Abstract
Conflicting results have been published on prognostic significance of central venous to arterial PCO2 difference (∆PCO2) after cardiac surgery. We compared the prognostic value of ∆PCO2 on intensive care unit (ICU) admission to an original algorithm combining ∆PCO2, ERO2 and lactate to identify different risk profiles. Additionally, we described the evolution of ∆PCO2 and its correlations with ERO2 and lactate during the first postoperative day (POD1). In this monocentre, prospective, and pilot study, 25 patients undergoing conventional cardiac surgery were included. Central venous and arterial blood gases were collected on ICU admission and at 6, 12 and 24 h postoperatively. High ∆PCO2 (≥ 6 mmHg) on ICU admission was found to be very frequent (64% of patients). Correlations between ∆PCO2 and ERO2 or lactate for POD1 values and variations were weak or non-existent. On ICU admission, a high ∆PCO2 did not predict a prolonged ICU length of stay (LOS). Conversely, a significant increase in both ICU and hospital LOS was observed in high-risk patients identified by the algorithm: 3.5 (3.0–6.3) days versus 7.0 (6.0–8.0) days (p = 0.01) and 12.0 (8.0–15.0) versus 8.0 (8.0–9.0) days (p < 0.01), respectively. An algorithm incorporating ICU admission values of ∆PCO2, ERO2 and lactate defined a high-risk profile that predicted prolonged ICU and hospital stays better than ∆PCO2 alone.
Similar content being viewed by others
1 Introduction
Tissue perfusion after cardiac surgery may become impaired due to multiple factors and in turn induce organ dysfunction, organ failure, prolonged stay in intensive care unit (ICU) and in hospital and increased mortality [1]. Unfortunately, the adequacy of tissue perfusion remains difficult to assess. Surrogate markers like central venous to arterial PCO2 difference (ΔPCO2), oxygen extraction ratio (ERO2) and lactate are used to evaluate this adequacy [2, 3]. Elevated arterial lactate is a commonly used marker of global anaerobic metabolism and even mild hyperlactatemia has recently found to be correlated both with microcirculatory flow abnormalities and a worse outcome [3,4,5]. However, lactate is not a pure marker of anaerobic metabolism and non-hypoxic causes of hyperlactatemia are common in septic shock or after cardiopulmonary bypass [6,7,8]. Accordingly, additional markers of tissue perfusion have been explored. ERO2 can be calculated on basis of oxygen arterial saturation (SaO2) and central venous saturation (ScvO2) using the following formula: ERO2 = (SaO2−ScvO2)/SaO2. Hemodynamic monitoring guidelines recommend to monitor this ratio after cardiac surgery and a ScvO2 ≥ 70% is often considered a target for optimal hemodynamic resuscitation [9, 10]. However, because of the potential extraction defect some patient might have microcirculatory impairment with a normal or supranormal ScvO2.
In this context ΔPCO2 has been proposed as a global marker of tissue perfusion adequacy [11,12,13]. ΔPCO2 is a marker of the venous blood flow ability to remove the excess CO2 produced in tissue. An impaired tissue perfusion, due to low cardiac output or microcirculatory alteration, is therefore the main determinant of an elevated ΔPCO2 [14].
Yet, the prognostic significance of ΔPCO2 after cardiac surgery remains unclear and conflicting results have been published [11, 15]. Moreover, limited prospectively reported data on ΔPCO2 after cardiopulmonary bypass (CPB) are available. Finally, in clinical practice ΔPCO2 and lactate or ERO2 values frequently appear contradictive, which makes the interpretation of an elevated ΔPCO2 difficult. Several authors already suggested that interpreting ΔPCO2 with ScvO2 improve the prognostic significance of these markers [11, 12, 16]. De Backer in a recent review on hemodynamic in shock suggests an algorithm combining ΔPCO2, ScvO2 and lactate [17]. This multiparametric approach could better discriminate different cardiovascular profiles and improve our understanding of apparently contradictive patterns. Still, no clinical study has yet evaluated algorithms combining these three markers following cardiac surgery.
In this pilot study, we evaluate the prognostic value of ΔPCO2 at the time of ICU admission and compare it to an original algorithm combining ΔPCO2, ERO2 and lactate to identify different risk profiles after elective conventional cardiac surgery. Additionally, we describe the evolution of ΔPCO2 and its correlations with ERO2 and lactate on the first post-operative day (POD1).
2 Materials and methods
2.1 Ethics
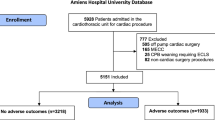
All adult patients scheduled for elective cardiac surgery with CPB were eligible for this monocentric, prospective, observational study, which was approved by the local Ethics Committee (Comité de Protection des Personnes, Reference CPP: A13-D55-VOL.19). According to French law and because data were collected during routine care, authorization was granted to waive written informed consent. However, verbal consent was obtained from all study participants before surgery. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
2.2 Study population
From April 2013 to June 2013, patients who were scheduled for cardiac surgery at Caen University Hospital, Caen, France, were eligible for participation in the study. Inclusion criteria were as follows:
Patients > 18 years old who were admitted to the surgical ICU following elective conventional cardiac surgery (Coronary artery bypass graft (CABG) and/or aortic or mitral valvular surgery) with CPB.
Exclusion criteria were age < 18 years or patient under tutorship, off pump surgery, cardiac transplantation, ventricular assist device implantation and any emergency situations.
2.3 Perioperative management
The anesthesia was standardized (target-controlled infusion of propofol and remifentanil) and adjusted to obtain a bispectral index value between 40 and 60. Immediately after the induction of general anesthesia and tracheal intubation in the operating room, a radial artery catheter and a right jugular central venous catheter were inserted. More advanced hemodynamic monitoring was left at the anesthetist’s discretion. Patients were ventilated at 6–8 mL kg−1 of ideal body weight, positive end expiratory pressure was set to 4–8 cm H2O. The ventilator was switched off during CPB. Anticoagulation was obtained during CPB with an initial bolus of heparin (300 UI kg−1) to maintain activated coagulation time more than 450 s. Reversion was systematically per- formed with protamine at the end of CPB. CPB was performed under normothermia and myocardial protection was achieved by intermittent cold blood cardioplegia. Boluses of ephedrine and/or phenylephrine were given intraoperatively to maintain mean arterial pressure between 50 and 80 mm Hg. The heart was defibrillated after aortic unclamping, if sinus rhythm did not resume spontaneously. After the termination of CPB, norepinephrine was used to maintain the mean arterial pressure greater than 65 mm Hg, and the trigger for transfusion of packed erythrocytes was set to a hematocrit of 21% in all patients and complied with routine practice at the study institution.
On arrival in the ICU, all pressure monitors were zeroed at the mid-axillary line upon arrival and the position of the tip of the central venous catheter in the upper part of the right atrium was verified by chest radiography. Discontinuation of invasive ventilation, administration of blood products, management of hemodynamics and fluid balance, ICU and hospital discharge followed institutional standards.
2.4 Data collection
Data elements included demographic variables: age, gender, body mass index (kg/m2), EuroSCORE 2 (%), baseline serum creatinine value (μmol/L); intra operative data: type of surgery, CPB time, Cross clamp time, use of epinephrine, norepinephrine or dobutamine, preoperative. The first blood sample was collected on admission to the ICU (T0) and 6 h (T6), 12 h (T12) and 24 h (T24) after. Venous and arterial blood gas were drawn simultaneously from radial arterial catheter and central venous catheter. Central venous and arterial lactate serum level, CO2 partial pressure, oxygen saturation and content were obtained from the blood gases. ΔPCO2 was calculated as PcvCO2 minus PaCO2. The patient’s heart rate, mean arterial pressure (MAP), central temperature and oxygen saturation were measured simultaneously to the blood samples. The primary outcome was ICU length of stay. At the ICU discharge, we also collected duration of mechanical ventilation, the need for epinephrine, norepinephrine or dobutamine on POD1 and total postoperative chest tube drainage. Secondary outcomes included Sequential Organ Failure Assessment (SOFA) score on POD1, acute kidney injury (AKI) on first and second post-operative day (POD1 and POD2) and hospital length of stay [18]. AKI was defined according to the Acute Kidney Injury Network criteria as stage 1 or higher (increase in peak postoperative serum creatinine level to > 150% or ≥ 26.5 μmol/L from baseline value) [19]. Hyperlactatemia was defined as an arterial lactate level above 1.5 mmol/L [4, 5]. We choose a ΔPCO2 > 6 mmHg to define an elevated ΔPCO2 and a normal ERO2 as a level of 30% or lower. These cutoff values were chosen according to previous studies [12, 13].
2.5 Description of the algorithm and definition of a high risk profile
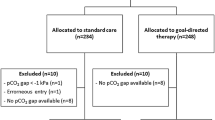
We constructed an algorithm combining ΔPCO2, ERO2 and lactate. This algorithm helped us identifying a low-risk profile and a high-risk profile (Fig. 1). In the algorithm, lactate elevation was considered a marker of global anaerobic metabolism in the presence of altered values of ΔPCO2 or ERO2. If ΔPCO2 and ERO2 were both normal, lactate elevation was considered to be non-hypoxic hyperlactatemia. ΔPCO2 elevation was considered to reflect low cardiac output (CO) in case of high ERO2 or microcirculatory dysfunction with impaired oxygen extraction if ERO2 was normal. An elevated ERO2 in presence of a normal ΔPCO2 was considered to reflect a decrease in DO2 non-related to a low CO (anemia, hypoxemia). Patients with global anaerobic metabolism, non-hypoxic hyperlactatemia or microcirculatory dysfunction with impaired oxygen extraction as determined by the algorithm were considered to have a high-risk profile. The ICU length of stay (LOS) of high-risk profile patients was then compared to the rest of the population.
Incidence of different hemodynamic pattern according to the proposed algorithm. nadm values on admission, ERO2 oxygen extraction ratio, ΔPCO2 central venous to arterial PCO2 difference, microcirc. microcirculation. Number (%). Overall, 13 (52%) patients had high-risk profile whereas 12 (48%) patients experienced a low-risk profile
2.6 Statistical analysis
The number of patients included in that pilot study was fixed empirically to 25. All data were tested for normal distribution with the Kolmogorov–Smirnov test. Normally distributed data were displayed as mean ± standard deviation and not normally distributed data were displayed as median with 25th percentile and 75th percentile. Comparisons were performed using Fisher’s exact test or Chi squared test for categorical data according to the distribution. Independent-samples T test was used to test the differences in normally distributed variables and Mann-Whithney U test for not normally distributed variables. Trends in the parameters over time in two groups were compared with repeated-measures ANOVA. Pairwise comparisons were corrected for multiple testing with the Bonferroni procedure. Pearson or Spearman correlation coefficients for data normally distributed and not normally distributed, respectively, were used to evaluate the relation between two variables. We analyzed correlation between values of the whole dataset and markers POD1 variations. To calculate markers POD1 variations we identified, among the whole dataset, the successive samples of Lactate, ΔPCO2 and ERO2 measured within 6 to 12 h intervals in a given patient and calculated the markers variations as following: Marker variation = 100% × (second marker value−initial marker value)/initial marker value. We used the log-rank test to compare the length of stay in ICU according to the patient risk group on admission. For all tests, a two-tailed P value less than 0.05 was considered significant. Statistical analyses were performed using R software (R Foundation for Statistical Computing 2016).
3 Results
Twenty-five consecutive adult patients were included in the study (52% CABG, 36% valvular surgery and 12% combined surgery). Baseline characteristics and surgery-related parameters in the whole cohort of patients and in both low- and high-risk groups are shown in Table 1. No significant difference was found between groups with the exception of the ICU LOS.
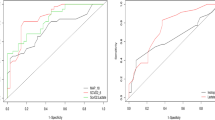
At the time of admission, 64% of the patients had elevated ΔPCO2 (Fig. 1). On POD1 a ΔPCO2 ≥ 6 mmHg was reported at least once in all patients. ΔPCO2 did not significantly decrease on POD1 and patients with high ΔPCO2 on admission did not have significantly different ΔPCO2 at T6, T12 and T24 compared with patients with normal ΔPCO2 (Fig. 2). Correlations between ΔPCO2 and lactate or ERO2 for POD1 values and variations are shown in Table 2. A weak correlation was found between ΔPCO2 and ERO2 both for POD1 absolute values (r = 0.41, p < 0.01) and variations (r = 0.46, p < 0.01). Correlation between ScvO2 and ERO2 was excellent (r = − 0.99, p < 0.01). Other correlations between markers were weak or non-significant (Table 2). ScvO2 was not significantly different in patients with normal or elevated ΔPCO2 (70 (63–74) % versus 65 (58–70) %, respectively, p = 0.1).
POD1 evolution of ΔPCO2 (a) and POD1 evolution of ΔPCO2 according to value on admission (b). ERO2 oxygen extraction ratio, ΔPCO2 central venous to arterial PCO2 difference. *Significant difference between groups with repeated-measures analysis of variance after Bonferroni correction. Time 0: admission to ICU
At the time of ICU admission an elevated ΔPCO2 did not predict prolonged ICU and hospital stays (Fig. 3a and b).
Length of stay in ICU stay according to ΔPCO2 alone (a) or according to risk group (ΔPCO2 in combination with ERO2 and lactate) (b) at the time of admission. ΔPCO2 central venous to arterial PCO2 difference, ICU intensive care unit. Patients with global anaerobic metabolism, non-hypoxic hyperlactatemia or microcirculatory dysfunction with impaired oxygen extraction as determined by the algorithm were considered to have a high-risk profile (Fig. 1). Patients with normal tissue perfusion or decreased oxygen delivery without anaerobic metabolism were considered to have low-risk profile
The algorithm combining ΔPCO2 with ERO2 and lactate identified 12 patients with a low-risk profile and 13 patients with a high-risk profile at the time of admission. Out of the 16 patients with elevated ΔPCO2 upon admission, 7 (43%) were classified as low-risk profile while 9 (57%) were identified as high-risk profile. Conversely, out of the 9 patients with low ΔPCO2 upon admission, 4 (44%) were identified as high-risk profile and 5 (56%) as low-risk profile. The precise incidence of the different hemodynamic patterns is further described in Fig. 1. Temperature on ICU admission was not different in patients with normal and elevated ΔPCO2 (36.5±0.5 °C vs. 36.5±0.5 °C respectively, p = 1.0) and between high and low risk groups (36.7±0.4 °C vs. 36.4±0.5 °C respectively, p = 0.1). The high-risk patient group at the time of admission had ICU LOS twice as long as those in the low-risk patient group. (Table 1 and Fig. 3c) Hospital length of stay was also significantly longer for patient in the high-risk group compared to the low risk group (12.0 (8.0–15.0) versus 8.0 (8.0–9.0) days respectively, p < 0.01). (Figure 3d) We found significantly more AKI in patients of the high-risk group compared to the low risk group ((4 (30%) vs. 0 (0%), respectively, p = 0.04) and serum creatinine on POD1 and POD2 were significantly higher (Table 1). All AKI were stage 1 according to the Acute Kidney Injury Network. Need for prolonged mechanical ventilation, inotropic support and SOFA on POD1 were not significantly different between groups (Table 1). The ICU LOS was not significantly different across patients with low or elevated lactate (5.0 (3.0–7.0) days versus 7.0 (6.0–8.0) days, respectively, p = 0.09) and/or low or elevated ERO2 (6.0 (5.0–7.5) days versus 6.5 (3.0–7.0) days, respectively, p = 0.60) at the time of admission.
4 Discussion
The main results of this prospective pilot study are as:
High ΔPCO2 (≥ 6 mmHg) on admission and on POD1 of conventional cardiac surgery was found to be very frequent and did not predict an elevated ΔPCO2 at T6, T12 or T24. Correlations between POD1 values and POD1 variations for ΔPCO2 and ERO2 or lactate were weak or non-existent.
At the time of admission an elevated ΔPCO2 alone did not predict a prolonged ICU stay. Conversely, ICU LOS increased by 2-fold in the high-risk patient group identified with the algorithm. High-risk patients also had significantly more postoperative AKI and longer hospital LOS.
Limited prospectively reported data on ΔPCO2 after CPB are available. As previously reported in retrospective studies, our prospective study demonstrates that a widening in ΔPCO2 on POD1 after conventional elective cardiac surgery is quite frequent [11, 15]. The reason why ΔPCO2 remains elevated on ICU admission and on POD1 is unclear. An adequate venous blood flow is the main contributor of ΔPCO2 and depends on both cardiac output and tissue perfusion [14, 20]. It has been demonstrated that ΔPCO2 after cardiac surgery is only poorly correlated to cardiac output or regional blood flow [21]. It has been suggested that impaired microcirculation could be responsible for the widening in ΔPCO2 especially when it is associated with normal ScvO2 [11, 12]. In these studies the pattern of a high ΔPCO2 with a normal ScvO2 was associated to further post-operative complications, impaired splanchnic function or elevated lactate. Yet, it is still uncertain whether a high ΔPCO2 after cardiac surgery is related to microcirculatory hypoperfusion and further studies are needed.
We found no strong correlations between ΔPCO2 and ERO2 or lactate, which is concordant with previous studies in the settings of cardiac surgery and septic shock [2, 15, 22,23,24]. This particular lack of strong correlation is not surprising, since ΔPCO2, ERO2 and lactate provide information on different hemodynamic mechanisms. For example, high lactate is a marker of global anaerobic metabolism whereas high ΔPCO2 indicates decreased blood flow that can occur without anaerobic metabolism [14]. Conversely, tissue hypoxia from non-ischemic cause will not be detected by ΔPCO2.but will induce a rise in lactate value [14]. Concerning ERO2, its elevation is a normal adaptation mechanism that can also occur without tissue hypoxia [1].
We did not find any significant prognostic value of an elevated ΔPCO2 at the time of admission. Similarly, ERO2 and lactate level taken alone at the time of admission did not predicted a prolonged ICU stay. It is important to not misinterpret these results. We underline that the prognostic value of hyperlactatemia or abnormal ERO2 after cardiac surgery has been demonstrated in several studies [3, 9, 22, 23]. Concerning ΔPCO2, an elevation ≥ 6 mmHg at admission has also been shown to be associated with poor prognosis in high surgical risk patients but the results are conflicting in cardiac surgery [11, 13, 15]. In a recent retrospective study, high ΔPCO2 after cardiac surgery was not associated with a worst outcome but the authors analyzed ΔPCO2 alone [15]. Conversely, Habicher et al. found that in presence of normal ScvO2 ≥ 70%, a high ΔPCO2 (ΔPCO2 ≥ 8 mmHg) was associated to further post-operative complications [11]. The combination of these two markers seem to better predict complications. Similarly, our study suggests that an algorithm combining ΔPCO2 with ERO2 and lactate improved prognostic signification of these markers at admission. Indeed, in our study, 43% of patients with high ΔPCO2 at the time of admission were classified as low-risk group and 44% patients with low ΔPCO2 were eventually categorized in the high-risk group. Consequently, we think that ΔPCO2, ERO2 and lactate should not be interpreted separately but together using an algorithm.
Our study population was at low risk according to the EuroSCORE 2 evaluation. However, when associating to this preoperative scoring system the ΔPCO2, ERO2 and lactate measures immediately at the ICU admission almost half of our population was eventually classified as high-risk group. Interestingly, although our study was lacking of power for prognosis evaluation, ICU and hospital stays were significantly longer and patients had more acute renal failure in the high-risk group compared to the low-risk group while their EuroSCORE 2 did not differ significantly. We think that our algorithm-based evaluation at the time of ICU admission may have led to the identification of clinically significant intraoperative complications.
The design of our interpretation algorithm is quite similar to the algorithm which was recently published by De Backer in a review on hemodynamic in shock [17]. Yet, some differences should be discussed. For example, De Backer considers hyperlactatemia with normal ERO2 and ΔPCO2 as a profile of high cardiac output with dysoxia (i.e. sepsis). In our algorithm we consider this pattern as non-hypoxic hyperlactatemia. Indeed, in the setting of cardiac surgery, the occurrence of hyperlactatemia without evidence of inadequate oxygen delivery (DO2) has been reported [7]. Although, the pathogenesis of this disorder remains unclear, according to the authors it should be considered as reflecting a type B lactic acidosis instead of an anaerobic metabolism. These patients with non-hypoxic hyperlactatemia were still considered as high risk. Indeed, an increased lactate level with a normal tension difference/arteriovenous O2 content difference ratio (ΔPCO2/ΔContO2; another anaerobic metabolism marker) was shown to be correlated to poor prognosis in a medical ICU [25]. Another difference of interpretation relates to the pattern of an increased ERO2 with normal lactatemia and ΔPCO2. Both our algorithm and De Backer’s findings agree on a decrease in DO2 but De Backer associates it with dysoxia while we consider a rise in ERO2 to be a normal adaptation mechanism [1]. Nevertheless, we regard both algorithms as useful tools for clinicians to improve comprehension of the patterns drawn by these routine markers of systemic perfusion. This study is the first to describe the incidence of the different hemodynamic profiles defined by these algorithms.
There are several limitations to our study. First, the circulatory profiles defined by the algorithm were not externally validated by, for example, a measurement of cardiac output and an evaluation of microcirculation by video microscopy. Further studies are needed to assess both macro and microcirculation in the suggested hemodynamic profiles. Another important limitation was the small size of the study population and the moderate severity of disease within it. We used central instead of mixed-venous blood to assess ERO2 and CO2 derived variables; our results may have differed if a pulmonary artery catheter (PAC) had been used [26]. However, PAC is no longer used in conventional cardiac surgery. Hypothermia is also a potential confounder for ΔPCO2 measurement. It may decrease cellular respiration and CO2 generation, especially for very low temperature [20]. Nevertheless none of our patients had profound hypothermia on ICU admission and normothermia was rapidly achieved for all of our patients. Finally, lactate, ΔPCO2 or ERO2 surely have different physiological kinetics, with the clearance of lactate probably slower than that of ERO2 and CO2 derived variables. This makes it difficult to interpret a snapshot of those markers. That being said, taking the kinetics variations of the markers into account would also be very difficult. We designed our algorithm to provide clinicians with an everyday tool for the interpretation of arterial and central venous blood gases, and it appears to correlate with a clinical reality as it predicts occurrence of post-operative AKI and longer ICU and hospital stays.
5 Conclusion
In this original pilot study on patients who underwent standard cardiac surgery high ΔPCO2 (≥ 6 mmHg) on admission and on POD1 of conventional cardiac surgery was found to be very frequent and high ΔPCO2 on admission did not predict an elevated ΔPCO2 at T6, T12 or T24. Correlations between POD1 values and POD1 variations for ΔPCO2 and ERO2 or lactate were weak or non-existent. An algorithm incorporating the ICU admission values of ΔPCO2, ERO2 and lactate defined a high-risk profile that predicted prolonged ICU and hospital stays better than ΔPCO2 alone.
References
Routsi C, Vincent JL, Bakker J, De Backer D, Lejeune P, d’Hollander A, et al. Relation between oxygen consumption and oxygen delivery in patients after cardiac surgery. Anesth Analg. 1993;77:1104–10.
Ariza M, Gothard JW, Macnaughton P, Hooper J, Morgan CJ, Evans TW. Blood lactate and mixed venous-arterial PCO2 gradient as indices of poor peripheral perfusion following cardiopulmonary bypass surgery. Intensive Care Med. 1991;17:320–4.
Maillet J-M, Le Besnerais P, Cantoni M, Nataf P, Ruffenach A, Lessana A, et al. Frequency, risk factors, and outcome of hyperlactatemia after cardiac surgery. Chest. 2003;123:1361–6.
Vellinga NAR, Boerma EC, Koopmans M, Donati A, Dubin A, Shapiro NI, et al. Mildly elevated lactate levels are associated with microcirculatory flow abnormalities and increased mortality: a microSOAP post hoc analysis. Crit Care Lond Engl. 2017;21:255.
Rishu AH, Khan R, Al-Dorzi HM, Tamim HM, Al-Qahtani S, Al-Ghamdi G, et al. Even mild hyperlactatemia is associated with increased mortality in critically ill patients. Crit Care Lond Engl. 2013;17:R197.
Rimachi R, de Carvahlo FB, Orellano-Jimenez C, Cotton F, Vincent JL, De Backer D. Lactate/pyruvate ratio as a marker of tissue hypoxia in circulatory and septic shock. Anaesth Intensive Care. 2012;40:427–32.
Raper RF, Cameron G, Walker D, Bowey CJ. Type B lactic acidosis following cardiopulmonary bypass. Crit Care Med. 1997;25:46–51.
James JH, Luchette FA, McCarter FD, Fischer JE. Lactate is an unreliable indicator of tissue hypoxia in injury or sepsis. Lancet. 1999;354:505–8.
Holm J, Håkanson E, Vánky F, Svedjeholm R. Mixed venous oxygen saturation predicts short- and long-term outcome after coronary artery bypass grafting surgery: a retrospective cohort analysis. Br J Anaesth. 2011;107:344–50.
Carl M, Alms A, Braun J, Dongas A, Erb J, Goetz A, et al. S3 Guidelines for intensive care in cardiac surgery patients: hemodynamic monitoring and cardiocirculary system. Ger Med Sci. 2010;8:Doc12.
Habicher M, von Heymann C, Spies CD, Wernecke K-D, Sander M. Central venous-arterial pCO2 difference identifies microcirculatory hypoperfusion in cardiac surgical patients with normal central venous oxygen saturation: a retrospective analysis. J Cardiothorac Vasc Anesth. 2015;29(3):646–55.
Futier E, Robin E, Jabaudon M, Guerin R, Petit A, Bazin J-E, et al. Central venous O2 saturation and venous-to-arterial CO2 difference as complementary tools for goal-directed therapy during high-risk surgery. Crit Care Lond Engl. 2010;14:R193.
Robin E, Futier E, Pires O, Fleyfel M, Tavernier B, Lebuffe G, et al. Central venous-to-arterial carbon dioxide difference as a prognostic tool in high-risk surgical patients. Crit Care Lond Engl. 2015;19:227.
Vallet B, Teboul JL, Cain S, Curtis S. Venoarterial CO(2) difference during regional ischemic or hypoxic hypoxia. J Appl Physiol Bethesda Md. 1985;2000(89):1317–21.
Morel J, Grand N, Axiotis G, Bouchet JB, Faure M, Auboyer C, et al. High veno-arterial carbon dioxide gradient is not predictive of worst outcome after an elective cardiac surgery: a retrospective cohort study. J Clin Monit Comput. 2016;30:783–9.
Pölönen P, Ruokonen E, Hippeläinen M, Pöyhönen M, Takala J. A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg. 2000;90:1052–9.
De Backer D. Detailing the cardiovascular profile in shock patients. Crit Care Lond Engl. 2017;21:311.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the european society of intensive care medicine. Intensive Care Med. 1996;22:707–10.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute kidney injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care Lond Engl. 2007;11:R31.
Cuschieri J, Rivers EP, Donnino MW, Katilius M, Jacobsen G, Nguyen HB, et al. Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med. 2005;31:818–22.
Ruokonen E, Soini HO, Parviainen I, Kosonen P, Takala J. Venoarterial CO2 gradient after cardiac surgery: relation to systemic and regional perfusion and oxygen transport. Shock Augusta Ga. 1997;8:335–40.
Balzer F, Sander M, Simon M, Spies C, Habicher M, Treskatsch S, et al. High central venous saturation after cardiac surgery is associated with increased organ failure and long-term mortality: an observational cross-sectional study. Crit Care Lond Engl. 2015;19:168.
Perz S, Uhlig T, Kohl M, Bredle DL, Reinhart K, Bauer M, et al. Low and “supranormal” central venous oxygen saturation and markers of tissue hypoxia in cardiac surgery patients: a prospective observational study. Intensive Care Med. 2011;37:52–9.
Vallée F, Vallet B, Mathe O, Parraguette J, Mari A, Silva S, et al. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intensive Care Med. 2008;34:2218–25.
Ospina-Tascón GA, Umaña M, Bermúdez W, Bautista-Rincón DF, Hernandez G, Bruhn A, et al. Combination of arterial lactate levels and venous-arterial CO2 to arterial-venous O2 content difference ratio as markers of resuscitation in patients with septic shock. Intensive Care Med. 2015;41:796–805.
van Beest PA, van Ingen J, Boerma EC, Holman ND, Groen H, Koopmans M, et al. No agreement of mixed venous and central venous saturation in sepsis, independent of sepsis origin. Crit Care Lond Engl. 2010;14:R219.
Acknowledgements
The proofreading of this article was supported by the Bibliothèque Scientifique de l’Internat de Lyon and the Hospices Civils de Lyon.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
According to the French law and because data were collected during routine care, authorization was granted to waive written informed consent. However, verbal consent was obtained from all study participants before surgery.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Portran, P., Jacquet-Lagreze, M., Schweizer, R. et al. Improving the prognostic value of ∆PCO2 following cardiac surgery: a prospective pilot study. J Clin Monit Comput 34, 515–523 (2020). https://doi.org/10.1007/s10877-019-00352-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00352-6