Abstract
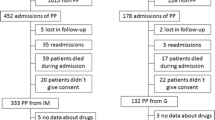
Objective The aims of the present study were to: analyse the prevalence of polypharmacy in a group of older patients; evaluate the influence of hospital stay on the number of drugs taken; assess the most frequently prescribed pharmacological classes; identify risk factors that predisposed the patient to polypharmacy. Setting The study was carried out in the Department of Internal Medicine of a non-university general hospital. Method In the retrospective study, 600 patients aged 65 years or more were enrolled. They were hospitalised in the period from 1st December 2003 to 31st March 2005. Each person taking six or more medications per day was considered to be a patient with polypharmacy. Particular sociodemographic and clinical characteristics, as well as comorbid conditions, were evaluated as factors potentially influencing the prevalence of polypharmacy. Main outcome measure The number and type of medications taken at the time of hospital admission and discharge were recorded and compared for each patient. Results Polypharmacy on admission and at discharge was observed in 362 (60.3%) and 374 (62.3%) patients, respectively. Hospitalisation led to a significant increase in the number of medications. The spectrum of medications used corresponded to the proportions of diagnoses in the evaluated group, in which cardiovascular diseases were most prevalent. According to the multivariate analysis using a logistic regression model, diabetes mellitus (odds ratio (OR) 2.40; 95% confidence interval (CI): 1.64–3.50), heart failure (OR 2.14; 95% CI: 1.46–3.14), dementia (OR 2.12; 95% CI: 1.26–3.57), living alone (OR 2.00; 95% CI: 1.28–3.10), arterial hypertension (OR 1.63; 95% CI: 1.08–2.44) and cerebrovascular disease (OR 1.58; 95% CI: 1.03–2.44) significantly increased the risk of the presence of polypharmacy. Conclusion Our study confirmed a relatively high prevalence of polypharmacy in Slovak elderly patients. Polypharmacy risk rose especially with the increased prevalence of diseases of advancing age (diabetes mellitus, heart failure, arterial hypertension, dementia and cerebrovascular diseases). The increasing numbers of medications in inpatients indicate the need for the careful re-evaluation of pharmacotherapy during the stay in hospital.

Similar content being viewed by others
References
Onder G, Pedone C, Landi F, Cesari M, Della Vedova C, Bernabei R, et al. Adverse drug reactions as cause of hospital admissions: results from the Italian Group of Pharmacoepidemiology in the Elderly (GIFA). J Am Geriatr Soc 2002;50:1962–8.
Koh Y, Fatimah BM, Li SC. Therapy related hospital admission in patients on polypharmacy in Singapore: a pilot study. Pharm World Sci 2003;25:135–7.
van der Hooft CS, Sturkenboom MCJ, van Grootheest K, Kingma HJ, Stricker BH. Adverse drug reaction-related hospitalisations: a nationwide study in the Netherlands. Drug Saf 2006;29:161–8.
Bressler R, Bahl JJ. Principles of drug therapy for the elderly patient. Mayo Clin Proc 2003;78:1564–77.
Annual Health Report of the Slovak Republic 2003. The Institute of Health Information and Statistics (UZIS), 2004. Home page at http://www.uzis.sk/
Census of inhabitants, houses and flats 2001. Statistical Office of the Slovak Republic, 2002. home page at http://www.statistics.sk/
Foltán V, Tesař T (eds) Lieky. Lieková politika. Farmakoekonomika (Drugs. Drug policy. Pharmacoeconomics). Bratislava: Propact, 2003. ISBN 80-968963-0-1.
Hoven JL, Haaijer-Ruskamp FM, Vander Stichele RH. Indicators of prescribing quality in drug utilisation research: report of a European meeting (DURQUIM, 13–15 May 2004). Eur J Clin Pharmacol 2005;60:831–4.
Wawruch M, Zikavska M, Wsolova L, Jezova D, Fialova D, Kunzo M, et al. Perception of potentially inappropriate medication in elderly patients by Slovak physicians. Pharmacoepidemiol Drug Saf 2006;15:829–34.
ICD-10. International Statistical Classification of Diseases and Related Health Problems, 10th Revision. Geneva: World Health Organization (WHO), 1992. ISBN 92-4154419-8.
Veehof LJG, Stewart RE, Haaijer-Ruskamp FM, Meyboom-de Jong B. The development of polypharmacy. A longitudinal study. Fam Pract 2000;17:261–7.
Williamson J, Chopin JM. Adverse reactions to prescribed drugs in the elderly: a multicentre investigation. Age Ageing 1980;9:73–80.
ATC/DDD index 2006. World Health Organization (WHO), 2006. Home page at http://www.whocc.no/
Veehof LJG, Meyboom-de Jong B, Haaijer-Ruskamp FM. Polypharmacy in the elderly—a literature review. Eur J Gen Pract 2000;6:98–106.
Newman SC. Biostatistical methods in epidemiology. Chichester, UK: Wiley; 2001. ISBN 0-471-36914-4.
Hanlon JT, Schmader KE, Ruby CM, Weinberger M. Suboptimal prescribing in older inpatients and outpatients. J Am Geriatr Soc 2001;49:200–9.
Viktil KK, Enstad M, Kutschera J, Smedstad LM, Schjott J. Polypharmacy among patients admitted to hospital with rheumatic diseases. Pharm World Sci 2001;23:153–8.
Jyrkkä J, Vartiainen L, Hartikainen S, Sulkava R, Enlund H. Increasing use of medicines in elderly persons: a five-year follow-up of the Kuopio 75+ Study. Eur J Clin Pharmacol 2006;62:151–8.
Linjakumpu T, Hartikainen S, Klaukka T, Veijola J, Kivela SL, Isoaho R. Use of medications and polypharmacy are increasing among the elderly. J Clin Epidemiol 2002;55:809–17.
Vinks THAM, de Koning FHP, de Lange TM, Eqberts TCG. Identification of potential drug-related problems in the elderly: the role of the community pharmacist. Pharm World Sci 2006;28:33–8.
Bjerrum L, Søgaard J, Hallas J, Kragstrup J. Polypharmacy: correlations with sex, age and drug regimen. Eur J Clin Pharmacol 1998;54:197–202.
Jörgensen T, Johansson S, Kennerfalk A, Wallander M-A, Svardsudd K. Prescription drug use, diagnoses, and healthcare utilization among the elderly. Ann Pharmacother 2001;35:1004–9.
Nobili A, Tettamanti M, Frattura L, Spagnoli A, Ferraro L, Marrazzo E, et al. Drug use by the elderly in Italy. Ann Pharmacother 1997;31:416–22.
Smith SC Jr, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update. Endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol 2006;47:2130–9.
van Dijk KN, de Vries CS, van den Berg PB, Brouwers JR, de Jong-van den Berg LT. Drug utilisation in Dutch nursing homes. Eur J Clin Pharmacol 2000;55:765–71.
Flicker L, Grimley Evans G. Piracetam for dementia or cognitive impairment. Cochrane Database Syst Rev 2001;2:CD001011.
Ricci S, Celani MG, Cantisani AT, Righetti E. Piracetam for acute ischaemic stroke. Cochrane Database Syst Rev 2006;2:CD000419.
Viola R, Csukonyi K, Doró P, Janka Z, Soós G. Reasons for polypharmacy among psychiatric patients. Pharm World Sci 2004;26:143–7.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The JNC7 report. JAMA 2003;289:2560–72.
Swedberg K, Cleland J, Dargie H, Drexler H, Follath F, Komajda M, et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005). Eur Heart J 2005;26:1115–40.
Fialová D, Topinková E, Gambassi G, Finne-Soveri H, Jónsson PV, Carpenter I, et al. Potentially inappropriate medication use among elderly home care patients in Europe. JAMA 2005;293:1348–58.
Onder G, Landi F, Liperoti R, Fialova D, Gambassi G, Bernabei R. Impact of inappropriate drug use among hospitalized older adults. Eur J Clin Pharmacol 2005;61:453–59.
Koopmans RTCM, van der Borgh JP, Bor JHJ, Hekster YA. Increase in drug use after admission to Dutch nursing homes. Pharm World Sci 2003;25:30–4.
George J, Pfleger D, McCaig D, Bond C, Stewart D. Independent prescribing by pharmacists: a study of the awareness, views and attitudes of Scottish community pharmacists. Pharm World Sci 2006;28:45–53.
Hobson RJ, Sewell GJ. Risks and concerns about supplementary prescribing: survey of primary and secondary care pharmacists. Pharm World Sci 2006;28:76–90.
Acknowledgements
We thank Dr. Katarina Kahayova and Dr. Peter Kruty, director of the general hospital in Povazska Bystrica, for assisting us in carrying out this study.
Funding The present study was supported by grants VEGA 0343, 0314 and the European Social Fund. Conflicts of interest None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wawruch, M., Zikavska, M., Wsolova, L. et al. Polypharmacy in elderly hospitalised patients in Slovakia. Pharm World Sci 30, 235–242 (2008). https://doi.org/10.1007/s11096-007-9166-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-007-9166-3