Abstract
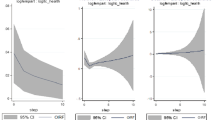
This paper examines health care expenditure (HCE) disparities between the European Union countries over the period 1995–2010. By means of using a continuous version of the distribution dynamics approach, the key conclusions are that the reduction in disparities is very weak and, therefore, persistence is the main characteristic of the HCE distribution. In view of these findings, a preliminary attempt is made to add some insights into potentially main factors behind the HCE distribution. The results indicate that whereas per capita income is by far the main determinant, the dependency ratio and female labour participation do not play any role in explaining the HCE distribution; as for the rest of the factors studied (life expectancy, infant mortality, R&D expenditure and public HCE expenditure share), we find that their role falls somewhat in between.









Similar content being viewed by others
Notes
In the same line, the empirical literature on the determinants of HCE, pioneered by Newhouse (1977), mainly considers four groups of determinants: income, demographic, heterogeneity of health care systems, and technological progress related variables.
Although in a different context, Meijer et al. (2013) also stress the fact that, with reference to health care expenditure, we need not only to account for its growth “but also explain changes in its distribution” (p. 88).
Quantile regressions, sometimes used to study convergence/divergence, are somewhat better suited than conventional regresssion methods to use the information for the whole distribution. However, they do it to a much lesser extent than the distribution dynamics approach.
Although we are well aware that OECD Health Data is the largest available source of statistics to compare OECD health care systems, here we have opted for the National Health Accounts database of the WHO because the OECD database does not provide information for some EU countries (Bulgaria, Cyprus, Latvia, Lithuania, Malta and Romania).
The PPPs are given in national currency units (NCU) per US dollar.
Another important and recent paper on this issue, devoted to Indian States, is Apergis and Padhi (2013). Other papers have also studied the issue of convergence/divergence across regions/states of a country but from the point of view of health outcomes. Montero-Granados and Dios Jimenez (2007), for the Spanish case, and Gächter and Theurl (2011), for the Austrian one, are among the most relevant.
As stressed by Hartwig (2008), “the share of current health expenditure (HCE) in the gross domestic product (GDP) rises rapidly in virtually all developed nations” (p. 603).
The bandwidth election gives a trade-off between bias and variance. Small bandwidths produce small bias and large variance, while large bandwidths yield large bias and small variance.
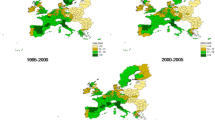
The “plateau” between around 30 and 130 % of the average is “taller” in 2010 than in the other selected years.
We refer the reader to Maza et al. (2010) for technical details regarding the main differences between the traditional and Hyndman continuous approaches.
These authors proposed a three-steps strategy for bandwidth selection: first, bandwidth selection with the traditional rule suggested by Silverman (1986); second, a bootstrap bandwidth selection approach for estimating conditional distribution functions (Hall et al. 1999); third, a regression-based bandwidth selector (Fan et al. 1996).
Then, we have 16 years \(\times \) 27 countries = 432 observations.
Although Wilson (1999) has argued for the need to count with “a formal theory to explain or predict the per capita medical care expenditure of a nation” (p. 160) and Hartwig (2008) has intended to meet this demand by revisiting Baumol’s model of unbalanced growth, it happens that, as stated by Hoffmeyer and McCarthy (1994) “there is just one, very clear, very well-established statistical fact relating to health expenditure care: its correlation with GDP. No other robust and stable correlation has yet been found” (p. 67).
However, it is necessary to stress that there is no consensus on this point in health economics literature. As rightly pointed out by an anonymous referee, there are doubts about whether a link exists, the signs of the coefficients, and even the direction the link runs.
We use total R&D data because there are no homogeneous data on health R&D spending for all the countries included in our sample.
References
Apergis, N., & Padhi, P. (2013). Health expenses and economic growth: Convergence dynamics across the Indian States. International Journal of Health Care Finance and Economics, 13(3–4), 261–277.
Barros, P. P. (1998). The black box of health care expenditure growth determinants. Health Economics, 7(6), 533–544.
Bashtannyk, D., & Hyndman, R. (2001). Bandwidth selection for kernel conditional estimation. Computational Statistics and Data Analysis, 36, 279–298.
Breyer, F., Costa-Font, J., & Felder, S. (2010). Ageing, health and health care. Oxford Review of Economic Policy, 26(4), 674–690.
Clark, R. (2011). World health inequality: Convergence, divergence, and development. Social Science and Medicine, 72, 617–624.
De Meijer, C., O’Donnell, O., Koopmanschap, M., & Van Doorslaer, E. (2013). Health expenditure growth: Looking beyond the average through the composition of the full distribution. Journal of Health Economics, 32, 88–105.
Dormont, B., Martins, J.O., Pelgrin, F. & Suhcke, M. (2007). Health expenditure, longevity and growth. Paper presented in the IX European Conference of the Fondazione Rodolfo Debenedetti on “Health, Longevity and Productivity”.
Dreger, C. & Reimers, H.E. (2005). Health care expenditures in OECD countries: A panel unit root and cointegration analysis. IZA DP \(\text{ N }^{\rm o}\) 1469.
Durlauf, S. N., & Quah, D. (1999). The new empirics for economic growth. In J. Taylor & M. Woodford (Eds.), Handbook of macroeconomics (Vol. I, pp. 235–308). Amsterdam: North-Holland.
Fan, J., Yao, Q., & Tong, H. (1996). Estimation of conditional densities and sensitivity measures in nonlinear dynamical systems. Biometrika, 83(1), 189–206.
Farag, M., NandaKumar, A., Wallackm, S., Hodgkin, D., Gaumer, G., & Erbil, C. (2012). The income elasticity of health care spending in developing and developed countries. International Journal of Health Care Finance and Economics, 12(2), 145–162.
Fischer, M. M., & Stumpner, P. (2008). Income distribution dynamics and cross-region convergence in Europe. Spatial filtering and novel stochastic kernel representations. Journal of Geographical Systems, 10(2), 109–140.
Gächter, M., & Theurl, E. (2011). Health status convergence at the local level: Empirical evidence from Austria. International Journal for Equity in Health, 10, 34.
Getzen, T. E. (2000). Health care is an individual necessity and a national luxury: Applying multilevel decision models to the analysis of health care expenditure. Journal of Health Economics, 19, 259–270.
Goli, S., & Arokiasamy, P. (2013). Trends in health and health inequalities among major states of India: Assessing progress through convergence models. Health Economics, Policy and Law, doi:10.1017/S1744133113000042.
Hall, P., Wolff, R. C., & Yao, Q. (1999). Methods for estimating a conditional density distribution. Journal of the American Statistical Association, 94(455), 154–163.
Hartwig, J. (2008). What drives health care expenditure?—Baumol’s model of “unbalanced growth” revisited. Journal of Health Economics, 27, 603–623.
Hitiris, T. (1997). Health care expenditure and integration in ten countries of the European Union. Applied Economics, 29, 1–6.
Hitiris, T., & Nixon, J. (2001). Convergence on health care expenditure in the EU countries. Applied Economics Letters, 8, 223–228.
Hoffmeyer, U. K., & McCarthy, T. R. (Eds.). (1994). Financing health care (Vol. 1). Dordrecht: Kluwer Academic Publishers.
Hyndman, R. J., Bashtannyk, D. M., & Grunwald, G. K. (1996). Estimating and visualizing conditional densities. Journal of Computational and Graphical Statistics, 5(4), 315–336.
Islam, N. (2003). What have we learnt from the convergence debate? Journal of Economic Surveys, 17, 309–362.
Kerem, K., Püss, T., Viies, M., & Maldre, R. (2008). Health and convergence of health care expenditure in EU. International Business and Economics Research Journal, 7, 29–44.
Laurini, M. P., & Valls, P. L. (2009). Conditional stochastic kernel estimation by nonparametric methods. Economics Letters, 105(3), 234–238.
Leiter, A. M., & Theurl, E. (2012). The convergence of health care financing structures: empirical evidence from OECD-countries. European Journal of Health Economics, 13, 7–18.
Maza, A., Hierro, M., & Villaverde, J. (2010). Measuring intra-distribution dynamics: An application of different approaches to the European regions. Annals of Regional Science, 45(2), 313–329.
Maza, A., Villaverde, J., & Hierro, M. (2009). Regional productivity distribution in the EU: Which are the influencing factors? European Planning Studies, 17(1), 149–159.
Montero-Granados, R., & De Dios Jimenez, J. (2007). Decentralisation and convergence in health among provinces of Spain. Social Science and Medicine, 64, 1253–1264.
Narayan, P. K. (2007). Do health expenditures ‘catch-up’? Evidence from OECD countries. Health Economics, 16, 993–1008.
Newhouse, J. P. (1977). Medical-care expenditure: A cross-national survey. The Journal of Human Resources, 12(1), 115–125.
Nixon, J. (2000). Convergence of health care spending and health outcomes in the European Union, 1960–95. Centre for Health Economics, Discussion Paper : The University of York. 183.
Okunade, A. (2005). Analysis and implications of the determinants of heathcare management expenditure in African countries. Health Care Management Science, 8, 267–276.
Okunade, A., & Murthy, V. (2002). Technology as a ’major driver’of health care costs: A cointegration analysis of the Newhouse conjecture. Journal of Health Economics, 21, 147–159.
Okunade, A., Karakus, M., & Okeke, C. (2004). Determinants of health expenditure growth of the OECD countries: Jackknife resamplin plan estimates. Health Care Managament Science, 7, 173–183.
Pammolli, F., Riccaboni, M., & Magazzini, L. (2012). The sustainability of European health care systems: Beyond income and aging. European Journal of Health Economics, 13, 623–634.
Panopolou, E., & Pantelidis, T. (2012). Convergence in per capita health expenditures and health outcomes in the OECD countries. Applied Economics, 44(30), 3909–3920.
Quah, D. (1996a). Twin peaks: Growth and convergence in models of distribution dynamics. Economic Journal, 106, 1045–1055.
Quah, D. (1996b). Empirics for economic growth and convergence. European Economic Review, 40, 1353–1375.
Quah, D. (1997). Empirics for growth and distribution: Stratification, polarization, and convergence clubs. Journal of Economic Growth, 2, 27–59.
Silverman, B. W. (1986). Density estimation for statistics and data analysis. London: Chapman and Hall.
Spitzer, A., Camus, D., Desaulles, C., & Kuhne, N. (2006). The changing context of Western European healthcare systems: Convergence versus divergence in nursing problematics. Social Sciences and Medicine, 63, 1796–1810.
Villaverde, J., & Maza, A. (2011). Measurement of regional economic convergence. In P. de Lombaerde, R. Flores, R. Lapadre, & M. Schulz (Eds.), The regional integration manual. Quantitative and qualitative methods (pp. 147–178). London: Routledge.
Wang, Z. (2009). The convergence of health care expenditure in the United States. Health Economics, 18, 55–70.
Wilson, R. M. (1999). Medical care expenditures and GDP growth in OECD nations. American Association of Behavioral and Social Sciences Journal, 2, 159–171.
Xu, K., Saksena, P. & Holly, A. (2011). The determinants of health expenditure. A country-level panel data analysis. WHO Working Paper, December.
Acknowledgments
We gratefully acknowledge an anonymous referee and the Editor (P. P. Barros) for comments and suggestions on an earlier version of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Villaverde, J., Maza, A. & Hierro, M. Health care expenditure disparities in the European Union and underlying factors: a distribution dynamics approach. Int J Health Care Finance Econ 14, 251–268 (2014). https://doi.org/10.1007/s10754-014-9147-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-014-9147-8