Abstract
Intrathecal application of liposomal cytarabine (Ara-C) (DepoCyte®) has been associated with neurotoxicity when applied as part of a polychemotherapy regimen. Patients with primary central nervous system lymphoma treated with high-dose systemic methotrexate (MTX)- and Ara-C-based polychemotherapy including six cycles of liposomal Ara-C (50 mg intrathecally every 3 weeks) were prospectively monitored for neurotoxic side-effects. Between November 2005 and February 2009, 149 intrathecal applications of liposomal cytarabine (DepoCyte®) were carried out in 33 patients, 7 (21%) of whom developed an incomplete conus medullaris/cauda equina syndrome with incontinence for bladder (6) and bowel function (3) or lumbosacral polyradicular paresis (1), resolving only incompletely over a follow-up period of 9–30 months. In six of these seven patients, lumbosacral magnetic resonance imaging (MRI) was negative for leptomeningeal infiltration or arachnoiditis. Cerebrospinal fluid (CSF) analysis performed in six of these seven patients showed normal cell count in all and increased total protein in four of them. One patient among these seven suffered a seizure without other identifiable causes. Conus/cauda syndrome has to be considered as a serious potential neurotoxic side-effect in patients receiving liposomal Ara-C as part of a multimodal regimen including high-dose systemic MTX and Ara-C.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphomas (PCNSL) are extranodal diffuse non-Hodgkin lymphomas (NHL), primarily of B-cell type, involving brain, meninges, spinal cord and eyes with no systemic manifestation [1, 15]. Prognosis of PCNSL has been poor, with median survival of 12–18 months in patients treated with whole-brain radiotherapy (WBRT) alone [16]. High-dose methotrexate (MTX)-based chemotherapy protocols in combination with or without WBRT [5, 18] have extended mean survival up to several years. In a multicentre pilot/phase II study evaluating systemic MTX- and cytarabine (Ara-C)-based polychemotherapy and intraventricular triple therapy (MTX, Ara-C, prednisolone) via Ommaya reservoir, median overall survival was 50 months and durable response could be achieved in about 50% of patients younger than 60 years of age [10]. However, Ommaya reservoir infections in nearly 20% of these patients hampered the good results of this study [18]. Since local chemotherapy of the cerebrospinal fluid compartment is not standard in PCNSL and in order to prevent Ommaya reservoir-related complications, intraventricular treatment was omitted in a consecutive phase II study in patients up to 60 years of age, not modifying systemic chemotherapy otherwise. However, study accrual was prematurely stopped in November 2005 due to a high rate of early relapse without intrathecal chemotherapy [17]. Therefore, we assumed that cerebrospinal fluid might serve as a reservoir for surviving tumour cells and that efficient treatment of the leptomeninges might be essential to prevent early tumour relapse in PCNSL [17]. To sustain long-term treatment responses, but to avoid Ommaya reservoir infections, intraventricular triple therapy was replaced by intrathecal liposomal Ara-C (DepoCyte®) applied via lumbar puncture once during each treatment course in a consecutive multicentre trial activated in November 2005 (details of the protocol are shown in Table 1).
Liposomal Ara-C is a slow-release formulation of Ara-C produced by encapsulating the aqueous drug solution in spherical multivesicular particles. Ara-C is gradually released from these particles into the cerebrospinal fluid, resulting in prolonged drug exposure approximately 40 times longer than standard Ara-C [3, 11]. In patients with lymphomatous or neoplastic meningitis, liposomal Ara-C once every 2 weeks turned out not to be inferior with regard to efficacy compared with the standard formulation of free Ara-C twice a week for 1 month [6, 9]. Glantz et al. [6] could show a statistically significant higher response rate of DepoCyte® compared with conventional (free) intrathecal Ara-C. Liposomal Ara-C has been applied in patients with diverse leptomeningeal cancers as treatment or prophylaxis in several series [4, 12, 20].
Here we report on toxicity associated with intrathecal liposomal Ara-C treatment in combination with a systemic high-dose MTX- and high-dose Ara-C-based chemotherapy protocol for PCNSL.
Patients and methods
Patients
Between November 2005 and February 2009, 33 patients (median age 65 years, range 32–76 years) with histologically proven PCNSL were prospectively monitored for toxicity of liposomal Ara-C (DepoCyte®) administered intrathecally. Twenty-five of these 33 patients had been enrolled in a phase II trial evaluating primary chemotherapy without radiotherapy in immunocompetent patients. Treatment consisted of a high-dose MTX- (MTX; cycles 1, 2, 4, 5) and Ara-C-based (ARA-C; cycles 3, 6) systemic therapy (including dexamethasone, vinca-alkaloids, ifosfamide and cyclophosphamide) and was combined with intrathecal liposomal Ara-C application. The protocol is presented in Table 1. Additionally, eight patients were treated with the same protocol but were not included in the trial because they did not fulfil the inclusion criteria (n = 7) or they had come under our observation prior to inclusion of this centre in the multicentre trial (n = 1).
Liposomal Ara-C (DepoCyte®, 50 mg) was administered intrathecally via lumbar puncture once during each cycle. Dexamethasone was given to all patients orally at a dosage of at least 4 mg twice daily for five consecutive days to prevent arachnoiditis, beginning on the day of liposomal Ara-C administration. A sample of cerebrospinal fluid (CSF) was taken prior to each intrathecal application of liposomal Ara-C to investigate cell count, total protein, lactate and cytological examination as well as microbiological analysis in case of pleocytosis. Each patient was studied by contrast-enhanced MRI of the brain within 72 h prior to initiation of the therapy protocol, after completion of the second chemotherapy cycle and of the whole therapy. MRI of the thoracolumbar spine was additionally performed in case of neurological symptoms indicative of arachnoiditis, i.e. incomplete conus/cauda syndrome or severe lumbosacral pain. Neurologic examinations were performed prior to each dose of intrathecal liposomal Ara-C. Toxicities were recorded according to version 2 of the National Cancer Institute common toxicity criteria (CTC) for peripheral neurotoxicity [CTC grade I: loss of deep tendon reflexes or paraesthesia (including tingling) but not interfering with function; CTC grade II: objective sensory loss or paraesthesia (including tingling), interfering with function, but not interfering with activities of daily living; CTC grade III: sensory loss or paraesthesia interfering with activities of daily living; CTC grade IV: permanent sensory loss that interferes with function].
Results
Study population and treatment
Thirty-three patients (14 men, 19 women) were prospectively monitored for systemic toxicity and neurotoxic side-effects. Median age was 65 years (range 32–76 years). Median Karnofsky performance score at diagnosis was 70 (range 30–100). Intrathecal liposomal Ara-C was administered for six treatment courses in 16 patients (48%), five courses in 6 patients (18%), four courses in 1 patient (3%), three courses in 3 patients (9%), two courses in 3 patients (9%) and one single course in 4 patients (12%). In total, 149 liposomal Ara-C applications were given via lumbar puncture (median 5 applications, range 1–6). Reasons for omitting intrathecal liposomal Ara-C were as follows: Due to a space-occupying cerebellar lymphoma manifestation, DepoCyte® was not administered during the first cycle in one patient. In two patients, one treatment course was finished prematurely before scheduled DepoCyte® application for infectious complications during treatment. One patient showed progressive disease during the last chemotherapy cycle, and therapy was stopped before liposomal Ara-C application. One patient received liposomal Ara-C only during the fifth and sixth cycle, after having been switched from a systemic protocol alone to the treatment regimen including intrathecal treatment (outside the trial). One patient received the first course of chemotherapy without intrathecal therapy due to a protocol violation.
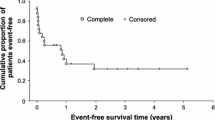
Neurotoxicity
Neurotoxic side-effects in association with liposomal Ara-C administration occurred in eight patients (24%). Seven patients (21%) suffered from an incomplete conus/cauda syndrome with incontinence for bladder (six) and bowel function (three) or lumbosacral polyradicular paresis (one), in two of those associated with lumbosacral pain making opioid therapy necessary. One patient of these seven suffered from a single generalized tonic clonic epileptic seizure without any other identifiable cause, 6 days after the fifth intrathecal administration of Ara-C. One patient experienced repetitive episodes of severe transient lumbosacral pain after the second cycle, then at each cycle after intrathecal therapy. Neurotoxic side-effects occurred at different time points in these eight patients, the earliest being after the second intrathecal administration of liposomal Ara-C, the last being even 5 months after completion of therapy. In general, neurotoxicity after liposomal Ara-C given intrathecally occurred late during treatment, in four patients after five intrathecal administrations of liposomal Ara-C, in three patients after six cycles. For further details see Table 2. In all patients affected by symptoms other than just pain, symptoms resolved only incompletely over a follow-up period of 9–30 months. In six of these seven patients with an incomplete conus/cauda syndrome, MRI scans of the lumbosacral spine were negative for leptomeningeal infiltration or arachnoiditis, as e.g. leptomeningeal thickening or contrast enhancement. CSF analysis was performed in six patients, without increased cell count but with slightly increased total protein of up to 66 mg/dl (normal range up to 45 mg/dl) in four cases.
Eight further patients of this series showed asymptomatic pleocytosis at routine CSF examination prior to i.t. application of DepoCyte® with maximum cell count of 50/μl and increased total protein up to 102 mg/dl.
Discussion
The aim of this case series was to observe and examine patients for neurologic symptoms after treatment with intrathecal liposomal Ara-C, which was part of a polychemotherapy regimen based on high-dose MTX and Ara-C for patients with PCNSL. The advantages of intrathecally administered liposomal Ara-C for treatment or prophylaxis of leptomeningeal tumour are its pharmacokinetics and its easy administration route [4, 6, 19]. Immediate serious neurotoxicity had not been observed [3, 6]. However, severe lumbosacral pain may follow intrathecal drug application within days, in particular when steroids are not given [3]. Single cases of sustained, severe and even life-threatening or lethal neurologic complications have been reported by some authors recently [7, 8, 13].
Limited experience exists with concomitant treatment of intrathecal liposomal Ara-C and systemic high-dose MTX- and Ara-C-based chemotherapy. Jabbour and co-workers reported significant neurotoxicity associated with liposomal Ara-C (dose 50 mg) given prophylactically in combination with high-dose MTX and Ara-C to patients with newly diagnosed acute lymphocytic leukaemia (ALL) in 5 of 31 patients (16%), including seizures, papilloedema, cauda equina syndrome (n = 2) and progressive encephalitis leading to death [8]. In another report six patients underwent allogeneic haematopoietic stem cell transplantation (HSCT) due to haematologic malignancies (ALL, acute myeloic leukaemia (AML), Burkitt’s lymphoma) and were treated with liposomal Ara-C for prophylaxis (two) and treatment (four) of neoplastic meningitis: two patients experienced sacral radiculopathy, one with an irreversible cauda equina syndrome [7]. Among nine children under 4 years of age treated with liposomal Ara-C for malignant brain tumours (doses between 20 and 35 mg) neurological side-effects were seen in five (56%), including “irritability” during 24 h following each dose in one and chemical arachnoiditis in two. One patient experienced seizures after the fourth intrathecal treatment and one patient sacral radiculopathy with irreversible cauda equina syndrome [13]. Serious side-effects in 6 out of 19 older children and adolescents with recurrent or refractory brain tumours treated with intrathecal liposomal Ara-C and concomitant systemic radiochemotherapy included chemical arachnoiditis (vomiting, headache, fever), leading to cessation of treatment in two of four patients. One of these two patients experienced seizures 16 days after the seventh intrathecal administration. Lethargy, memory problems, ataxia and slurred speech were observed in two other patients [2]. In contrast, McClune et al. reported mostly minor neurologic side-effects using liposomal Ara-C for CNS prophylaxis in adults with acute lymphatic leukaemia. Liposomal Ara-C 50 mg was given to 14 patients through an Ommaya reservoir once per cycle of a hyper-cyclophosphamide, vincristine, doxorubicine, dexamethasone (CVAD) regimen. After one patient developed hyponatraemia and somnolence, the dose was reduced to 25 mg. During a 18-month follow-up, no relevant side-effects led to termination of therapy [14].
In this series, during the course of treatment or even months after completion of therapy, a long-lasting incomplete conus/cauda syndrome, consisting of urinary and/or faecal incontinence, impairment of perianal sensibility and/or lumbosacral pain, developed in eight patients (24%). In line with other reports [7, 8], the findings presented here support the assumption that combination of systemic high-dose MTX and Ara-C with intrathecal liposomal Ara-C is particularly associated with a high risk of developing a sustained conus/cauda syndrome, even though all of our patients had been treated with dexamethasone as arachnoiditis prophylaxis. Leptomeningeal involvement by the tumour itself or infectious complications were excluded as alternative explanations by MRI and CSF investigations. Therefore, this unexpectedly frequent neurotoxic side-effect has to be attributed to the neurotoxic potential of the chemotherapeutics. Symptoms resolved only incompletely even at a follow-up period of up to 30 months after therapy. Thus, occurrence of a conus/cauda syndrome may be a consequence of the cumulative dose of systemic and intrathecal chemotherapy. Systemic high-dose MTX and Ara-C results in cytotoxic CNS concentrations, and ifosfamide is able to cross the blood–brain barrier as well. This condition may increase the neurotoxic potential of liposomal Ara-C. With the exception of two individuals, patients of this series affected by “delayed” conus/cauda syndrome did not experience severe immediate lumbosacral pain after intrathecal liposomal Ara-C application, supporting the view that a cumulative toxic and not inflammatory mechanism might mediate this disturbance.
Referring to CTC for peripheral neurotoxicity, incontinence of bladder and bowel function is not listed, but should be categorized as grade III toxicity. Furthermore, this complication could occur even months after completion of therapy, so a long follow-up period is necessary.
It should be considered that there is a special risk of this complication being overlooked, since some older patients, women in particular, did not spontaneously complain of incontinence, because they felt ashamed of this symptom. Therefore, special continuous questioning is necessary to detect an evolving cauda equina syndrome as soon as possible. In conclusion, irreversible or only partially reversible cauda equina syndrome has to be recognized as a relevant disabling adverse event after intrathecal liposomal Ara-C in combination with systemic high-dose MTX- and Ara-C-based chemotherapy, long-lasting in a follow-up time up to 30 months.
References
Batchelor T, Loeffler JS (2006) Primary CNS lymphoma. J Clin Oncol 24:1281–1288
Benesch M, Siegler N, Hoff K, Lassay L, Kropshofer G, Muller H, Sommer C, Rutkowski S, Fleischhack G, Urban C (2009) Safety and toxicity of intrathecal liposomal cytarabine (Depocyte) in children and adolescents with recurrent or refractory brain tumors: a multi-institutional retrospective study. Anticancer Drugs 20:794–799
Chamberlain MC, Kormanik P, Howell SB, Kim S (1995) Pharmacokinetics of intralumbar DTC-101 for the treatment of leptomeningeal metastases. Arch Neurol 52:912–917
Garcia-Marco JA, Panizo C, Garcia ES, Deben G, Alvarez-Larran A, Barca EG, Sancho JM, Penarrubia MJ, Garcia-Cerecedo T, Garcia Vela JA (2009) Efficacy and safety of liposomal cytarabine in lymphoma patients with central nervous system involvement from lymphoma. Cancer 115:1892–1898
Gavrilovic IT, Hormigo A, Yahalom J, DeAngelis LM, Abrey LE (2006) Long-term follow-up of high-dose methotrexate-based therapy with and without whole brain irradiation for newly diagnosed primary CNS lymphoma. J Clin Oncol 24:4570–4574
Glantz MJ, LaFollette S, Jaeckle KA, Shapiro W, Swinnen L, Rozental JR, Phuphanich S, Rogers LR, Gutheil JC, Batchelor T, Lyter D, Chamberlain M, Maria BL, Schiffer C, Bashir R, Thomas D, Cowens W, Howell SB (1999) Randomized trial of a slow-release versus a standard formulation of cytarabine for the intrathecal treatment of lymphomatous meningitis. J Clin Oncol 17:3110–3116
Hilgendorf I, Wolff D, Junghanss C, Kahl C, Leithaeuser M, Steiner B, Casper J, Freund M (2008) Neurological complications after intrathecal liposomal cytarabine application in patients after allogeneic haematopoietic stem cell transplantation. Ann Hematol 87:1009–1012
Jabbour E, O’Brien S, Kantarjian H, Garcia-Manero G, Ferrajoli A, Ravandi F, Cabanillas M, Thomas DA (2007) Neurologic complications associated with intrathecal liposomal cytarabine given prophylactically in combination with high-dose methotrexate and cytarabine to patients with acute lymphocytic leukemia. Blood 109:3214–3218
Jaeckle KA, Batchelor T, O’Day SJ, Phuphanich S, New P, Lesser G, Cohn A, Gilbert M, Aiken R, Heros D, Rogers L, Wong E, Fulton D, Gutheil JC, Baidas S, Kennedy JM, Mason W, Moots P, Russell C, Swinnen LJ, Howell SB (2002) An open label trial of sustained-release cytarabine (DepoCyt) for the intrathecal treatment of solid tumor neoplastic meningitis. J Neurooncol 57:231–239
Juergens A, Pels H, Rogowski S, Fliessbach K, Glasmacher A, Engert A, Reiser M, Diehl V, Vogt-Schaden M, Egerer G, Schackert G, Reichmann H, Kroschinsky F, Bode U, Herrlinger U, Linnebank M, Deckert M, Fimmers R, Schmidt-Wolf IG, Schlegel U (2010) Long-term survival with favorable cognitive outcome after chemotherapy in primary central nervous system lymphoma. Ann Neurol 67:182–189
Kim S, Chatelut E, Kim JC, Howell SB, Cates C, Kormanik PA, Chamberlain MC (1993) Extended CSF cytarabine exposure following intrathecal administration of DTC 101. J Clin Oncol 11:2186–2193
Kripp M, Hofheinz RD (2008) Treatment of lymphomatous and leukemic meningitis with liposomal encapsulated cytarabine. Int J Nanomed 3:397–401
Lassaletta A, Lopez-Ibor B, Mateos E, Gonzalez-Vicent M, Perez-Martinez A, Sevilla J, Diaz MA, Madero L (2009) Intrathecal liposomal cytarabine in children under 4 years with malignant brain tumors. J Neurooncol 95:65–69
McClune B, Buadi FK, Aslam N, Przepiorka D (2007) Intrathecal liposomal cytarabine for prevention of meningeal disease in patients with acute lymphocytic leukemia and high-grade lymphoma. Leuk Lymphoma 48:1849–1851
Morris PG, Abrey LE (2009) Therapeutic challenges in primary CNS lymphoma. Lancet Neurol 8:581–592
Nelson DF (1999) Radiotherapy in the treatment of primary central nervous system lymphoma (PCNSL). J Neurooncol 43:241–247
Pels H, Juergens A, Glasmacher A, Schulz H, Engert A, Linnebank M, Schackert G, Reichmann H, Kroschinsky F, Vogt-Schaden M, Egerer G, Bode U, Schaller C, Lamprecht M, Hau P, Deckert M, Fimmers R, Bangard C, Schmidt-Wolf IG, Schlegel U (2009) Early relapses in primary CNS lymphoma after response to polychemotherapy without intraventricular treatment: results of a phase II study. J Neurooncol 91:299–305
Pels H, Schmidt-Wolf IG, Glasmacher A, Schulz H, Engert A, Diehl V, Zellner A, Schackert G, Reichmann H, Kroschinsky F, Vogt-Schaden M, Egerer G, Bode U, Schaller C, Deckert M, Fimmers R, Helmstaedter C, Atasoy A, Klockgether T, Schlegel U (2003) Primary central nervous system lymphoma: results of a pilot and phase II study of systemic and intraventricular chemotherapy with deferred radiotherapy. J Clin Oncol 21:4489–4495
Phuphanich S, Maria B, Braeckman R, Chamberlain M (2007) A pharmacokinetic study of intra-CSF administered encapsulated cytarabine (DepoCyt) for the treatment of neoplastic meningitis in patients with leukemia, lymphoma, or solid tumors as part of a phase III study. J Neurooncol 81:201–208
Rueda Dominguez A, Olmos Hidalgo D, Viciana Garrido R, Torres Sanchez E (2005) Liposomal cytarabine (DepoCyte) for the treatment of neoplastic meningitis. Clin Transl Oncol 7:232–238
Disclosures
Drs. Pels and Schlegel have received honoraria from Mundipharma and ESSEX-Pharma. Dr. Schlegel has received honoraria from Sigma Tau.
Author information
Authors and Affiliations
Corresponding author
Additional information
Kathrin Ostermann and Hendrik Pels contributed equally.
Rights and permissions
About this article
Cite this article
Ostermann, K., Pels, H., Kowoll, A. et al. Neurologic complications after intrathecal liposomal cytarabine in combination with systemic polychemotherapy in primary CNS lymphoma. J Neurooncol 103, 635–640 (2011). https://doi.org/10.1007/s11060-010-0435-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0435-y