Abstract
Aspirin (acetylsalicylic acid, ASA) can lead to gastrointestinal mucosal injury through disruption of its protective phospholipid bilayer. A liquid formulation of a novel pharmaceutical lipid–aspirin complex (PL-ASA) was designed to prevent this disruption. We sought to determine the pharmacokinetic (PK)/pharmacodynamic (PD) characteristics of PL-ASA compared with immediate release aspirin (IR-ASA). In this active-control crossover study, 32 healthy volunteers were randomized to receive 1 of 2 dose levels (a single dose of 325 mg or 650 mg) of either PL-ASA or IR-ASA. After a 2-week washout period between treatment assignments, subjects received a single dose of the alternative treatment, at the same dose level. The primary objectives of the study were to assess, for PL-ASA and IR-ASA at 325 mg and 650 mg dose levels, PK and PD bioequivalence, and safety, over a 24–h period after administration of both drugs. PK parameters were similar for PL-ASA and IR-ASA, and met FDA-criteria for bioequivalence. Regarding PD, both drugs also showed Cmin TxB2 values below 3.1 ng/mL (cut-off associated with decreased cardiovascular events) and > 99% inhibition of serum TxB2 ( ≥ 95% inhibition represents the cut-off for aspirin responders) along with similar results in several secondary PK/PD parameters. There were no serious adverse events or changes from baseline in vital signs or laboratory values in either of the 2 treatment groups. PL-ASA’s novel liquid formulation has similar PK and PD performance compared with IR-ASA, supporting functional and clinical equivalence. These data coupled with the improved gastric safety of PL-ASA suggest that this novel formulation may exhibit an improved benefit-risk profile, warranting evaluation in future trials.
Clinical trial registration:http://www.clinicaltrials.gov. Unique Identifier: NCT04008979
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
Observational studies of upper gastrointestinal (GI) bleeding in patients taking aspirin showed that the risk is not lowered with coated tablets; PD studies also suggest high rates of non-responsiveness.
-
The novel pharmaceutical lipid-aspirin-complex (PL-ASA) liquid capsule formulation has been specifically designed to reduce the acute GI toxicity of aspirin.
-
The results of the current study demonstrate functional and clinical bioequivalence between immediate release aspirin and PL-ASA and suggest that this novel aspirin formulation with significantly lower risk of acute GI toxicity can also deliver aspirin in a fast and reliable manner that results in the desired antiplatelet effect.
-
Further studies are warranted to test the performance of PL-ASA versus enteric-coated aspirin, the preferred aspirin by the majority of physicians and patients.
Introduction
Aspirin, or acetylsalicylic acid, is an irreversible inhibitor of the platelet cyclooxygenase (COX)-1 enzyme, which leads to suppression of thromboxane (Tx) A2 formation, a potent inducer of platelet activation and aggregation [1]. Low-dose aspirin regimens (75 to 325 mg) are commonly used for the prevention of serious vascular events in patients with established atherosclerotic disease [2].
Although recent data have questioned its role for primary prevention, low-dose aspirin still remains a cornerstone of guideline-recommended therapy for secondary prevention [2,3,4,5]. High-dose aspirin ( ≥ 650 mg) has antipyretic, analgesic and anti-inflammatory properties, which are primarily mediated through inhibition of COX-2 by salicylic acid, aspirin’s primary metabolite [1]. In addition to the established efficacy, aspirin is also frequently associated with gastrointestinal (GI) toxicity and bleeding, which can lead to poor adherence or discontinuation and increase the risk of ischemic recurrences [6,7,8].
Aspirin-induced GI toxicity is mediated by three mechanisms including: (a) impaired hemostatic function via antiplatelet effects (b) inhibition of COX-derived prostaglandin (PG) production (locally and through systemic exposure), which is key in epithelial mucus production, microvascular mucosal perfusion and wound healing in the GI tract, and (c) physical disruption of the protective gastric phospholipid barrier thereby allowing direct acid injury [9]. With an estimated 40 million Americans consuming daily aspirin, GI-related toxicity associated with aspirin use represents an important public health problem [10]. These observations underscore the need for aspirin formulations with a more favorable safety profile while maintaining pharmacologic efficacy.
PL-ASA is a novel pharmaceutical lipid–aspirin complex liquid formulation developed to mitigate disruption of the epithelial phospholipid layer of the gastric mucosa without delaying absorption [11,12,13]. This study was a prospective pharmacokinetic (PK) and pharmacodynamic (PD) evaluation conducted to define bioequivalence and support the new drug application and subsequent approval of PL-ASA by the United States Food and Drug Administration (FDA). To determine bioequivalence for FDA approval, the study was performed with healthy volunteers, and the doses studied bracketed currently approved doses for aspirin for cardiovascular protection (i.e., 325 mg) and anti-inflammatory effects (i.e., 650 mg).
Methods
Study design and study population
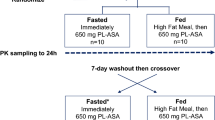
This current investigation was a randomized, active control, cross-over study to assess the bioequivalence (using PK and PD parameters), and safety of PL-ASA compared with IR-ASA administered orally at a single dose (Clinicaltrials.gov identifier: NCT04008979). The study design and details of the study conduct are provided in the Supplemental Appendix (Online Fig. 1, Online Table 1, and “Statistical methods”). A total of 32 healthy subjects were randomized to treatment with 1 of 2 dose levels (325 mg or 650 mg) of either IR-ASA tablets (Genuine Bayer® Aspirin) or PL-ASA capsules. After a 2-week washout period between treatment assignments, subjects received a single dose of the alternative treatment, at the same dose level. Therefore, in aggregate, each subject received a total of two doses of study drug (one dose of PL-ASA and one dose of IR-ASA at the same dose level) separated by a 2-week washout period between the doses.
All subjects were included in the safety analyses, which included monitoring incidence of adverse events, and changes in laboratory assessments (hematology and blood chemistry) and vital signs. The study protocol was approved by IntegReview Ethical Review Board (IORG Number IORG0000689) and conducted in the Houston Institute for Clinical Research. Dr Angiolillo prepared the first draft of this manuscript, and had full access to the analyzed data.
PK and PD analyses
After absorption, as acetylsalicylic acid is rapidly converted to salicylic acid by hydrolysis and first-pass metabolism, peak plasma concentrations of acetylsalicylic acid are extremely sensitive to minor variations in solid dosage form dissolution and disintegration. In contrast, plasma concentrations of salicylic acid are predictable and relatively stable, and salicylic acid is considered to be a superior analyte for comparative bioequivalence assessments. Salicylic acid PK parameters were used for primary PK endpoints.
The primary PK endpoints were the parameters AUC0-t, AUC0-∞, Cmax, tmax, λz, t½, VD/F, and CL/F of the primary PL-ASA/IR-ASA metabolite salicylic acid, and the primary PD endpoints were AUC0-24, Imax, and tmax of the percent inhibition of serum Thromboxane B2 (TxB2) levels. PK and PD parameters were used to assess bioequivalence [14]. Secondary PK endpoints included similar PK parameters for acetylsalicylic acid; secondary PD endpoints assessed the incidence of aspirin responders and the level of platelet aggregation in response to arachidonic acid and collagen in an ex vivo assay. The full list of PK and PD endpoints measured are given in Online Table 1.
Statistical methods
PK analyses were performed on all 32 subjects. For the comparisons between PL-ASA and IR-ASA, confidence intervals (CI) of 95% were employed, and statistical significance was assessed using a two-sided test at the 0.05 significance level. For bioequivalence analyses, 90% CI were employed, and statistical significance was assessed using 2 one-sided tests at the 0.05 significance level. Further details of the statistical analysis methods are given in the Supplemental Appendix.
Analytical methods
Plasma samples were collected into sodium fluoride/potassium oxalate, frozen (-80 °C) and analyzed by MEDTOX Laboratories, St. Paul, MN. Salicylic acid and acetylsalicylic acid plasma levels and TxB2 serum levels were determined by High Performance Liquid Chromatography with tandem Mass Spectrometry (LC- MS/MS). Urinary 11-dehydro-TxB2 was determined by an Enzyme-Linked Immunosorbent Assay (ELISA), and urinary creatinine was measured via a spectrophotometric assay. Subjects were considered as being aspirin responders if: (a) demonstrated ≥ 95% inhibition of serum TxB2 levels (b) had TxB2 Cmin values < 3.1 ng/mL, or c) had values of urinary 11-dehydro-TxB2 ≤ 1500 pg/mg of creatinine [15,16,17]. Inhibition of platelet aggregation in response to arachidonic acid (0.5 mg/mL) and collagen (4 µg/mL, fibrillar Type I) as agonists in blood samples collected after study treatment was measured by ex vivo light transmittance aggregometry.
Results
Pharmacokinetic results
The bioavailability of aspirin was estimated using the stable active metabolite plasma salicylic acid. Concentration–time curves for acetylsalicylic acid and salicylic acid levels illustrate that time to mean peak acetylsalicylic acid concentration after PL-ASA appears to be nominally longer and mean peak acetylsalicylic acid concentration slightly lower compared with IR-ASA, however, none of these differences were statistically significant and both formulations were absorbed and metabolized at similar rates (Fig. 1).
Impact of the pharmaceutical formulation on aspirin’s disposition. Plasma concentration time profiles of acetylsalicylic acid (a, b) and salicylic acid (c, d) were compared in healthy, fasted volunteers who received single doses (325 and 650 mg) of PL-ASA and IR-ASA. h hours, IR-ASA immediate release aspirin, mg milligrams, ng nanograms, PL-ASA pharmaceutical lipid–aspirin complex
For the primary endpoints (the salicylic acid PK parameters AUC0−t, AUC0–∞, Cmax, tmax, λz, t½, VD/F, and CL/F), the PK parameter values were similar for PL-ASA and IR-ASA, but the median AUC0−t and Cmax values were nominally slightly higher for the PL-ASA group than for the IR-ASA group at the 325 mg dose level (Table 1); at the 650 mg dose level, the median AUC0−t, AUC0–∞, and Cmax values are slightly higher following IR-ASA treatment (Table 1). Comparable results were obtained by analysis of PK parameters based on acetylsalicylic acid, a secondary endpoint: the acetylsalicylic acid PK parameters for both study drugs were similar, but the median AUC0−t and AUC0–∞ values were nominally slightly higher for the IR-ASA group and median Cmax values are nominally slightly higher following PL-ASA at both dose levels (Online Table 3).
Values of the log-transformed PK parameters AUC0−t, AUC0–∞, and Cmax for the ratio of PL-ASA to IR-ASA were examined to evaluate bioequivalence of PL-ASA and IR-ASA at both dose levels. The results of these analyses are presented in Table 2. Analysis of the PK endpoints showed that the 90% CIs for the mean log-transformed salicylic acid parameters AUC0−t, AUC0–∞ and Cmax for the ratio PL-ASA to IR-ASA at both the 325 mg and 650 mg dose levels were within the FDA-accepted bioequivalence range of 80% to 125%. All 90% CIs contained 100% at both dose levels, indicating that nearly the same amount of salicylic acid was metabolized by each subject.
Analysis of the acetylsalicylic acid PK parameters for bioequivalence demonstrated that the 90% CIs for the mean log-transformed acetylsalicylic acid ratio for AUC0−t and AUC0–∞ were within the 80% to 125% range were within the 80% to 125% range at both dose levels (Table 2), but the 90% CI for Cmax was outside the range at both dose levels.
A total of 32 subjects were randomized. All but two subjects, both in the 325 mg dose group, were crossed over to the second study drug. Three additional subjects, one in the 325 mg dose group and two in the 650 mg dose group, were excluded from PK assessments because of the inability to confirm assigned dosing in these subjects. Demographics of the study population are provided in Online Table 2. No serious adverse events (AE) were reported during the study; only 1 AE was reported ('flu syndrome'), in the PL-ASA group, graded as mild severity and considered be unrelated to the study drug. Vital signs and laboratory results were unremarkable.
Pharmacodynamic results
To establish pharmacodynamic equivalence between PL-ASA and IR-ASA we compared parameters related to COX-1 activity and platelet aggregation. Thromboxane B2 (TXB2), a downstream product and established surrogate for TXA2 production, was measured. The mean concentration over time following dosing with PL-ASA and IR-ASA were shown to be similar (Fig. 2). In addition, Cmin (TxB2) values for both PL-ASA and IR-ASA were below 3.1 ng/mL (the cut-off associated with a decreased occurrence of major adverse cardiovascular events in patients taking aspirin for cardioprotection), suggesting that PL-ASA and IR-ASA could be considered functionally and clinically equivalent.
Graphs of the mean concentration of TxB2. Decrease in TxB2 level from baseline was measured as a marker for inhibition of platelet aggregation by PL-ASA and IR-ASA (samples collected at baseline, and 2, 4, 6, 8, 10, and 24 h post-dose). Results are shown as mean % inhibition of TxB2 concentration for 325 mg (top panel) and 650 mg dose (bottom panel). h hours, IR-ASA immediate release aspirin, mg milligrams, mL milliliters, ng nanograms, PL-ASA pharmaceutical lipid–aspirin complex, TxB2 thromboxane B2
The PD parameters AUC0-24, Imax, and tmax based on the percent inhibition of serum TxB2 levels for PL-ASA and IR-ASA were very similar, with identical Imax and tmax medians at both dose levels (Online Table 4). The 90% CIs for the mean log-transformed parameters AUC0–24 and Imax were within the accepted 80% to 125% bioequivalence interval at both dose levels. All the 90% CIs contained 100%, indicating little variation present in the percent inhibition of TxB2 levels observed among subjects. In addition, all subjects evaluable for this TxB2-related primary endpoint demonstrated at least 99% inhibition of baseline TxB2 levels, for both PL-ASA and IR-ASA at both dose levels, and were classified as aspirin responders (Online Table 5).
Levels of urinary 11-dehydro-TxB2, a stable metabolite of TxB2, also indicated a similar and high incidence of aspirin responders for both formulations (subjects having ≤ 1500 pg urinary 11-dehydro-TxB2 per mg of creatinine). Urinary 11-dehydro-TxB2 assay results showed that 85.7% of subjects were responders to IR-ASA and 78.6% were responders to PL-ASA at 325 mg doses; 100.0% responded to IR-ASA and 93.8% to PL-ASA at 650 mg doses.
In platelet-rich plasma from subjects at baseline, and 6 and 24 h after PL-ASA or IR-ASA treatment at either dose level (Fig. 3), platelet aggregation induced by arachidonic acid was inhibited more than 99% compared to that observed in pre-treatment blood samples. When the same assay was used to measure collagen-induced platelet aggregation (a distinct process in the early stages of in vivo plaque-formation at the site of vascular damage), collagen-induced aggregation was inhibited to a lesser degree than arachidonic acid-induced aggregation. There were no statistically significant differences between the effects of PL-ASA and IR-ASA at the same dose and time point, except in the 6-h samples after dosing at 325 mg, where inhibition of platelet aggregation was greater with PL-ASA (44.0% vs. 10.2%, p < 0.01), a difference that was no longer present at 24 h (34.3% vs. 32.9, p = ns).
Mean Percent Inhibition of Platelet Aggregation (IR-ASA and PL-ASA doses of 325 mg and 650 mg). The baseline levels of platelet aggregation induced by arachidonic acid and by collagen in platelet-rich plasma (PRP) prepared from blood samples collected at screening were determined. Platelet aggregation induced by each agonist was then measured in PRP prepared from blood drawn at 6 h and at 24 h after dosing, and the % inhibition of aggregation observed was calculated for each subject at each time point (compared to baseline). *P < 0.01. AA arachidonic acid, h hours, IR-ASA immediate release aspirin, PL-ASA pharmaceutical lipid–aspirin complex
Discussion
PL-ASA is a novel, pharmaceutical lipid-aspirin formulation administered in liquid-filled capsules, which was developed specifically to mitigate disruption of the epithelial phospholipid layer of the gastric mucosa and prevent direct gastric injury while still providing fast and complete absorption [13, 18]. The results of this PK/PD and bioequivalence study in healthy volunteers for PL-ASA compared with traditional IR-ASA can be summarized as follows:
(1) PK PL-ASA and IR-ASA have similar PK profiles, with the 90% CIs for the mean log-transformed salicylic acid PK parameters within the bioequivalence acceptance interval for both the 325 mg and the 650 mg dose levels. PK parameters for plasma acetylsalicylic acid levels were within the 80% to 125% bioequivalence range at the 325 mg dose level; at the 650 mg dose, only the 90% CIs for the mean log-transformed acetylsalicylic acid parameters AUC0−t and AUC0–∞ were within the that range. Differences in PK parameters reflected a difference in the rate of absorption between PL-ASA and IR-ASA dosing, likely due to differences between the capsule/tablet disintegration rates of PL-ASA capsules and IR-ASA tablets. Because acetylsalicylic acid is rapidly converted to salicylic acid by hydrolysis and first-pass metabolism, peak plasma concentrations of acetylsalicylic acid are extremely sensitive to minor variations in solid dosage form dissolution and disintegration. In contrast, plasma concentrations of salicylic acid are predictable and relatively stable compared with acetylsalicylic acid, and thus salicylic acid is considered to be a superior analyte for comparative bioequivalence assessments. Overall, these PK findings support that PL-ASA is bioequivalent to IR-ASA.
(2) PD PL-ASA and IR-ASA have similar profiles at the 325 mg and 650 mg dose levels. All evaluable subjects for TxB2 levels experienced at least 99% inhibition by both drugs at both dose levels, clearly meeting the threshold of 95% inhibition of serum TxB2 suggested as an indication of complete aspirin responsiveness [15]. Cmin(TxB2) values for both PL-ASA and IR-ASA are below 3.1 ng/mL, a cut-off associated with a decreased occurrence of major adverse cardiovascular events in patients taking aspirin for cardiovascular protection [17]. PD equivalence was further supported by the observation of complete inhibition of arachidonic acid-induced platelet aggregation following both PL-ASA and IR-ASA administration at both dose levels.
Regarding inhibition of collagen-induced platelet aggregation, PL-ASA exhibited a higher inhibition rate than IR-ASA at 6 h post-dosing. Inhibition rates were similar for PL-ASA and IR-ASA at 24 h post-dosing. Our observations on the enhanced degree of collagen-induced aggregation with PL-ASA 325 mg at 6 h are likely play of chance given that the level of inhibition was even greater than with PL-ASA 650 mg and not observed in other investigations (data on file, PLXPharma). Thus, PL-ASA demonstrated overall anti-platelet activity equivalent to that of IR-ASA.
(3) Safety PL-ASA was shown to be safe; only 1 unrelated, mild AE was reported during the study; no serious AEs; and no clinically significant vital sign or laboratory abnormalities occurred.
Aspirin-induced GI toxicity is an important side effect associated with both short and long-term use of aspirin [19]. These observations have prompted investigations aimed at developing aspirin formulations with greater tolerability, such as enteric coated tablets [20]. However, enteric coating is known to delay and impair drug absorption and contribute to variability in PK/PD profiles [21,22,23,24,25]. PL-ASA is a novel formulation of aspirin, specifically developed to mitigate disruption of the epithelial phospholipid layer of the gastric mucosa without delaying absorption. PL-ASA has been shown to reduce acute gastric mucosal lesion formation during short-term exposure when compared with IR-ASA [18]. Moreover, PL-ASA is an immediate-release formulation. In fact, the present analyses of the plasma concentration profiles of aspirin and its metabolite salicylic acid confirms that PL-ASA behaves as an immediate release formulation in fasted healthy volunteers. We have previously demonstrated that the pharmacokinetics of PL-ASA are also similar to those of IR-ASA in an obese diabetic population [13]. Overall, a new aspirin formulation characterized by improved safety and comparable efficacy with IR-ASA can be very appealing for both the acute and chronic management of patients with vascular disease. In the acute setting, the favorable safety profile of PL-ASA and its prompt absorption are indeed characteristics that are highly desirable in patients presenting with acute coronary syndromes or ischemic stroke who will likely also be treated with additional antithrombotic agents, hence increasing risk of GI bleeding, but who also require immediate and effective antiplatelet therapy. In the chronic setting, reliable platelet inhibition coupled with better tolerability due to reduced GI toxicity can improve patient adherence and provide better long-term protection from recurrent events.
Study limitations
The present bioequivalence study was conducted in healthy volunteers who did not have an indication to be treated with aspirin. This is consistent with standard guidance for FDA-required bioequivalence studies in order to allow for pure pharmacologic comparisons without the risk of interaction or interference by underlying clinical conditions. In addition, such bioequivalence studies are also not designed nor meant to test for clinical outcomes. However, the information derived from this study serves as a foundation to inform additional studies in specific patient populations that do have an indication to be treated with aspirin. It may be questioned why reporting of these early data supporting bioequivalence of PL-ASA with IR-ASA has occurred after publication of other reports on PL-ASA. Following FDA approval of PL-ASA, the prioritization shifted to studies focusing on antiplatelet activity (efficacy) and gastrointestinal toxicity (safety). However, in light of ongoing development of an 81 mg formulation and the upcoming commercial availability of both doses, investigators felt that publication of all prior data with PL-ASA and especially the data that supported FDA approval was very important.
Conclusions
Administration of a single dose of PL-ASA at 325-mg or 650-mg is safe, and pharmacokinetically and pharmacodynamically equivalent to IR-ASA based on log-transformed ratios for AUC0−t, AUC0–∞, and Cmax of plasma salicylic acid and for AUC0-24 and Imax of the percent inhibition of serum TxB2 levels. The findings of this study demonstrate that PL-ASA is both bioequivalent to aspirin for non-prescription indications, and pharmacodynamically equivalent to aspirin for physician-directed cardiovascular indications. The previously reported improved endoscopic safety profile of PL-ASA coupled with its pharmacologic efficacy equivalent to IR-ASA may potentially result in an improved benefit-risk profile. Further studies are warranted to test the performance of PL-ASA versus enteric-coated aspirin, the aspirin preferred by the majority of physicians and patients.
References
Patrono C (1994) Aspirin as an antiplatelet drug. N Engl J Med 330:1287–1294
Patrono C, Garcia Rodriguez LA, Landolfi R, Baigent C (2005) Low-dose aspirin for the prevention of atherothrombosis. N Engl J Med 353:2373–2383
Antithrombotic Trialists' (ATT) Collaboration (2009) Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 73:1849–1860
Abdelaziz HK, Saad M, Pothineni NVK et al (2019) Aspirin for primary prevention of cardiovascular events. J Am Coll Cardiol 73:2915–2929
Raber I, McCarthy CP, Vaduganathan M (2019) The rise and fall of aspirin in the primary prevention of cardiovascular disease. Lancet 393:2155–2167
García Rodríguez LA, Hernández-Díaz S, de Abajo FJ et al (2001) Association between aspirin and upper gastrointestinal complications: systematic review of epidemiologic studies. Br J Clin Pharmacol 52:563–571
Lanas A, García-Rodríguez LA, Arroyo MT et al (2006) Risk of upper gastrointestinal ulcer bleeding associated with selective cyclo-oxygenase-2 inhibitors, traditional non-aspirin non-steroidal anti-inflammatory drugs, aspirin and combinations. Gut 55:1731–1738
Pratt S, Thompson VJ, Elkin EP, Næsdal J, Sörstadius E (2010) The impact of upper gastrointestinal symptoms on nonadherence to, and discontinuation of, low-dose acetylsalicylic acid in patients with cardiovascular risk. Am J Cardiovasc Drugs 10:281–288
Davenport HW (1965) Damage to the gastric mucosa: Effects of salicylates and stimulation. Gastroenterology 49:189–196
Cryer B, Mahaffey KW (2014) Dose of aspirin in the treatment and prevention of cardiovascular disease: current and future directions. J Multidiscip Healthcare 7:137–146
Lichtenberger LM, Wang ZM, Romero JJ et al (1995) Non-steroidal anti-inflammatory drugs (NSAIDs) associate with zwitterionic phospholipids: Insight into the mechanism and reversal of NSAID-induced gastrointestinal injury. Nat Med 1:154–158
Darling RL, Romero JJ, Dial EJ, Akunda JK, Langenbach R, Lichtenberger LM (2004) The effects of aspirin on gastric mucosal integrity, surface hydrophobicity, and prostaglandin metabolism in cyclooxygenase knockout mice. Gastroenterology 127:94–104
Bhatt DL, Grosser T, Dong JF et al (2017) Enteric coating and aspirin nonresponsiveness in patients with type 2 diabetes mellitus. J Am Coll Cardiol 69:603–612
Polli JE, Abrahamsson BS, Yu LX et al (2008) Summary workshop report: bioequivalence, biopharmaceutics classification system, and beyond. AAPS J 10:373–379
Patrono C, Ciabattoni G, Pinca E, Pugliese F, Castrucci G, De Salvo A, Satta MA, Peskar BA (1980) Low dose aspirin and inhibition of thromboxane B2 production in healthy subjects. Thromb Res 17:317–327
Catella F, Healy D, Lawson J, FitzGerald GA (1986) 11-Dehydrothromboxane B2: a quantitative index of thromboxane A2 formation in the human circulation. Proc Natl Acad Sci USA 83:5861–5865
Frelinger AL III, Li Y, Linden MD et al (2009) Association of cyclooxygenase-1-dependent and -independent platelet function assays with adverse clinical outcomes in aspirin-treated patients presenting for cardiac catheterization. Circulation 120:2586–2596
Cryer B, Bhatt DL, Lanza FL, Dong JF, Lichtenberger LM, Marathi UK (2011) Low-dose aspirin-induced ulceration is attenuated by aspirin-phosphatidylcholine: A randomized clinical trial. Am J Gastroenterol 106:272–277
García Rodríguez LA (2001) HernándezDiaz S, De Abajo FJ Association between aspirin and upper gastrointestinal complications: systematic review of epidemiological studies. Br J Clin Pharmacol 52:563–571
Lanza FL, Royer GL Jr, Nelson RS (1980) Endoscopic evaluation of the effects of aspirin, buffered aspirin, and enteric-coated aspirin on gastric and duodenal mucosa. N Engl J Med 303:136–138
Bogentoft C, Carlsson I, Ekenved G, Magnusson A (1978) Influence of food on the absorption of acetylsalicylic acid from enteric-coated dosage forms. Eur J Clin Pharmacol 14:351–355
Grosser T, Fries S, Lawson JA, Kapoor SC, Grant GR, FitzGerald GA (2013) Drug resistance and pseudoresistance: an unintended consequence of enteric coating aspirin. Circulation 127:377–385
Bhatt DL (2004) Aspirin resistance: more than just a laboratory curiosity. J Am Coll Cardiol 43:1127–1129
Bhatt DL (2008) Resisting the temptation to oversimplify antiplatelet resistance. JACC Cardiovasc Interv 1:660–662
McKee SA, Sane DC, Deliargyris EN (2017) Aspirin resistance in cardiovascular disease: a review of prevalence, mechanisms, and clinical significance. Thromb Haemost 88:711–715
Acknowledgements
We are grateful to Francis Rack and the other clinical staff at Houston Institute for Clinical Research, a Phase I clinic where the current study was conducted, and to Angie Woodley, Baylor College of Medicine for conducting the platelet aggregation assays.
Funding
Plx Pharma was the study sponsor. The study was also partially supported by Grant Number R42DK063882 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive And Kidney Diseases or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Angiolillo declares that he has received consulting fees or honoraria from Amgen, Aralez, AstraZeneca, Bayer, Biosensors, Boehringer Ingelheim, Bristol-Myers Squibb, Chiesi, Daiichi-Sankyo, Eli Lilly, Haemonetics, Janssen, Merck, PhaseBio, PLx Pharma, Pfizer, Sanofi, and The Medicines Company and has received payments for participation in review activities from CeloNova and St Jude Medical. D.J.A. also declares that his institution has received research grants from Amgen, AstraZeneca, Bayer, Biosensors, CeloNova, CSL Behring, Daiichi-Sankyo, Eisai, Eli Lilly, Gilead, Idorsia, Janssen, Matsutani Chemical Industry Co., Merck, Novartis, Osprey Medical, and Renal Guard Solutions. Dr. Deepak L. Bhatt discloses the following relationships—Advisory Board: Cardax, Cereno Scientific, Elsevier Practice Update Cardiology, Medscape Cardiology, PhaseBio, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care, TobeSoft; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic (including for the ExCEED trial, funded by Edwards), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo), Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Vice-Chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees), HMP Global (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Medtelligence/ReachMD (CME steering committees), Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Abbott, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, Forest Laboratories, Idorsia, Ironwood, Ischemix, Lilly, Medtronic, PhaseBio, Pfizer, Regeneron, Roche, Sanofi Aventis, Synaptic, The Medicines Company; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); Site Co-Investigator: Biotronik, Boston Scientific, St. Jude Medical (now Abbott), Svelte; Trustee: American College of Cardiology; Unfunded Research: FlowCo, Fractyl, Merck, Novo Nordisk, PLx Pharma, Takeda. Dr Cryer is a consultant for Horizon Pharma, PLx Pharma, and Ritter. Pharmaceuticals.Dr. Jeske is the principal investigator on a research grant to Loyola University Chicago from KinMaster Produtos Quimicos and has been a consultant to PLx Pharma Inc., Machaon Diagnostics, and Repros Therapeutics. Dr. Deliargyris, Mr, Zimmerman, and Ms, von Chong are employees of PLx Pharma. Dr. Prats is a consultant to PLx Pharma. Dr. Marathi was an employee of PLx Pharma at the time of the study, and is an investor, option holder, and a co-inventor of the PL-ASA delivery technology. All other authors report no conflicts related to the current study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Angiolillo, D.J., Bhatt, D.L., Lanza, F. et al. Pharmacokinetic/pharmacodynamic assessment of a novel, pharmaceutical lipid–aspirin complex: results of a randomized, crossover, bioequivalence study. J Thromb Thrombolysis 48, 554–562 (2019). https://doi.org/10.1007/s11239-019-01933-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-019-01933-7