibotte G, Giovanni A (2015) Realistic glottal motion and airflow rate during human breathing. Med Eng Phys 37:829–839
Scheinherr A, Bailly L, Boiron O, Legou T, Giovanni A, Caillibotte G, Pichelin M (2012) Glottal motion and its impact on the respiratory flow. Comput Methods Biomech Biomed Eng 15:69–71
Lane RW, Weider DJ, Steinem C, Marin-Padilla M (1984) Laryngomalacia. A review and case report of surgical treatment with resolution of pectus excavatum. Arch Otolaryngol 110:546–551
Pevernagie D, Aarts RM, De Meyer M (2010) The acoustics of snoring. Sleep Med Rev 14:131–144
Saha S, Bradley TD, Taheri M, Moussavi Z, Yadollahi A (2016) A subject-specific acoustic model of the upper airway for snoring sounds generation. Sci Rep 6:25730
Douglas NJ, White DP, Pickett CK, Weil JV, Zwillich CW (1982) Respiration during sleep in normal man. Thorax 37:840–844
Nicoud F, Ducros F (1999) Subgrid-scale stress modeling based on the square of the velocity gradient tensor. Flow Turbul Combust 62:183–200
Proudman I (1952) The generation of noise by isotropic turbulence. Proceedings of the Royal Society of London Series A—Mathematical and Physical. Sciences 214:119–132
Ffowes Williams JE, Hawkings DL (1969) Sound generation by turbulence and surfaces in arbitrary motion. Philosophical Transactions of the Royal Society of London A (Mathematical and Physical Sciences) 264:321–342
Lilley GM (1993) The radiated noise from isotropic turbulence revisited. NASA Contract Report 93–75, NASA Langley Research Center, Hampton, VA
Brentner KS, Farassat F (2003) Modeling aerodynamically generated sound of helicopter rotors. Prog Aerosp Sci 39:83–120
Bregraves GA, Peacuterot F, Freed D (2010) A Ffowcs Williams-Hawkings solver for Lattice-Boltzmann based computational aeroacoustics. 16th AIAA/CEAS Aeroacoustics Conference 2010. 31st AIAA Aeroacoustics Conference:145–159
Khelladi S, Bakir F (2010) A consistency test of thickness and loading noise codes using Ffowcs Williams and Hawkings equation. Advances in Acoustics and Vibration: 174,361 (174,366 pp.)–174,361 (174,366 pp.)
Spalart PR, Shur ML (2009) Variants of the Ffowcs Williams-Hawkings equation and their coupling with simulations of hot jets. Int J Aeroacoustics 8:477–491
Grossmann A, Morlet J (1984) Decomposition of Hardy functions into square integrable wavelets of constant shape. SIAM J Math Anal 15:723–736
Subbu A, Ray A (2008) Space partitioning via Hilbert transform for symbolic time series analysis, pp. 084,107–084,107
Jubran BA, Hamdan MN, Shabanneh NH, Szepessy S (1998) Wavelet and chaos analysis of irregularities of vortex shedding. Mech Res Commun 25:583–591
Xi J, Yuan JE, Yang M, Si X, Zhou Y, Cheng YS (2016) Parametric study on mouth-throat geometrical factors on deposition of orally inhaled aerosols. J Aerosol Sci 99:94–106
Revell JD, Prydz RA, Hays AP (1977) Experimental study of airframe noise vs. drag relationship for circular cylinders. Lockheed Report 28074, Final Report for NASA Contract NAS1–14403. Final Report for NASA Contract NAS1–14403
Larrosa F, Hernandez L, Morello A, Ballester E, Quinto L, Montserrat JM (2004) Laser-assisted uvulopalatoplasty for snoring: does it meet the expectations? Eur Respir J 24:66–70
Xi J, Si XA, Kim J, Mckee E, Lin E-B (2014) Exhaled aerosol pattern discloses lung structural abnormality: a sensitivity study using computational modeling and fractal analysis. PLoS One 9:e104682
Lee GS, Lee LA, Wang CY, Chen NH, Fang TJ, Huang CG, Cheng WN, Li HY (2016) The frequency and energy of snoring sounds are associated with common carotid artery intima-media thickness in obstructive sleep apnea patients. Sci Rep 6:30559
Hu FB, Willett WC, Manson JE, Colditz GA, Rimm EB, Speizer FE, Hennekens CH, Stampfer MJ (2000) Snoring and risk of cardiovascular disease in women. J Am Coll Cardiol 35:308–313
Ffowcs Williams JE, Hawkings DL (1969) Sound generation by turbulence and surfaces in arbitrary motion. Philos Trans Royal Soc A264:321–342
Ramig LO, Fox C, Sapir S (2008) Speech treatment for Parkinson’s disease. Expert Rev Neurother 8:297–309
Blumin JH, Berke GS (2002) Bilateral vocal fold paresis and multiple system atrophy. Arch Otolaryngol–Head Neck Surg 128:1404–1407
Pasterkamp H, Kraman SS, Wodicka GR (1997) Respiratory sounds—advances beyond the stethoscope. Am J Respir Crit Care Med 156:974–987
Pickering DN, Beardsmore CS (1999) Nasal flow limitation in children. Pediatr Pulmonol 27:32–36
Ohki M, Ogoshi T, Yuasa T, Kawano K, Kawano M (2005) Extended observation of the nasal cycle using a portable rhinoflowmeter. J Otolaryngol 34:346–349
Funding
NSF provided financial support in the form of Grants CBET 1605434 (Xi) and 1605232 (Dong). This work was partially supported by NIH R01 CA204189 (Glide-Hurst). The supporters have no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Xi, J., Wang, Z., Talaat, K. et al. Numerical study of dynamic glottis and tidal breathing on respiratory sounds in a human upper airway model. Sleep Breath 22, 463–479 (2018). https://doi.org/10.1007/s11325-017-1588-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1588-0