Abstract
Purpose
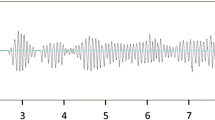
The characterization of apneas during polysomnography (PSG) as obstructive or central is a key element of a sleep study. Pulse transit time (PTT) has demonstrated its potential as a noninvasive surrogate marker for inspiratory efforts. The aim of the study was to assess the ability of PTT to classify apneas as central or obstructive, as compared to respiratory inductance plethysmography (RIP) in children.
Methods
Overnight PSG with simultaneous PTT recording was performed on 11 consecutive children (mean age 8.9 years, range 1–18.2 years). The same observer scored the apneas using two blinded configurations: (1) the RIP scoring used the nasal pressure, thermistors, thoracic and abdominal movements, and pulse oximetry signals: (2) the PTT scoring used PTT in combination with all the other signals without the thoracic and abdominal movements.
Results
One hundred fourteen apneas out of a total of 520 respiratory events were analyzed. With RIP, 58 (51%) apneas were scored as obstructive and 56 (49%) as central. Using PTT, 77 (68%) of the apneas were scored as obstructive and 37 (32%) as central. When using PTT, 30 apneas scored as central by RIP were scored as obstructive. PTT was highly sensitive (81%) but poorly specific (46%) in scoring 58 apneas as obstructive. PTT was less sensitive (46%) but highly specific (81%) to score 56 apneas as central.
Conclusion
PTT may be used as an additional tool to RIP to improve the scoring of apneas as obstructive or central in children. The high percentage of artifact is a limitation of PTT.

Similar content being viewed by others
References
Kaditis AG, Alonso Alvarez ML, Boudewyns A, Alexopoulos EI, Ersu R, Joosten K, Larramona H, Miano S, Narang I, Trang H, Tsaoussoglou M, Vandenbussche N, Villa MP, Van Waardenburg D, Weber S, Verhulst S (2016) Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J 47:69–94
Chervin RD, Aldrich MS (1997) Effects of esophageal pressure monitoring on sleep architecture. Am J Respir Crit Care Med 156:881–885
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:597–619
Staats BA, Bonekat HW, Harris CD, Offord KP (1984) Chest wall motion in sleep apnea. Am Rev Respir Dis 130:59–63
Boudewyns A, Willemen M, Wagemans M, De Cock W, Van de Heyning P, De Backer W (1997) Assessment of respiratory effort by means of strain gauges and esophageal pressure swings: a comparative study. Sleep 20:168–170
Luo YM, Tang J, Jolley C, Steier J, Zhong NS, Moxham J, Polkey MI (2009) Distinguishing obstructive from central sleep apnea events: diaphragm electromyogram and esophageal pressure compared. Chest 135:1133–1141
Pitson D, Stradling J (1998) Autonomic markers of arousal during sleep in patients undergoing investigation for obstructive sleep apnoea, their relationship to EEG arousals, respiratory events and subjective sleepiness. J Sleep Res 7:53–59
Pitson D, Sandell A, Van den Hout R, Stradling J (1995a) Use of pulse transit time as a measure of inspiratory effort in patients with obstructive sleep apnoea. Eur Respir J 81:669–674
Argod J, Pépin JL, Smith RP, Lévy P (2000) Comparison of esophageal pressure with pulse transit time as a measure of respiratory effort for scoring obstructive nonapneic respiratory events. Am J Respir Crit Care Med 162:87–93
Foo JYA, Wilson SJ, Bradley AP, Williams GR, Harris MA, Cooper DM (2005) Use of pulse transit time to distinguish respiratory events from tidal breathing in sleeping children. Chest 128:3013–3019
Geddes LA, Voelz M, James S, Reiner D (1981) Pulse arrival time as a method of obtaining systolic and diastolic blood pressure indirectly. Med Biol Eng Comput 19:671–762
Argod J, Pépin JL, Lévy P (1998) Differentiating obstructive and central sleep respiratory events through pulse transit time. Am J Respir Crit Care Med 158:1778–1783
Pitson DJ, Sandell A, van den Hout R, Stradling JR (1995b) Use of pulse transit time as a measure of inspiratory effort in patients with obstructive sleep apnoea. Eur Respir J 8:1668–1674
Katz ES, Lutz J, Black C, Marcus CL (2003) Pulse transit time as a measure of arousal and respiratory effort in children with sleep-disordered breathing. Pediatr Res 53:580–588
Pépin JL, Delavie N, Pin I, Deschaux C, Argod J, Bost M, Levy P (2005) Pulse transit time improves detection of sleep respiratory events and microarousals in children. Chest 127:722–730
Galland BC, Tan E, Taylor BJ (2007) Pulse transit time and blood pressure changes following auditory-evoked subcortical arousal and waking of infants. Sleep 30:891–897
Foo JYA, Wilson SJ, Williams GR, Harris MA, Cooper DM (2008) Investigation of pulse transit time characteristics during single and recurrent obstructive respiratory events. J Clin Monit Comput 22:327–332
Smith RP, Argod J, Pépin JL, Lévy PA (1999) Pulse transit time: an appraisal of potential clinical applications. Thorax 54:452–457
Farré R, Montserrat JM, Navajas D (2004) Noninvasive monitoring of respiratory mechanics during sleep. Eur Respir J 24:1052–1060
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Financial support
No funding was received for this research. The research of Brigitte Fauroux is supported by the Association Française contre les Myopathies (AFM), Assistance Publique-Hôpitaux de Paris, Inserm, Université Paris Descartes, ADEP Assistance, ASV Santé, S2A and Elivie.
Additional information
Comment
This paper adds an important contribution for the clinical application of the PTT which can be used as an adjunct tool for the screening and evaluation of SDB.
Luigi Nespoli
Varese, Italy
Rights and permissions
About this article
Cite this article
Griffon, L., Amaddeo, A., Olmo Arroyo, J. et al. Pulse transit time as a tool to characterize obstructive and central apneas in children. Sleep Breath 22, 311–316 (2018). https://doi.org/10.1007/s11325-017-1488-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1488-3