Summary
Background Foretinib is a small-molecule, oral multikinase inhibitor primarily targeting the mesenchymal epithelial transition (MET) factor receptor, and the vascular endothelial growth factor receptor 2. We conducted a phase II study to evaluate the single-agent activity and tolerability of foretinib in patients with recurrent/metastatic squamous cell carcinoma of the head and neck (SCCHN). Methods An open-label, single-arm, multicenter trial employing a Simon 2-stage design was conducted with a total of 41 patients planned for the study. One or more responses in the first 14 patients were required in order to progress to the second stage. Foretinib was administered as 240 mg orally for 5 consecutive days of a 14-day treatment cycle (5/9 schedule) to patients with recurrent and/or metastatic SCCHN. Results Fourteen patients were enrolled. The study did not meet criteria for continuing to the second stage. A maximum of 30 cycles were administered (median = 4.0). Fifty percent of patients (7/14) showed stable disease (SD), 43 % of patients (6/14) experienced tumor shrinkage and two patients had prolonged disease stabilization for ≥13 months. The most common adverse events were fatigue, constipation and hypertension, which were manageable with additional medication or adjustments to the dosing schedule. Conclusion Foretinib 240 mg on a 5/9 schedule was generally well tolerated. SD was the best-observed outcome, with minor tumor shrinkage detected in nearly half of all patients. The efficacy results, prolonged disease stabilization and tolerable side-effect profile, support further investigation, possibly in combination with other targeted agents or cytotoxic chemotherapy for SCCHN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck cancer (HNC) represents a heterogeneous group of potentially deadly cancers. Approximately 650,000 HNC diagnoses are made each year worldwide with almost 50,000 cases and 11,000 deaths occurring in the United States alone [1, 2]. Overall 5-year survival rates for patients with HNC are below 50 % [3]. Although the head and neck comprise a variety of tissue types, squamous cell carcinomas originating from mucosal surfaces represent >90 % of all cases of HNC [3]. The risk factors for squamous cell carcinomas of the head and neck (SCCHN) have been strongly linked with tobacco and alcohol use as well as with human papillomavirus [3].
Treatment modalities for SCCHN include surgery, radiation therapy, and chemotherapy [4]. Most patients with SCCHN present with advanced locoregional disease [5]. With advanced SCCHN, only 35 % to 55 % of patients survive and remain disease-free for 3 years, despite aggressive therapy [1]. Locoregional recurrence develops in 30 % to 40 % of patients and distant metastases develop in 12 % to 22 % of patients [6]. Once the disease is recurrent/metastatic, combination chemotherapy using a platinum-based regimen remains the standard of care for SCCHN. The addition of cetuximab, an epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor, to chemotherapeutic agents has provided a modest survival benefit (10 vs. 7 months) [7]. Nevertheless, palliative treatment of recurrent/metastatic SCCHN remains largely ineffective and little progress has been made. More effective, targeted treatments are needed.
The mesenchymal epithelial transition (MET) factor receptor and its sole ligand, hepatocyte growth factor (HGF), are strongly overexpressed in >80 % of SCCHN [8, 9]. Activation of the MET factor receptor by HGF stimulates cell proliferation, survival and motility, thus promoting cancer cell metastases [9, 10]. There is evidence to suggest that the HGF/MET signaling pathway may represent a promising target in the treatment of recurrent SCCHN, as preclinical data have provided additional support for activity with MET inhibitors in SCCHN models [8, 9, 11]. Vascular endothelial growth factor (VEGF) is also upregulated in patients with SCCHN [12]. VEGF upregulation in SCCHN has been linked to tumor angiogenesis and disease severity [13, 14]. However, targeting VEGF receptors alone in recurrent or metastatic cancers of the head and neck has shown modest objective response rates; data from one study showed only one minor response and one partial response out of 31 evaluable patients [15]. HGF and VEGF may, therefore, act in concert to spur angiogenesis and metastasis in patients with SCCHN. Thus, targeting both the HGF/MET and VEFG signaling pathways is an attractive therapeutic approach [16]. Previous studies combining anti-angiogenic agents with other approaches have shown promise with combination approaches using anti-angiogenic agents, such as the combination of erlotinib, an EGFR tyrosine kinase inhibitor, and bevacizumab [17]. Other targeted therapies used as single agents have shown limited or no activity for SCCHN [18].
Foretinib (also known as GSK1363089 or XL880) is an oral multikinase inhibitor that primarily targets signaling of HGF/MET (in vitro IC50 of 3 nmol/L) and the VEGF receptor-2 (VEGFR2) (in vitro IC50 of 7 nmol/L) [19] signaling pathways by binding in the adenosine triphosphate pocket of both MET and VEGFR2. In preclinical studies, foretinib induced tumor hemorrhage and necrosis in human xenografts [20]. Foretinib also targets several other receptor tyrosine kinases (RTKs), including the MET-related recepteur d'origine nantais (RON) receptor (in vitro IC50 of 3 nmol/L) [19] and additional RTKs involved in tumor angiogenesis (AXL and TIE-2) [20, 21]. While the role of RON in SCCHN remains unclear, its effects appear to largely overlap with MET, and in other tumor types synergy has been reported with the inhibition of both targets [22]. MET has been evaluated extensively as a potential treatment target for SCCHN, with promising results [8, 9], and foretinib demonstrated activity against human SCCHN cell lines [23]. Foretinib has also shown antitumor activity in clinical studies of papillary renal cell carcinoma and hepatocellular carcinoma [24, 25], and may have the potential to prevent tumor growth in SCCHN, chiefly by reducing tumor cell proliferation and metastasis through HGF/MET inhibition and decreasing angiogenesis through VEGFR2 pathway inhibition.
The primary purpose of this study was to evaluate the response rate for single-agent foretinib treatment in patients with recurrent and/or metastatic SCCHN, and to assess foretinib safety and tolerability in SCCHN patients. This is the first report evaluating a MET inhibitor in SCCHN.
Patients and methods
Eligible patients were ≥18 years of age with histologically or cytologically confirmed recurrent and/or metastatic SCCHN who were not eligible for curative-intent surgery or radiotherapy. Patients had measurable disease according to Response Evaluation Criteria In Solid Tumors (RECIST) 1.0, Eastern Cooperative Oncology Group (ECOG) performance status of ≤1 [26]. All patients participating in the study provided informed consent.
Exclusion criteria included previous radiation therapy (>25 % of bone marrow) within 30 days of study treatment, >1 regimen of systemic anticancer therapy for disease that had recurred or was metastatic, except for adjuvant or neoadjuvant chemotherapy, those who had disease progression within 6 months after completion of curative-intent therapy, and patients at high risk of bleeding.
Study design
This was a single-arm, phase II, multicenter (all in the United States), non-randomized, open-label, Simon 2-stage safety and efficacy study [27]. The primary objectives of this study were to determine the response rate according to RECIST 1.0 [28] for foretinib treatment in patients with SCCHN, and to evaluate the safety and tolerability of foretinib. Secondary objectives included an assessment of progression-free survival (PFS), duration of response, overall survival (OS) and the pharmacokinetic parameters of foretinib. Foretinib was administered at doses of 240 mg orally for 5 consecutive days of a 14-day treatment cycle (5/9 schedule). Patients fasted from 2 h prior to 1 h after each dose. In the absence of progressive disease and unacceptable toxicity, patients were eligible to continue with foretinib treatment for 1 year or longer. If the patient required additional anticancer therapy (e.g. chemotherapy, radiation or surgery), foretinib dosing was discontinued. The relationship between foretinib trough concentrations and percent change from baseline in tumor size was examined.
Assessments
Tumor assessments were performed within 14 days before dosing. During the study treatment period tumor response was assessed after 8 weeks. Patients were asked to return to the study site 30 days after the last dose of foretinib for laboratory assessments and clinical examination. Patients were contacted for follow-up at 90 and 180 days after the last dose. Toxicity grade of adverse events (AEs), serious AEs and laboratory variables were defined by the National Cancer Institute Common Terminology Criteria for Adverse Events v3.0.
Statistical analyses
A total of 14 patients were enrolled into stage 1 (to ensure a total of 12 evaluable patients). If no patients had either a complete response (CR) or partial response (PR) to treatment in stage 1, then the study was to be halted. If one or more patients had a response in stage 1, a second stage was to be opened to enroll additional patients up to a total of 41 patients (to ensure a total of 35 evaluable patients). EGFR inhibitors have a response rate of 5 % to 13 % as single agents, and a similar response rate was hypothesized to be meaningful in the current study [7, 29]. The study had a type 1 error rate of 5 % for the null hypothesis that the response rate is at least 10 %, with 80 % power for an alternative response rate of at least 25 %.
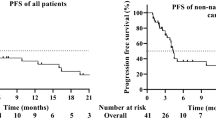
Response rates were summarized with exact 95 % confidence intervals using Klopper–Pearson methods, and PFS, stable disease (SD) and OS data were summarized using Kaplan–Meier methods with 95 % confidence intervals for medians. Foretinib exposure measures for all analyses were the average trough concentration for foretinib across days 5, 19, 33 and 47, which represented the trough concentration after 4 days of dosing. Ordinal logistic regression was used to examine the maximal grade of the following AEs: elevated aspartate aminotransferase (AST), elevated alanine aminotransferase (ALT), elevated lactate dehydrogenase, fatigue and hypertension. Linear regression analysis was used to determine whether a relationship existed between exposure and change in tumor size.
Results
Patient disposition
Between August 2007 and May 2009, 14 patients were enrolled. Of these, only 11 treated patients had at least one on-treatment scan. Recruitment was halted because no patient met the treatment response criterion (CR or PR) required for continuation to stage 2. All patients had histologically or cytologically confirmed SCCHN, with a mean time since the initial diagnosis of 1.4 years (range, 0–7 years). All patients had distant metastatic disease, and 12 patients had received prior antitumor therapy regimens and radiation therapy (85.7 %). Two patients did not have any line of prior therapy for recurrent and/or metastatic disease, four patients had received only first-line therapy, six patients two lines of prior therapy, and two patients three lines of prior therapy. Chemotherapeutic drugs included platinating agents, taxanes, 5-FU, hydroxycarbamide, cetuximab and bevacizumab. Table 1 presents the baseline demographics and Table 2 displays the disposition of the 14 patients included in the study.
Efficacy
Although there were no confirmed PRs or CRs in this trial, seven of 14 patients had SD and six of 14 patients experienced some tumor shrinkage (range 5–21 %) (Fig. 1). The median duration of SD was 4.1 months and the disease stabilization rate was 50 % (Table 3). Two patients had prolonged SD of 13 and 13.9 months’ duration, respectively.
Waterfall plot for best percentage change from baseline in target lesion tumor measurement. Only 11 of the 14 treated patients had at least one on-treatment scan to be included. *Patient had a best percentage change from baseline in tumor measurement of 0 %. At that visit, the overall response assessment was stable disease
The median duration of PFS was 3.65 months (Fig. 2). The median OS was 5.59 months; five patients (35.7 %) were alive at 6 months and two patients (14.3 %) at 12 months (Fig. 3).
Pharmacokinetics
For the exposure-response analysis, foretinib trough concentration data were available for 11 patients; however, week 8 tumor size data were available for only nine patients. No relationship was detected between average foretinib trough concentrations after 4 days of dosing and percent change from baseline to week 8 in the sum of the longest tumor diameter (Supplemental Fig. 1).
Moreover, no relationship was detected between average foretinib trough concentrations and the incidence of any AE. Statistical tests were limited by the small sample size.
Safety and adverse events
All patients experienced at least one AE with 14 patients evaluable for safety. Fatigue, constipation and hypertension were the most common AEs, occurring in seven (50 %), five (35.7 %), and five (35.7 %) patients, respectively (Table 4). These were managed with additional medication (e.g. antihypertensives) or dose delay and/or reduction. Of all AEs, 55 % were considered related to foretinib treatment. The most frequent treatment-related grade 3 AE was hypophosphatemia (experienced by three patients). There were no grade 4 treatment-related AEs, but one fatal hemorrhage occurred during cycle 7 and was considered possibly related to foretinib. This patient had severe hemoptysis, and cardiopulmonary resuscitation was unsuccessful.
A total of six other patients died during treatment or follow-up. Four (28.6 %) of these deaths were due to progressive disease and two (14.3 %) due to other causes (pneumonia/respiratory failure and reasons that were not confirmed); none of these six deaths were attributed to the study medication. Two of 14 patients (14 %) required dose reductions to 160 mg due to AEs. No AEs occurred that resulted in study drug discontinuation.
Discussion
Recurrent and/or metastatic SCCHN is a devastating disease for which few effective treatment options are available. This is the first report evaluating a MET inhibitor as a single agent for SCCHN. While the response rate in this two-stage phase II trial did not meet the criteria to allow progression to stage 2, as there were no responders based on RECIST, signs of moderate activity were evident: seven of 14 patients (50 %) experienced SD and six of 14 patients (43 %) showed tumor shrinkage of up to 21 %. Two patients (2/14) (14 %) experienced SD over a period of 13 months or more, exceeding the typical PFS of 3–5 months observed with standard of care [7, 30].
Cetuximab is commonly used in the treatment of recurrent/metastatic disease, either in combination with chemotherapy or as a single agent [31, 32]. The addition of cetuximab to chemotherapy as first-line treatment of patients with recurrent or metastatic SCCHN increased the response rate from 20 % to 36 % (P < 0.001) and median PFS from 3.3 to 5.6 months (P < 0.001) [31]. As a single agent, cetuximab has demonstrated only moderate activity in a phase II study; the best response rate was 13 % (13/103 patients) and 33 % (34/103 patients) experienced SD [32]. The disease control rate was 46 % and the median TTP was 2.3 months [32]. Methotrexate as a single agent has been a standard comparator for clinical studies and has shown response rates of only 3.9 % (6/152 patients; PFS data not reported) [33]. By comparison, foretinib in this (albeit much smaller) study showed a PFS of 3.65 months and a disease stabilization rate of 50 %.
There was no biomarker analysis performed in this study to predict a response to treatment, and it is unclear from the information obtained why the tumors did not respond as predicted by the preclinical data. However, there are many factors that could play a role: foretinib levels in the tumor cells may not be high enough to sufficiently inhibit MET with the intermittent 5/9 schedule, although pharmacodynamic data and clinical data in papillary renal cell [24, 25] and hepatocellular carcinoma [34] do support adequate target inhibition [20]. Notably, inhibition of MET phosphorylation and decreased proliferation in selected tumor biopsies were observed in patients treated with submaximal doses of foretinib [20]. A more likely explanation may be that the in vivo situation is more complex than suggested by in vitro models. One hypothesis may be that additional pathways to those targeted by foretinib may contribute to MET resistance. In future studies, serial biopsy may help elucidate mechanisms of resistance.
We know from other cancer types that compensatory RTK signaling can lead to tumor robustness and resistance [22, 35], and co-targeting may increase efficacy. In non-small cell lung cancer (NSCLC), MET inhibition increased the efficacy of the EGFR inhibitor erlotinib in two large randomized phase II trials [11, 36], despite limited single-agent activity of the respective MET inhibitors in NSCLC [37]. It is therefore reasonable to hypothesize that combined MET/EGFR inhibition may be a promising approach for SCCHN. This is supported by preclinical data showing potent MET/EGFR synergy in SCCHN cell line models [11, 21].
While this is a negative study that did not meet the predefined statistical criteria to proceed to stage 2 of the trial, it is also evident that there is modest activity in a high proportion of SCCHN patients. If significant inhibition of invasion and metastasis is achieved by foretinib treatment, this may be clinically meaningful and efficacy assessment by RECIST may not be optimal in assessing true clinical benefit. In a recent study, time to development of new metastatic lesions was evaluated with a different MET inhibitor (tivantinib) in combination with erlotinib in patients with advanced NSCLC [38]. Time to new metastasis was delayed with tivantinib plus erlotinib versus erlotinib alone (7.3 vs 3.6 months, respectively; P < 0.01). The effect was more pronounced in patients with non-squamous histology (median time to metastatic disease 11.0 vs 3.6 months, respectively; P < 0.01), whilst the objective response rates were only 10 % (7/74 patients) vs 7 % (5/72 patients), respectively (PRs only) [38]. These data further support the evaluation of time to metastatic disease with MET inhibitors in follow-up studies. Furthermore, the anti-angiogenic effect of foretinib may result in a metabolic response against the tumor rather than tumor shrinkage. Future studies should take this into consideration as well as incorporating biomarker analyses to help understand and predict a response to treatment.
Foretinib was well tolerated, with the most common AEs (fatigue, constipation and hypertension) being readily manageable, and the most common foretinib-related laboratory abnormalities (elevated ALT and AST) being asymptomatic. Thus, foretinib may be a good candidate for combination therapy. At this point, no validated biomarkers are available and the small sample size precludes further analysis. There are several potential biomarker candidates, including MET immunohistochemistry [39] and MET copy number [38].
Foretinib is not a MET-specific inhibitor. Like many MET tyrosine kinase inhibitors, it also inhibits the MET-like kinase RON, which is functionally similar to MET [22]. In contrast to other more specific MET inhibitors, foretinib also inhibits VEGFR2 and TIE-2 at clinically achievable concentrations. Inhibition of these multiple targets may have contributed to the modest activity seen; however, further exploration is required [40]. The activity of foretinib against targets in addition to MET may provide a good basis for achieving better outcomes with combination therapy in the future.
No AEs related to MET inhibition were reported; however, AEs related to VEGF inhibition were observed. Observations included night blindness in some patients receiving foretinib [24], other ocular toxicities with crizotinib [41], a MET/ALK inhibitor, and hematologic toxicities with tivantinib [42], an inhibitor of MET. The fact that the three MET inhibitors do not result in similar toxicities suggests that these effects may be potentially unrelated to MET inhibition.
In conclusion, this is the first report of a MET inhibitor used for SCCHN. There is evidence of modest activity, despite the lack of objective responses to treatment. Furthermore, preclinical data, as well as clinical observations, in NSCLC suggest that combination approaches with EGFR inhibition may be promising and should be explored further.
References
Marur S, Forastiere AA (2008) Head and neck cancer: changing epidemiology, diagnosis, and treatment. Mayo Clin Proc 83:489–501
Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60:277–300
Kim L, King T, Agulnik M (2010) Head and neck cancer: changing epidemiology and public health implications. Oncology (Williston Park) 24:915–919–924
Crozier E, Sumer BD (2010) Head and neck cancer. Med Clin North Am 94:1031–1046
Forastiere AA, Goepfert H, Maor M, Pajak TF, Weber R, Morrison W, Glisson B, Trotti A, Ridge JA, Chao C, Peters G, Lee DJ, Leaf A, Ensley J, Cooper J (2003) Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med 349:2091–2098
Vikram B, Strong EW, Shah JP, Spiro R (1984) Second malignant neoplasms in patients successfully treated with multimodality treatment for advanced head and neck cancer. Head Neck Surg 6:734–737
Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S, Erfan J, Zabolotnyy D, Kienzer HR, Cupissol D, Peyrade F, Benasso M, Vynnychenko I, De Raucourt D, Bokemeyer C, Schueler A, Amellal N, Hitt R (2008) Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med 359:1116–1127
Seiwert TY, Jagadeeswaran R, Faoro L, Janamanchi V, Nallasura V, El Dinali M, Yala S, Kanteti R, Cohen EE, Lingen MW, Martin L, Krishnaswamy S, Klein-Szanto A, Christensen JG, Vokes EE, Salgia R (2009) The MET receptor tyrosine kinase is a potential novel therapeutic target for head and neck squamous cell carcinoma. Cancer Res 69:3021–3031
Knowles LM, Stabile LP, Egloff AM, Rothstein ME, Thomas SM, Gubish CT, Lerner EC, Seethala RR, Suzuki S, Quesnelle KM, Morgan S, Ferris RL, Grandis JR, Siegfried JM (2009) HGF and c-Met participate in paracrine tumorigenic pathways in head and neck squamous cell cancer. Clin Cancer Res 15:3740–3750
Cortesina G, Martone T (2006) Molecular metastases markers in head and neck squamous cell carcinoma: review of the literature. Acta Otorhinolaryngol Ital 26:317–325
Xu H, Stabile LP, Gubish CT, Gooding WE, Grandis JR, Siegfried JM (2011) Dual blockade of EGFR and c-Met abrogates redundant signaling and proliferation in head and neck carcinoma cells. Clin Cancer Res 17:4425–4438
Linder C, Linder S, Munck-Wikland E, Auer G, Aspenblad U, Strander H (1998) Evaluation of tissue and serum VEGF in patients with head and neck carcinoma. Angiogenesis 2:365–372
Shang ZJ, Li ZB, Li JR (2006) VEGF is up-regulated by hypoxic stimulation and related to tumour angiogenesis and severity of disease in oral squamous cell carcinoma: in vitro and in vivo studies. Int J Oral Maxillofac Surg 35:533–538
Salven P, Heikkilä P, Anttonen A, Kajanti M, Joensuu H (1997) Vascular endothelial growth factor in squamous cell head and neck carcinoma: expression and prognostic significance. Mod Pathol 10:1128–1133
Fury MG, Zahalsky A, Wong R, Venkatraman E, Lis E, Hann L, Aliff T, Gerald W, Fleisher M, Pfister DG (2007) A Phase II study of SU5416 in patients with advanced or recurrent head and neck cancers. Invest New Drugs 25:165–172
Linkov F, Lisovich A, Yurkovetsky Z, Marrangoni A, Velikokhatnaya L, Nolen B, Winans M, Bigbee W, Siegfried J, Lokshin A, Ferris RL (2007) Early detection of head and neck cancer: development of a novel screening tool using multiplexed immunobead-based biomarker profiling. Cancer Epidemiol Biomarkers Prev 16:102–107
Cohen EE, Davis DW, Karrison TG, Seiwert TY, Wong SJ, Nattam S, Kozloff MF, Clark JI, Yan DH, Liu W, Pierce C, Dancey JE, Stenson K, Blair E, Dekker A, Vokes EE (2009) Erlotinib and bevacizumab in patients with recurrent or metastatic squamous-cell carcinoma of the head and neck: a phase I/II study. Lancet Oncol 10:247–257
Schmitz S, Kaminsky-Forrett M, Henry S, Zanetta S, Geoffrois L, Bompas E, Moxhon A, Guigay J, Machiels JH (2010) Phase II study of figitumumab in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck: GORTEC 2008-02. J Clin Oncol 28:15s(Suppl): Abstract nr 5500
Qian F, Engst S, Yamaguchi K, Yu P, Won KA, Mock L, Lou T, Tan J, Li C, Tam D, Lougheed J, Yakes FM, Bentzien F, Xu W, Zaks T, Wooster R, Greshock J, Joly AH (2009) Inhibition of tumor cell growth, invasion, and metastasis by EXEL-2880 (XL880, GSK1363089), a novel inhibitor of HGF and VEGF receptor tyrosine kinases. Cancer Res 69:8009–8016
Eder JP, Shapiro GI, Appleman LJ, Zhu AX, Miles D, Keer H, Cancilla B, Chu F, Hitchcock-Bryan S, Sherman L, McCallum S, Heath EI, Boerner SA, LoRusso PM (2010) A phase I study of foretinib, a multi-targeted inhibitor of c-Met and vascular endothelial growth factor receptor 2. Clin Cancer Res 16:3507–3516
Liu L, Greger J, Shi H, et al (2010) Foretinib: a multikinase AXL/MET inhibitor. ESMO-IASLC—2nd European Lung Cancer Conference, Geneva, Switzerland; May 2010
Catenacci DV, Cervantes G, Yala S, Nelson EA, El-Hashani E, Kanteti R, El Dinali M, Hasina R, Brägelmann J, Seiwert T, Sanicola M, Henderson L, Grushko TA, Olopade O, Karrison T, Bang YJ, Kim WH, Tretiakova M, Vokes E, Frank DA, Kindler HL, Huet H, Salgia R (2011) RON (MST1R) is a novel prognostic marker and therapeutic target for gastroesophageal adenocarcinoma. Cancer Biol Ther 12:9–46
Liu L, Shi H, Liu Y, Anderson A, Peterson J, Greger J, Martin AM, Gilmer TM (2011) Synergistic effects of foretinib with HER-targeted Agents in MET and HER1- or HER2-coactivated tumor cells. Mol Cancer Ther 10:518–530
Choueiri TK, Vaishampayan UK, Rosenberg JE, Logan T, Harzstark AL, Rini BI, Srinivas S, Adams LM, Sherman LJ, Ottesen LH, McDermott DF, Bottaro DP, Marston Linehan W, Srinivasan R (2012) A phase II and biomarker study (MET111644) of the dual Met/VEGFR-2 inhibitor foretinib in patients with sporadic and hereditary papillary renal cell carcinoma: final efficacy, safety, and PD results. J Clin Oncol 30(Suppl 5): Abstract nr 355
Srinivasan R, Bottaro DP, Choueiri TK, Rosenberg JE, Logan T, Harzstark AL, Rini BI, Srinivas S, Adams LM, Laubscher K, Ottesen LH, McDermott DF, Marston Linehan W (2012) Correlation of germline MET mutation with response to the dual Met/VEGFR-2 inhibitor foretinib in patients with sporadic and hereditary papillary renal cell carcinoma: Results from a multicenter phase II study (MET111644). J Clin Oncol 30(Suppl 5): Abstract nr 372
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Simon R (1989) Optimal two-stage designs for phase II clinical trials. Control Clin Trials 10:1–10
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216
Cohen EE, Haraf DJ, Kunnavakkam R, Stenson KM, Blair EA, Brockstein B, Lester EP, Salama JK, Dekker A, Williams R, Witt ME, Grushko TA, Dignam JJ, Lingen MW, Olopade OI, Vokes EE (2010) Epidermal growth factor receptor inhibitor gefitinib added to chemoradiotherapy in locally advanced head and neck cancer. J Clin Oncol 28:3336–3343
Shin DM, Khuri FR (2011) Advances in the management of recurrent or metastatic squamous cell carcinoma of the head and neck. Head Neck. doi: 10.1002/hed.21910. [Epub ahead of print]
Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S, Erfan J, Zabolotnyy D, Kienzer H-R, Cupissol D, Peyrade F, Benasso M, Vynnychenko I, De Raucourt D, Bokemeyer C, Schueler A, Amellal N, Hitt R (2008) Platinum-based chemotherapy plus cetuximab in head and neck cancer. New Engl J Med 389:1116–1127
Vermorken JB, Trigo J, Hitt R, Koralewski P, Diaz-Rubio E, Rolland F, Knecht R, Amellal N, Schueler A, Baselga J (2007) Open-label, uncontrolled, multicenter phase II study to evaluate the efficacy and toxicity of cetuximab as a single agent in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck who failed to respond to platinum-based therapy. J Clin Oncol 25:2171–2177
Stewart JSW, Cohen EEW, Licitra L, Van Herpen CML, Khorprasert C, Soulieres D, Vodvarka P, Rischin D, Garin AM, Hirsch FR, Varella-Garcia M, Ghiorghiu S, Hargreaves L, Armour A, Speake G, Swaisland A, Vokes EE (2009) Phase III study of gefitinib compared with intravenous methotrexate for recurrent squamous cell carcinoma of the head and neck. J Clin Oncol 27:1864–1871
Yau T, Yen C-J, Chen P-J (2011) A phase I/II study of foretinib, an oral multikinase inhibitor targeting MET, RON, AXL, TIE-2, and VEGFR in advanced hepatocellular carcinoma (HCC). J Hepatol 54(Suppl 1):S268
Maulik G, Shrikhande A, Kijima T, Ma PC, Morrison PT, Salgia R (2002) Role of the hepatocyte growth factor receptor, c-Met, in oncogenesis and potential for therapeutic inhibition. Cytokine Growth Factor Rev 13:41–59
Engelman JA, Zejnullahu K, Mitsudomi T, Song Y, Hyland C, Park JO, Lindeman N, Gale CM, Zhao X, Christensen J, Kosaka T, Holmes AJ, Rogers AM, Cappuzzo F, Mok T, Lee C, Johnson BE, Cantley LC, Jänne PA (2007) MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science 316:1039–1043
Wakelee HA, Gettinger SN, Engelman JA, Janne PA, West HJ, Subramaniam DS, Leach JW, Wax MB, Yaron Y, Lara P Jr (2010) A phase Ib/II study of XL184 (BMS 907351) with and without erlotinib (E) in patients (pts) with non-small cell lung cancer (NSCLC). J Clin Oncol 28:15s(Suppl): Abstract nr 3017
Sequist LV, von Pawel J, Garmey EG, Akerley WL, Brugger W, Ferrari D, Chen Y, Costa DB, Gerber DE, Orlov S, Ramlau R, Arthur S, Gorbachevsky I, Schwartz B, Schiller JH (2011) Randomized phase II study of erlotinib plus tivantinib versus erlotinib plus placebo in previously treated non–small-cell lung cancer. J Clin Oncol 29:3307–3315
Spigel DR, Ervin TJ, Ramlau R, Daniel DB, Goldschmidt JH, Blumenschein GR, Krzakowski MJ, Robinet G, Clement-Duchene C, Barlesi F, Govindan R, Patel T, Orlov SV, Wertheim MS, Zha J, Pandita A, Yu W, Yauch RL, Patel PH, Peterson AC (2011) Final efficacy results from OAM4558g, a randomized phase II study evaluating MetMAb or placebo in combination with erlotinib in advanced NSCLC. J Clin Oncol 29: (Suppl): Abstract nr 7505
Chen LF, Cohen EE, Grandis JR (2010) New strategies in head and neck cancer: understanding resistance to epidermal growth factor receptor inhibitors. Clin Cancer Res 16:2489–2495
Crizotinib label http://labeling.pfizer.com/showlabeling.aspx?id=676
Zucali P, Santoro A, Rodriguez-Lope C, Simonelli M, Camacho LH, Senzer NN, Bolondi L, Lamar M, Abbadessa G, Schwartz BE (2010) Final results from ARQ 197-114: a Phase 1b safety trial evaluating the c-MET inhibitor ARQ 197 in cirrhotic patients with hepatocellular carcinoma. J Clin Oncol 28:15s(Suppl): Abstract nr 4137
Acknowledgments
Funding for this study was provided by GlaxoSmithKline (NCT00725764). All listed authors meet the criteria for authorship set forth by the International Committee for Medical Journal Editors. Editorial support in the form of copyediting, development of a draft outline, assembling tables and figures, collating author comments and referencing was provided by Jim Kesslick of CONNEXION Healthcare, Newtown, PA and MediTech Media, Manchester, UK, funded by GlaxoSmithKline. Grant support for MET-related research was provided from a Flight Attendant Medical Research Institute (FAMRI) Young Clinical Scientist Award (T.Y. Seiwert).
Conflicts of Interest
Dr. Seiwert and Dr. Sarantopoulos declared no conflicts of interest; Dr. Kallender and Dr. McCallum are employees of, and have equity interest in, GlaxoSmithKline; Dr. Keer is an employee of Exelixis; Dr. Blumenschein received research funding from GlaxoSmithKline for the trial.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
Relationship between foretinib trough concentration and percentage change from baseline in tumor size. Average trough concentration on study days 5, 19, 33 and 47 (JPEG 10 kb)
High Resolution Image 1
(TIFF 756 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Seiwert, T., Sarantopoulos, J., Kallender, H. et al. Phase II trial of single-agent foretinib (GSK1363089) in patients with recurrent or metastatic squamous cell carcinoma of the head and neck. Invest New Drugs 31, 417–424 (2013). https://doi.org/10.1007/s10637-012-9861-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-012-9861-3