Abstract
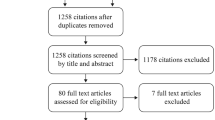
Background More than 30 years since it was developed for clinical use, the third-generation cephalosporin ceftriaxone remains the most commonly used agent for outpatient parental antimicrobial therapy (OPAT). Recent antimicrobial stewardship programmes have tended to restrict ceftriaxone use in hospitals to control antibiotic resistance and outbreaks of Clostridium difficle infection (CDI). Considering the expansion of OPAT programmes both in the UK and worldwide, revisiting the role of ceftriaxone in OPAT in the context of changing antimicrobial prescribing practices is timely. Aim of the review To identify the evidence base for OPAT, review current and historical data on indications for, and safety of ceftriaxone within the OPAT setting, and to provide some perspectives on the future role of ceftriaxone. Method We searched PubMed and Scopus for articles published in English, and hand searched reference lists. We also conducted a complementary descriptive analysis of prospectively acquired data on the use of ceftriaxone in more than 1,300 OPAT episodes over a 10-year period in our UK centre. Results Ceftriaxone has an excellent safety profile in the OPAT setting, and its broad spectrum of activity makes it an established agent in a wide range of clinical infection syndromes, such as skin and soft-tissue infection, bone and joint infection, streptococcal endocarditis and several others. Intriguingly, in contrast to the inpatient setting, liberal use of ceftriaxone in OPAT has not been strongly linked to CDI, suggesting additional patient and environmental factors may be important in mediating CDI risk.

Similar content being viewed by others
References
Newton GG, Abraham EP, Cephalosporin C. a new antibiotic containing sulphur and D-alpha-aminoadipic acid. Nature. 1955;175(4456):548.
Abraham EP. Cephalosporins 1945–1986. Drugs. 1987;34(Suppl 2):1–14.
Reiner R, Weiss U, Brombacher U, Lanz P, Montavon M, Furlenmeier A, et al. Ro 13-9904/001, a novel potent and long-acting parenteral cephalosporin. J Antibiot (Tokyo). 1980;33(7):783–6.
Esposito S. Parenteral cephalosporin therapy in ambulatory care: advantages and disadvantages. Drugs. 2000;59(Suppl 3):19–28. (discussion 47–49).
Esposito S, Noviello S, Leone S, Tice A, Seibold G, Nathwani D, et al. Outpatient parenteral antibiotic therapy (OPAT) in different countries: a comparison. Int J Antimicrob Agents. 2004;24(5):473–8.
Paladino JA, Poretz D. Outpatient parenteral antimicrobial therapy today. Clin Infect Dis. 2010;51(Suppl 2):S198–208.
Eron LJ, Park CH, Hixon DL, Goldenberg RI, Poretz DM. Ceftriaxone therapy of bone and soft tissue infections in hospital and outpatient settings. Antimicrob Agents Chemother. 1983;23(5):731–7.
Poretz DM. Outpatient parenteral antibiotic therapy. Int J Antimicrob Agents. 1995;5(1):9–12.
Bernstein Hahn L, Barclay CA, Iribarren MA, Traballi CA. Ceftriaxone, a new parenteral cephalosporin, in the treatment of urinary tract infections. Chemotherapy. 1981;27(Suppl 1):75–9.
Eichmann A, Weidmann G, Havas L. One-dose treatment of acute uncomplicated gonorrhoea of male patients with ceftriaxone Ro 13-9904, a new parenteral cephalosporin. A dose-range finding pilot study using doses of 500, 250, 125 and 50 mg respectively, in descending order. Chemotherapy. 1981;27(Suppl 1):62–9.
Baumgartner JD, Glauser MP. Single daily dose treatment of severe refractory infections with ceftriaxone. Cost savings and possible parenteral outpatient treatment. Arch Intern Med. 1983;143(10):1868–73.
Handsfield HH, Murphy VL. Comparative study of ceftriaxone and spectinomycin for treatment of uncomplicated gonorrhoea in men. Lancet. 1983;2(8341):67–70.
Poretz DM, Woolard D, Eron LJ, Goldenberg RI, Rising J, Sparks S. Outpatient use of ceftriaxone: a cost-benefit analysis. Am J Med. 1984;77(4C):77–83.
Tice AD. Once-daily ceftriaxone outpatient therapy in adults with infections. Chemotherapy. 1991;37(Suppl 3):7–10.
Tice AD. International outpatient parenteral antimicrobial therapy. Int J Clin Pract Suppl. 2000;115:26.
Torok ME, Chapman AL, Lessing MP, Sanderson F, Seaton RA. Outpatient parenteral antimicrobial therapy: recent developments and future prospects. Curr Opin Investig Drugs. 2010;11(8):929–39.
Russo TA, Cook S, Gorbach SL. Intramuscular ceftriaxone in home parenteral therapy. Antimicrob Agents Chemother. 1988;32(9):1439–40.
Chapman AL, Dixon S, Andrews D, Lillie PJ, Bazaz R, Patchett JD. Clinical efficacy and cost-effectiveness of outpatient parenteral antibiotic therapy (OPAT): a UK perspective. J Antimicrob Chemother. 2009;64(6):1316–24.
Caplan GA, Ward JA, Brennan NJ, Coconis J, Board N, Brown A. Hospital in the home: a randomised controlled trial. Med J Aust. 1999;170(4):156–60.
Corwin P, Toop L, McGeoch G, Than M, Wynn-Thomas S, Wells JE, et al. Randomised controlled trial of intravenous antibiotic treatment for cellulitis at home compared with hospital. Bmj. 2005;330(7483):129.
Shepperd S, Doll H, Angus RM, Clarke MJ, Iliffe S, Kalra L, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2008;(4):CD007491.
Nathwani D, Tice A. Ambulatory antimicrobial use: the value of an outcomes registry. J Antimicrob Chemother. 2002;49(1):149–54.
Wynn M, Dalovisio JR, Tice AD, Jiang X. Evaluation of the efficacy and safety of outpatient parenteral antimicrobial therapy for infections with methicillin-sensitive Staphylococcus aureus. South Med J. 2005;98(6):590–5.
Matthews PC, Conlon CP, Berendt AR, Kayley J, Jefferies L, Atkins BL, et al. Outpatient parenteral antimicrobial therapy (OPAT): is it safe for selected patients to self-administer at home? A retrospective analysis of a large cohort over 13 years. J Antimicrob Chemother. 2007;60(2):356–62.
Esposito S, Leone S, Noviello S, Ianniello F, Fiore M, Russo M, et al. Outpatient parenteral antibiotic therapy for bone and joint infections: an Italian multicenter study. J Chemother. 2007;19(4):417–22.
Mackintosh CL, White HA, Seaton RA. Outpatient parenteral antibiotic therapy (OPAT) for bone and joint infections: experience from a UK teaching hospital-based service. J Antimicrob Chemother. 2011;66(2):408–15.
Gesser RM, McCarroll KA, Woods GL. Evaluation of outpatient treatment with ertapenem in a double blind controlled clinical trial of complicated skin/skin structure infections. J Infect. 2004;48(1):32–8.
Rehm S, Campion M, Katz DE, Russo R, Boucher HW. Community-based outpatient parenteral antimicrobial therapy (CoPAT) for Staphylococcus aureus bacteraemia with or without infective endocarditis: analysis of the randomized trial comparing daptomycin with standard therapy. J Antimicrob Chemother. 2009;63(5):1034–42.
Amodeo MR, Clulow T, Lainchbury J, Murdoch DR, Gallagher K, Dyer A, et al. Outpatient intravenous treatment for infective endocarditis: safety, effectiveness and one-year outcomes. J Infect. 2009;59(6):387–93.
Seaton RA, Bell E, Gourlay Y, Semple L. Nurse-led management of uncomplicated cellulitis in the community: evaluation of a protocol incorporating intravenous ceftriaxone. J Antimicrob Chemother. 2005;55(5):764–7.
Seaton RA, Sharp E, Bezlyak V, Weir CJ. Factors associated with outcome and duration of therapy in outpatient parenteral antibiotic therapy (OPAT) patients with skin and soft-tissue infections. Int J Antimicrob Agents. 2011;38(3):243–8.
Nathwani D. The management of skin and soft tissue infections: outpatient parenteral antibiotic therapy in the United Kingdom. Chemotherapy. 2001;47(Suppl 1):17–23.
Tice AD. Pharmacoeconomic considerations in the ambulatory use of parenteral cephalosporins. Drugs. 2000;59(Suppl 3):29–35. (discussion 47–49).
Eron LJ, Goldenberg RI, Poretz DM. Combined ceftriaxone and surgical therapy for osteomyelitis in hospital and outpatient settings. Am J Surg. 1984;148(4A):1–4.
Mauceri AA. Treatment of bone and joint infections utilizing a third-generation cephalosporin with an outpatient drug delivery device. HIAT Study Group. Am J Med. 1994;97(2A):14–22.
Tice AD, Hoaglund PA, Shoultz DA. Risk factors and treatment outcomes in osteomyelitis. J Antimicrob Chemother. 2003;51(5):1261–8.
Francioli PB. Ceftriaxone and outpatient treatment of infective endocarditis. Infect Dis Clin North Am. 1993;7(1):97–115.
Francioli P, Etienne J, Hoigne R, Thys JP, Gerber A. Treatment of streptococcal endocarditis with a single daily dose of ceftriaxone sodium for 4 weeks. Efficacy and outpatient treatment feasibility. JAMA. 1992;267(2):264–7.
Cervera C, del Rio A, Garcia L, Sala M, Almela M, Moreno A, et al. Efficacy and safety of outpatient parenteral antibiotic therapy for infective endocarditis: a ten-year prospective study. Enferm Infecc Microbiol Clin. 2011;29(8):587–92.
Larioza J, Heung L, Girard A, Brown RB. Management of infective endocarditis in outpatients: clinical experience with outpatient parenteral antibiotic therapy. South Med J. 2009;102(6):575–9.
Popescu GA. The long journey of outpatient parenteral antibiotic therapy in infective endocarditis: from idea to clinical guidelines. South Med J. 2009;102(6):559–60.
Tice AD. Safety of outpatient parenteral antimicrobial therapy for endocarditis. Clin Infect Dis. 2002;34(3):419–20.
Monteiro CA, Cobbs CG. Outpatient management of infective endocarditis. Curr Infect Dis Rep. 2001;3(4):319–27.
Andrews MM, von Reyn CF. Patient selection criteria and management guidelines for outpatient parenteral antibiotic therapy for native valve infective endocarditis. Clin Infect Dis. 2001;33(2):203–9.
Steele RW. Ceftriaxone therapy of meningitis and serious infections. Am J Med. 1984;77(4C):50–3.
Martin E. Once-daily administration of ceftriaxone in the treatment of meningitis and other serious infections in children. Eur J Clin Microbiol. 1983;2(5):509–15.
Faella F, Pagliano P, Fusco U, Attanasio V, Conte M. Combined treatment with ceftriaxone and linezolid of pneumococcal meningitis: a case series including penicillin-resistant strains. Clin Microbiol Infect. 2006;12(4):391–4.
O’Connell S. Lyme borreliosis: current issues in diagnosis and management. Curr Opin Infect Dis. 2010;23(3):231–5.
Ljostad U, Skogvoll E, Eikeland R, Midgard R, Skarpaas T, Berg A, et al. Oral doxycycline versus intravenous ceftriaxone for European Lyme neuroborreliosis: a multicentre, non-inferiority, double-blind, randomised trial. Lancet Neurol. 2008;7(8):690–5.
Mogabgab WJ. Single-dose oral temafloxacin versus parenteral ceftriaxone in the treatment of gonococcal urethritis/cervicitis. Am J Med. 1991;91(6A):145S–9S.
Reusser P, Serex P. Outpatient treatment of gonorrhea with ceftriaxone. J Chemother. 1989;1(4 Suppl):895–6.
Collier AC, Judson FN, Murphy VL, Leach LA, Root CJ, Handsfield HH. Comparative study of ceftriaxone and spectinomycin in the treatment of uncomplicated gonorrhoea in women. Am J Med. 1984;77(4C):68–72.
Chisholm SA, Alexander S, Desouza-Thomas L, Maclure-Webster E, Anderson J, Nichols T, et al. Emergence of a Neisseria gonorrhoeae clone showing decreased susceptibility to cefixime in England and Wales. J Antimicrob Chemother. 2011;66(11):2509–12.
Carannante A, Prignano G, Cusini M, Matteelli A, Dal Conte I, Ghisetti V, et al. Cefixime and ceftriaxone susceptibility of Neisseria gonorrhoea in Italy from 2006 to 2010. Clin Microbiol Infect. 2011.
Martin I, Jayaraman G, Wong T, Liu G, Gilmour M. Trends in antimicrobial resistance in Neisseria gonorrhoeae isolated in Canada: 2000–2009. Sex Transm Dis. 2011;38(10):892–8.
Butler T. Treatment of typhoid fever in the 21st century: promises and shortcomings. Clin Microbiol Infect. 2011;17(7):959–63.
Beeching NJ, Parry CM. Outpatient treatment of patients with enteric fever. Lancet Infect Dis. 2011;11(6):419–21.
White B, Coia JE, Sykes C, Mather H, Seaton RA. Enteric fever in returning travellers: role of outpatient parenteral antibiotic therapy. J Infect. 2012;64(2):242–5.
Fekety FR. Safety of parenteral third-generation cephalosporins. Am J Med. 1990;88(4A):38S–44S.
Bijie H, Kulpradist S, Manalaysay M, Soebandrio A. In vitro activity, pharmacokinetics, clinical efficacy, safety and pharmacoeconomics of ceftriaxone compared with third and fourth generation cephalosporins: review. J Chemother. 2005;17(1):3–24.
Lamb HM, Ormrod D, Scott LJ, Figgitt DP. Ceftriaxone: an update of its use in the management of community-acquired and nosocomial infections. Drugs. 2002;62(7):1041–89.
Boggs SR, Cunnion KM, Raafat RH. Ceftriaxone-induced hemolysis in a child with lyme arthritis: a case for antimicrobial stewardship. Pediatrics. 2011;128(5):e1289–92.
Kapur G, Valentini RP, Mattoo TK, Warrier I, Imam AA. Ceftriaxone induced hemolysis complicated by acute renal failure. Pediatr Blood Cancer. 2008;50(1):139–42.
Imam SN, Wright K, Bhoopalam N, Choudhury A. Hemolytic anemia from ceftriaxone in an elderly patient: a case report. J Am Med Dir Assoc. 2008;9(8):610–1.
Goyal M, Donoghue A, Schwab S, Hasbrouck N, Khojasteh S, Osterhoudt K. Severe hemolytic crisis after ceftriaxone administration. Pediatr Emerg Care. 2011;27(4):322–3.
Andersohn F, Konzen C, Garbe E. Systematic review: agranulocytosis induced by nonchemotherapy drugs. Ann Intern Med. 2007;146(9):657–65.
Duncan CJ, Evans TJ, Seaton RA. Ceftriaxone-related agranulocytosis during outpatient parenteral antibiotic therapy. J Antimicrob Chemother. 2010;65(11):2483–4.
Patel R, Grogg KL, Edwards WD, Wright AJ, Schwenk NM. Death from inappropriate therapy for Lyme disease. Clin Infect Dis. 2000;31(4):1107–9.
Zishka PA, Douglas JM Jr. Immediate hypersensitivity reaction to single-dose parenteral ceftriaxone therapy for gonorrhea. Sex Transm Dis. 1991;18(1):26–7.
Pichichero ME. Use of selected cephalosporins in penicillin-allergic patients: a paradigm shift. Diagn Microbiol Infect Dis. 2007;57(3 Suppl):13S–8S.
Rienstra M, Bonten MJ, Gaillard CA. Ceftriaxone-associated biliary pseudolithiasis. Neth J Med. 2009;67(3):113–4.
Karakitsos D, Poularas J, Samonis G, Karabinis A. Ceftriaxone-associated reversible biliary sludge in a critical care patient. Acta Anaesthesiol Scand. 2008;52(8):1171–2.
Martin E, Fanconi S, Kalin P, Zwingelstein C, Crevoisier C, Ruch W, et al. Ceftriaxone-bilirubin-albumin interactions in the neonate: an in vivo study. Eur J Pediatr. 1993;152(6):530–4.
Mohkam M, Karimi A, Gharib A, Daneshmand H, Khatami A, Ghojevand N, et al. Ceftriaxone associated nephrolithiasis: a prospective study in 284 children. Pediatr Nephrol. 2007;22(5):690–4.
Kimata T, Kaneko K, Takahashi M, Hirabayashi M, Shimo T, Kino M. Increased urinary calcium excretion caused by ceftriaxone: possible association with urolithiasis. Pediatr Nephrol. 2012;27(4):605–9.
Owens RC Jr, Donskey CJ, Gaynes RP, Loo VG, Muto CA. Antimicrobial-associated risk factors for Clostridium difficile infection. Clin Infect Dis. 2008;46(Suppl 1):S19–31.
Kuntz JL, Chrischilles EA, Pendergast JF, Herwaldt LA, Polgreen PM. Incidence of and risk factors for community-associated Clostridium difficile infection: a nested case-control study. BMC Infect Dis. 2011;11:194.
Barr DA, Semple L, Seaton RA. Outpatient parenteral antimicrobial therapy (OPAT) in a teaching hospital-based practice: a retrospective cohort study describing experience and evolution over 10 years. Int J Antimicrob Agents. 2012;39(5):407-13.
Schirmer PL, Deresinski SC. Ceftobiprole: a new cephalosporin for the treatment of skin and skin structure infections. Expert Rev Anti Infect Ther. 2009;7(7):777–91.
Laudano JB. Ceftaroline fosamil: a new broad-spectrum cephalosporin. J Antimicrob Chemother. 2011;66(Suppl 3):iii11–iii18.
Struelens MJ, Monnet DL. Prevention of methicillin-resistant Staphylococcus aureus infection: is Europe winning the fight? Infect Control Hosp Epidemiol. 2010;31(Suppl 1):S42–4.
Acknowledgments
CJAD is supported by a Wellcome Trust Research Training Fellowship.
Funding
None.
Conflicts of interest
RAS has previously received speaker fees, consultancy and research funding from Novartis and Pfizer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duncan, C.J.A., Barr, D.A. & Seaton, R.A. Outpatient parenteral antimicrobial therapy with ceftriaxone, a review. Int J Clin Pharm 34, 410–417 (2012). https://doi.org/10.1007/s11096-012-9637-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-012-9637-z