Abstract
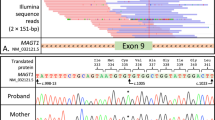
XMEN disease (X-linked immunodeficiency with Magnesium defect, Epstein-Barr virus infection and Neoplasia) is a novel primary immune deficiency caused by mutations in MAGT1 and characterised by chronic infection with Epstein-Barr virus (EBV), EBV-driven lymphoma, CD4 T-cell lymphopenia, and dysgammaglobulinemia [1]. Functional studies have demonstrated roles for magnesium as a second messenger in T-cell receptor signalling [1], and for NKG2D expression and consequently NK- and CD8 T-cell cytotoxicity [2]. 7 patients have been described in the literature; the oldest died at 45 years and was diagnosed posthumously [1–3]. We present the case of a 58-year-old Caucasian gentleman with a novel mutation in MAGT1 with the aim of adding to the phenotype of this newly described disease by detailing his clinical course over more than 20 years.



Similar content being viewed by others
References
Li FY, Chaigne-Delalande B, Kanellopoulou C, Davis JC, Matthews HF, Douek DC, et al. Second messenger role for Mg2+ revealed by human T-cell immunodeficiency. Nature. 2011;475(7357):471–6.
Chaigne-Delalande B, Li FY, O’Connor GM, Lukacs MJ, Jiang P, Zheng L, et al. Mg2+ regulates cytotoxic functions of NK and CD8 T cells in chronic EBV infection through NKG2D. Science. 2013;341(6142):186–91.
Li FY, Chaigne-Delalande B, Su H, Uzel G, Matthews H, Lenardo MJ. XMEN disease: a new primary immunodeficiency affecting Mg2+ regulation of immunity against Epstein-Barr virus. Blood. 2014;123(14):1248–52.
Sadler R, Bateman EA, Heath V, Patel SY, Schwingshackl PP, Cullinane AC, et al. Establishment of a healthy human range for the whole blood ’OX40′ assay for the detection of antigen-specific CD4+ T cells by flow cytometry. Cytometry B Clin Cytom. 2014.
Misbah SA, Spickett GP, Zeman A, Esiri MM, Wallington TB, Kurtz JB, et al. Progressive multifocal leucoencephalopathy, sclerosing cholangitis, bronchiectasis and disseminated warts in a patient with primary combined immune deficiency. J Clin Pathol. 1992;45(7):624–7.
Chikezie PU, Greenberg AL. Idiopathic CD4+ T lymphocytopenia presenting as progressive multifocal leukoencephalopathy: case report. Clin Infect Dis. 1997;24(3):526–7.
Haider S, Nafziger D, Gutierrez JA, Brar I, Mateo N, Fogle J. Progressive multifocal leukoencephalopathy and idiopathic CD4 + lymphocytopenia: a case report and review of reported cases. Clin Infect Dis. 2000;31(4):E20–2.
Inhoff O, Doerries K, Doerries R, Scharf J, Groden C, Goerdt S, et al. Disseminated cutaneous Kaposi sarcoma and progressive multifocal leukoencephalopathy in a patient with idiopathic CD4+ T lymphocytopenia. Arch Dermatol. 2007;143(5):673–5.
Delgado-Alvarado M, Sedano MJ, González-Quintanilla V, de Lucas EM, Polo JM, Berciano J. Progressive multifocal leukoencephalopathy and idiopathic CD4 lymphocytopenia. J Neurol Sci. 2013;327(1–2):75–9.
Carson KR, Focosi D, Major EO, Petrini M, Richey EA, West DP, et al. Monoclonal antibody-associated progressive multifocal leucoencephalopathy in patients treated with rituximab, natalizumab, and efalizumab: a review from the research on adverse drug events and reports (RADAR) project. Lancet Oncol. 2009;10(8):816–24.
Ferenczy MW, Marshall LJ, Nelson CD, Atwood WJ, Nath A, Khalili K, et al. Molecular biology, epidemiology, and pathogenesis of progressive multifocal leukoencephalopathy, the JC virus-induced demyelinating disease of the human brain. Clin Microbiol Rev. 2012;25(3):471–506.
Houff SA, Major EO, Katz DA, Kufta CV, Sever JL, Pittaluga S, et al. Involvement of JC virus-infected mononuclear cells from the bone marrow and spleen in the pathogenesis of progressive multifocal leukoencephalopathy. N Engl J Med. 1988;318(5):301–5.
Monaco MC, Atwood WJ, Gravell M, Tornatore CS, Major EO. JC virus infection of hematopoietic progenitor cells, primary B lymphocytes, and tonsillar stromal cells: implications for viral latency. J Virol. 1996;70(10):7004–12.
Houff SA, Berger JR. The bone marrow, B cells, and JC virus. J Neurovirol. 2008;14(5):341–3.
Acknowledgments
This work was supported by the intramural research program of the National Institute of Allergy and Infectious Diseases. We thank Tammy Krogmann for preparing RNA and cDNA from the nephew.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jeffrey I. Cohen and Smita Y. Patel contributed equally
Work originated from the Department of Clinical Immunology and the Nuffield Department of Medicine, John Radcliffe Hospital, Oxford.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 195 kb)
Rights and permissions
About this article
Cite this article
Dhalla, F., Murray, S., Sadler, R. et al. Identification of a Novel Mutation in MAGT1 and Progressive Multifocal Leucoencephalopathy in a 58-Year-Old Man with XMEN Disease. J Clin Immunol 35, 112–118 (2015). https://doi.org/10.1007/s10875-014-0116-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-014-0116-2