Abstract
Purpose
To evaluate whether ICSI offers any benefit compared with IVF in different ovarian response categories in case of non-male factor infertility.
Methods
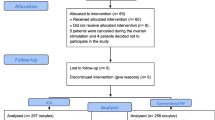
This is a retrospective multicenter analysis using individual patient data, conducted in 15 tertiary referral hospitals in Europe (1 center in Belgium and 14 in Spain). The study included the first cycle of all patients undergoing ovarian stimulation for IVF or ICSI in a GnRH antagonist protocol. Only patients having either IVF or ICSI for non-male factor infertility were included. Patients were divided into 4 groups based on their ovarian response as follows: group A, poor responders (1–3 oocytes); group B, suboptimal responders (4–9 oocytes); group C, normal responders (10–15 oocytes); group D, high responders (> 15 oocytes).
Results
In total, 4891 patients were analyzed, of whom 4227 underwent ICSI and 664 IVF. There was no significant difference for the insemination method (ICSI vs. IVF) used among the different ovarian response categories: 87% vs. 13%, 87% vs. 13%, 86% vs. 14%, 84% vs. 16%, for groups A, B, C, and D, respectively, p value = 0.35. Mean fertilization rates and embryo utilization rates were comparable between IVF and ICSI in the whole cohort. Fresh and cumulative LBR did not differ significantly for IVF and ICSI in poor, suboptimal, normal, and high responders.
Conclusion
There is no advantage of ICSI over IVF as insemination method for non-male factor infertility, irrespective of the ovarian response. The number of oocytes retrieved has no value for the selection of the insemination procedure in case of non-male infertility.




Similar content being viewed by others
Change history
14 October 2019
The original article unfortunately contained 2 mistakes.
References
Palermo G, Joris H, Devroey P, Van Steirteghem AC. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet. 1992;340(8810):17–8.
De Geyter C, Calhaz-Jorge C, Kupka MS, Wyns C, Mocanu E, Motrenko T, et al. ART in Europe, 2014: results generated from European registries by ESHRE: the European IVF-monitoring consortium (EIM) for the European Society of Human Reproduction and Embryology (ESHRE). Hum Reprod. 2018;33(9):1586–601. https://doi.org/10.1093/humrep/dey242.
Boulet SL, Mehta A, Kissin DM, Warner L, Kawwass JF, Jamieson DJ. Trends in use of and reproductive outcomes associated with intracytoplasmic sperm injection. JAMA. 2015;313(3):255–63. https://doi.org/10.1001/jama.2014.17985.
Adamson GD, de Mouzon J, Chambers GM, Zegers-Hochschild F, Mansour R, Ishihara O, et al. International Committee for Monitoring Assisted Reproductive Technology: world report on assisted reproductive technology, 2011. Fertil Steril. 2018;110(6):1067–80. https://doi.org/10.1016/j.fertnstert.2018.06.039.
Check JH, Yuan W, Garberi-Levito MC, Swenson K, McMonagle K. Effect of method of oocyte fertilization on fertilization, pregnancy and implantation rates in women with unexplained infertility. Clin Exp Obstet Gynecol. 2011;38(3):203–5.
Luna M, Bigelow C, Duke M, Ruman J, Sandler B, Grunfeld L, et al. Should ICSI be recommended routinely in patients with four or fewer oocytes retrieved? J Assist Reprod Genet. 2011;28(10):911–5. https://doi.org/10.1007/s10815-011-9614-9.
Tannus S, Son WY, Gilman A, Younes G, Shavit T, Dahan MH. The role of intracytoplasmic sperm injection in non-male factor infertility in advanced maternal age. Hum Reprod. 2017;32(1):119–24. https://doi.org/10.1093/humrep/dew298.
Schwarze J, Jeria R, Crosby J, Villa S, Ortega O, Pommer R. Is there a reason to perform ICSI in the absence of male factor? Lessons from the Latin American Registry of ART. Human Reprod Open. 2017;2(2):1–5. https://doi.org/10.1093/hropen/hox013.
Drakopoulos P, Blockeel C, Stoop D, Camus M, de Vos M, Tournaye H, et al. Conventional ovarian stimulation and single embryo transfer for IVF/ICSI. How many oocytes do we need to maximize cumulative live birth rates after utilization of all fresh and frozen embryos? Hum Reprod. 2016;31(2):370–6. https://doi.org/10.1093/humrep/dev316.
Polyzos NP, Drakopoulos P, Parra J, Pellicer A, Santos-Ribeiro S, Tournaye H, et al. Cumulative live birth rates according to the number of oocytes retrieved after the first ovarian stimulation for in vitro fertilization/intracytoplasmic sperm injection: a multicenter multinational analysis including approximately 15,000 women. Fertil Steril. 2018;110(4):661–70 e1. https://doi.org/10.1016/j.fertnstert.2018.04.039.
Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010;16(3):231–45. https://doi.org/10.1093/humupd/dmp048.
Papanikolaou EG, Pozzobon C, Kolibianakis EM, Camus M, Tournaye H, Fatemi HM, et al. Incidence and prediction of ovarian hyperstimulation syndrome in women undergoing gonadotropin-releasing hormone antagonist in vitro fertilization cycles. Fertil Steril. 2006;85(1):112–20. https://doi.org/10.1016/j.fertnstert.2005.07.1292.
Humaidan P, Polyzos NP, Alsbjerg B, Erb K, Mikkelsen AL, Elbaek HO, et al. GnRHa trigger and individualized luteal phase hCG support according to ovarian response to stimulation: two prospective randomized controlled multi-centre studies in IVF patients. Hum Reprod. 2013;28(9):2511–21. https://doi.org/10.1093/humrep/det249.
Ferraretti AP, La Marca A, Fauser BC, Tarlatzis B, Nargund G, Gianaroli L, et al. ESHRE consensus on the definition of ‘poor response’ to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26(7):1616–24. https://doi.org/10.1093/humrep/der092.
Polyzos NP, Sunkara SK. Sub-optimal responders following controlled ovarian stimulation: an overlooked group? Hum Reprod. 2015;30(9):2005–8. https://doi.org/10.1093/humrep/dev149.
Embryology ESIGo, Alpha Scientists in Reproductive Medicine. Electronic address cbgi. The Vienna consensus: report of an expert meeting on the development of ART laboratory performance indicators. Reprod BioMed Online. 2017;35(5):494–510. https://doi.org/10.1016/j.rbmo.2017.06.015.
Dang VQ, Vuong LN, Ho TM, Ha AN, Nguyen QN, Truong BT, et al. The effectiveness of ICSI versus conventional IVF in couples with non-male factor infertility: study protocol for a randomised controlled trial. Hum Reprod Open. 2019;2019(2):hoz006. https://doi.org/10.1093/hropen/hoz006.
Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The international glossary on infertility and fertility care, 2017. Hum Reprod. 2017;32(9):1786–801. https://doi.org/10.1093/humrep/dex234.
van Rumste MM, Evers JL, Farquhar CM. Intra-cytoplasmic sperm injection versus conventional techniques for oocyte insemination during in vitro fertilisation in patients with non-male subfertility. Cochrane Database Syst Rev. 2003;2:CD001301. https://doi.org/10.1002/14651858.CD001301.
Rosen MP, Shen S, Dobson AT, Fujimoto VY, McCulloch CE, Cedars MI. Oocyte degeneration after intracytoplasmic sperm injection: a multivariate analysis to assess its importance as a laboratory or clinical marker. Fertil Steril. 2006;85(6):1736–43. https://doi.org/10.1016/j.fertnstert.2005.12.017.
Li Z, Wang AY, Bowman M, Hammarberg K, Farquhar C, Johnson L, et al. ICSI does not increase the cumulative live birth rate in non-male factor infertility. Hum Reprod. 2018;33(7):1322–30. https://doi.org/10.1093/humrep/dey118.
Acknowledgments
The authors would like to thank Walter Meul and Alfredo Navarro for their contribution to the data management of the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 53 kb)
Rights and permissions
About this article
Cite this article
Drakopoulos, P., Garcia-Velasco, J., Bosch, E. et al. ICSI does not offer any benefit over conventional IVF across different ovarian response categories in non-male factor infertility: a European multicenter analysis. J Assist Reprod Genet 36, 2067–2076 (2019). https://doi.org/10.1007/s10815-019-01563-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-019-01563-1