Abstract
The interesting data reported by Bernhardt et al. strengthen the diagnostic benefit of CMR in patients with ischemic cardiomyopathy. Consequently, the presence, location and size of the CMR-determined scar tissue may be used for better risk stratification in patients with ischemic cardiomyopathy eligible for ICD therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over the past years considerable progress has been made in the field of cardiovascular magnetic resonance (CMR), providing accurate evaluation of left ventricular function particularly in patients prone to heart failure due to both ischemic and non-ischemic cardiomyopathy [1–14]. In particular, high-resolution contrast-enhanced CMR has been used to visualize myocardial fibrosis with a high accuracy [15–22]. For instance, in patients with acute myocardial infarction, the injured myocardium shows increased CMR contrast compared to normal myocardium when imaged by delayed gadolinium enhancement. The transmural extent of delayed gadolinium enhancement predicts functional outcome after interventional procedures performed in patients with acute myocardial infarction and chronic ischemic heart disease [23–32]. Not only in the setting of an acute myocardial infarction, but also in patients with various manifestations of cardiomyopathy, evidence of delayed gadolinium enhancement may have important clinical and prognostic implications [32–36]. In patients eligible for cardiac resynchronization therapy, the presence of scar tissue may have consequences for implanting a biventricular device and subsequent accurate lead positioning [37–51]. In patients with hypertrophic cardiomyopathy, the presence of fibrotic tissue may result in increased occurrence of ventricular arrhythmias [52–57]. Recently, it has been shown that presence and quantity of late enhancement is correlated with cardiovascular events and arrhythmias in patients with dilated cardiomyopathy [58–61].
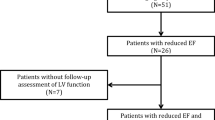
In the present issue of the International Journal of Cardiovascular Imaging, Bernhardt et al. [62] address the hypothesis that infarct size in patients with ischemic cardiomyopathy is related to spontaneous monomorphic ventricular tachycardia which may be determined by contrast-enhanced CMR. The purpose of the study was to establish the relationship between functional and contrast-enhanced CMR findings and spontaneous ventricular tachy-arrhythmias in patients with ischemic cardiomyopathy who underwent implantable cardioverter-defibrillator (ICD) therapy. A total of 41 patients with ischemic cardiomyopathy and an indication for ICD therapy underwent delayed gadolinium enhancement CMR for quantification of left ventricular volumes, function and myocardial scar tissue before subsequent implantation of an ICD device. During a follow-up period of 1,184 ± 442 days 68 monomorphic and 14 polymorphic types of ventricular tachycardia could be observed in 12 patients. Patients with monomorphic ventricular tachycardia had more extensive scar tissue than patients with polymorphic ventricular tachycardia (mean 25% vs. mean 12% of myocardial mass). Moreover, myocardial infarction involved more segments in the region of the left anterior descending coronary artery (LAD) than in patients with polymorphic ventricular tachycardia (86 vs. 20%). During the long-term follow-up period, patients with spontaneous monomorphic ventricular tachycardia had more infarcted tissue, being more often present in the LAD region, than patients with polymorphic events. As a result, the most important finding of the study was a significant difference between patients with monomorphic and polymorphic events. Patients with monomorphic ventricular arrhythmias during follow up had more dilated ventricles, decreased ejection fractions and larger scar volumes than patients with polymorphic events. More segments in the LAD region showed scar patterns in patients with monomorphic events. This larger extent of scar tissue in the LAD region was independent of the indication for ICD implantation compared to patients with polymorphic ventricular arrhythmias.
Several studies have recently focused on the relation between the extent of myocardial scar tissue and the incidence of ventricular arrhythmias in patients with ischemic cardiomyopathy. Fernandes et al. [63] determined whether mechanical behavior of left ventricular wall segments containing different degrees of scar tissue and localized at different distances from the interface between infarcted and noninfarcted myocardial tissue could assist in predicting inducibility of monomorphic ventricular tachycardia in 46 patients with ischemic cardiomyopathy. They showed that inducible patients had more infarcted and border zone sectors and a shorter time to peak circumferential shortening strain than did noninducible patients in the border zone of adjacent and infarcted regions. Yokokawa et al. [64] sought to clarify the relationship between the scar characteristics and occurrence of sustained ventricular tachycardias in 47 patients with advanced heart failure. The volume of the hyperenhanced areas and total number of hyperenhanced segments were greater in patients with sustained ventricular tachycardias than in those without. The presence and magnitude of the nontransmural scar tissue predicted sustained ventricular tachycardias in patients with advanced heart failure. Di Bella et al. [65] investigated the relationship between nonsustained ventricular tachycardia and left ventricular dilatation, function, remodeling, and CMR-assessed scar tissue extent in patients with previous myocardial infarction. It was shown that necrotic and viable myocardium coexistence within the same wall segments predicted occurrence of nonsustained ventricular tachycardia in patients without left ventricular dilatation, whereas left ventricular mass and end-systolic volume were predictors of nonsustained ventricular tachycardia in those with left ventricular dilatation. Roes et al. [66] recently studied 91 patients with ischemic cardiomyopathy for a mean duration of 8.5 months after ICD implantation for ICD therapy in spontaneous ventricular tachycardias. The authors showed that patients with appropriate ICD therapy had larger myocardial scar detected by CMR than patients without appropriate ICD therapy. They concluded that infarct tissue heterogeneity on contrast-enhanced CMR was the strongest predictor of spontaneous ventricular arrhythmia with subsequent ICD therapy (as surrogate of sudden cardiac death) among other clinical and CMR variables in patients with previous myocardial infarction. However, the authors did not distinguish between monomorphic and polymorphic ventricular tachycardia, and rather addressed ICD therapy itself.
Apart from the value of scar identification in patients with left ventricular dysfunction, delayed gadolinium enhancement CMR can also be used to assess the long-term arrhythmia recurrence rate and outcome in patients with scar-related ventricular tachycardia of right ventricular origin [67–69]. Wijnmaalen et al. [69] studied 29 (45%) patients diagnosed with arrhythmogenic right ventricular dysplasia according to Task Force criteria (TF+) and 35 (55%) with right ventricular scar of undetermined origin (TF−) at the end of follow-up (64 ± 42 months). The authors demonstrated that scar-related right ventricular tachycardias have a high recurrence rate in TF+ and TF− patients. Patients presenting with a fast index ventricular tachycardia are at high risk for recurrence of fast ventricular tachycardias and may benefit most from ICD therapy.
To summarize, the interesting data reported by Bernhardt et al. [62] strengthen the diagnostic benefit of using CMR in patients with ischemic cardiomyopathy. Consequently, the presence, location and size of the CMR-determined scar tissue may be used for better risk stratification in patients with ischemic cardiomyopathy eligible for ICD therapy.
References
de Roos A, Matheijssen NA, Doornbos J, van Dijkman PR, van Rugge PR, van der Wall EE (1991) Myocardial infarct sizing and assessment of reperfusion by magnetic resonance imaging: a review. Int J Card Imaging 7:133–138
van Rugge FP, Boreel JJ, van der Wall EE et al (1991) Cardiac first-pass and myocardial perfusion in normal subjects assessed by sub-second Gd-DTPA enhanced MR imaging. J Comput Assist Tomogr 15:959–965
van der Wall, Vliegen HW, de Roos A, Bruschke AV (1995) Magnetic resonance imaging in coronary artery disease. Circulation 92:2723–2739
Nollen GJ, Groenink M, Tijssen JG, van der Wall EE, Mulder BJ (2004) Aortic stiffness and diameter predict progressive aortic dilatation in patients with Marfan syndrome. Eur Heart J 25:1146–1152
van Rugge FP, van der Wall EE, Bruschke AV (1992) New developments in pharmacologic stress imaging. Am Heart J 124:468–485
van Rugge FP, van der Wall EE, van Dijkman PR, Louwerenburg HW, de Roos A, Bruschke AV (1992) Usefulness of ultrafast magnetic resonance imaging in healed myocardial infarction. Am J Cardiol 70:1233–1237
Matheijssen NA, Louwerenburg HW, van Rugge FP et al (1996) Comparison of ultrafast dipyridamole magnetic resonance imaging with dipyridamole SestaMIBI SPECT for detection of perfusion abnormalities in patients with one-vessel coronary artery disease: assessment by quantitative model fitting. Magn Reson Med 35:221–228
Matheijssen NA, de Roos A, Doornbos J, Reiber JH, Waldman GJ, van der Wall EE (1993) Left ventricular wall motion analysis in patients with acute myocardial infarction using magnetic resonance imaging. Magn Reson Imaging 11:485–492
Holman ER, van Jonbergen HP, van Dijkman PR, van der Laarse A, de Roos A, van der Wall EE (1993) Comparison of magnetic resonance imaging studies with enzymatic indexes of myocardial necrosis for quantification of myocardial infarct size. Am J Cardiol 71:1036–1040
Matheijssen NA, Baur LH, Reiber JH et al (1996) Assessment of left ventricular volume and mass by cine magnetic resonance imaging in patients with anterior myocardial infarction intra-observer and inter-observer variability on contour detection. Int J Card Imaging 12:11–19
van der Geest RJ, Niezen RA, van der Wall EE, de Roos A, Reiber JH (1998) Automated measurement of volume flow in the ascending aorta using MR velocity maps: evaluation of inter- and intra observer variability in healthy volunteers. J Comput Assist Tomogr 22:904–911
Nemes A, Geleijnse ML, van Geuns RJ et al (2008) Dobutamine stress MRI versus threedimensional contrast echocardiography: it’s all black and white. Neth Heart J 16:217–218
Groenink M, Lohuis TA, Tijssen JG et al (1999) Survival and complication free survival in Marfan’s syndrome: implications of current guidelines. Heart 82:499–504
van Rugge FP, Holman ER, van der Wall EE et al (1993) Quantitation of global and regional left ventricular function by cine magnetic resonance imaging during dobutamine stress in normal human subjects. Eur Heart J 14:456–463
van der Wall EE, van Dijkman PR, de Roos A et al (1990) Diagnostic significance of gadolinium-DTPA (diethylenetriamine penta-acetic acid) enhanced magnetic resonance imaging in thrombolytic treatment for acute myocardial infarction: its potential in assessing reperfusion. Br Heart J 63:12–17
Nijveldt R, Beek AM, Hirsch A et al (2008) ‘No-reflow’ after acute myocardial infarction: direct visualisation of microvascular obstruction by gadolinium enhanced CMR. Neth Heart J 16:179–181
Oemrawsingh PV, Mintz GS, Schalij MJ, Zwinderman AH, Jukema JW, van der Wall EE (2003) Intravascular ultrasound guidance improves angiographic and clinical outcome of stent implantation for long coronary artery stenoses: final results of a randomized comparison with angiographic guidance (TULIP Study). Circulation 107:62–67
van Dijkman PR, van der Wall EE, de Roos A et al (1991) Acute, subacute, and chronic myocardial infarction: quantitative analysis of gadolinium-enhanced MR images. Radiology 180:147–151
van der Wall EE, den Hollander W, Heidendal GA, Westera G, Majid PA, Roos JP (1981) Dynamic myocardial scintigraphy with 123I-labeled free fatty acids in patients with myocardial infarction. Eur J Nucl Med 6:383–389
van der Laarse A, Kerkhof PL, Vermeer F et al (1988) Relation between infarct size and left ventricular performance assessed in patients with first acute myocardial infarction randomized to intracoronary thrombolytic therapy or to conventional treatment. Am J Cardiol 61:1–7
Torn M, Bollen WL, van der Meer FJ, van der Wall EE, Rosendaal FR (2005) Risks of oral anticoagulant therapy with increasing age. Arch Intern Med 165:1527–1532
de Roos A, Matheijssen NA, Doornbos J, van Dijkman PR, van Voorthuisen AE, van der Wall EE (1990) Myocardial infarct size after reperfusion therapy: assessment with Gd-DTPA-enhanced MR imaging. Radiology 176:517–521
Slart RH, Bax JJ, van Veldhuisen DJ, van der Wall EE, Dierckx RA, Jager PL (2006) Imaging techniques in nuclear cardiology for the assessment of myocardial viability. Int J Cardiovasc Imaging 22:63–80
van der Wall EE, Heidendal GA, den Hollander W, Westera G, Roos JP (1980) I-123 labeled hexadecenoic acid in comparison with thallium-201 for myocardial imaging in coronary heart disease. A preliminary study. Eur J Nucl Med 5:401–405
Underwood SR, Bax JJ, vom Dahl J et al (2004) Study Group of the European Society of Cardiology. Imaging techniques for the assessment of myocardial hibernation. Report of a study group of the European society of cardiology. Eur Heart J 25:815–836
Kleijn SA, Kamp O (2009) Clinical application of three-dimensional echocardiography: past, present and future. Neth Heart J 17:18–24
Kamp O (2008) History of echocardiography in the Netherlands: 30 years of education and clinical applications. Neth Heart J 16:16–20
Cramer MM, De Boeck BW (2007) Three-dimensional echocardiography and left bundle branch block: prime time in cardiology. Neth Heart J 15:87–88
van Eck-Smit BL, van der Wall EE, Kuijper AF, Zwinderman AH, Pauwels EK (1993) Immediate thallium-201 reinjection following stress imaging: a time-saving approach for detection of myocardial viability. J Nucl Med 34:737–743
Bakx AL, van der Wall EE, Braun S, Emanuelsson H, Bruschke AV, Kobrin I (1995) Effects of the new calcium antagonist mibefradil (Ro 40–5967) on exercise duration in patients with chronic stable angina pectoris: a multicenter, placebo-controlled study. Ro 40–5967 International study group. Am Heart J 130:748–757
Schuijf JD, Bax JJ, van der Wall EE (2007) Anatomical and functional imaging techniques: basically similar or fundamentally different? Neth Heart J 15:43–44
Ten Cate FJ (2009) Cardiomyopathies: a revolution in molecular medicine and cardiac imaging. Neth Heart J 17:456–457
Portegies MC, Schmitt R, Kraaij CJ et al (1991) Lack of negative inotropic effects of the new calcium antagonist Ro 40–5967 in patients with stable angina pectoris. J Cardiovasc Pharmacol 18:746–751
Kaandorp TA, Lamb HJ, Viergever EP et al (2007) Scar tissue on contrast-enhanced MRI predicts left ventricular remodelling after acute infarction. Heart 93:375–376
Schuijf JD, Bax JJ, van der Wall EE (2007) Anatomical and functional imaging techniques: basically similar or fundamentally different? Neth Heart J 15:43–44
Assomull RG, Prasad SK, Lyne J et al (2006) Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol 48:1977–1985
Borleffs CJ, Wilde AA, Cramer MJ, Wever E, Mosterd A (2007) Clinical implementation of guidelines for cardioverter defibrillator implantation: lost in translation? Neth Heart J 15:129–132
Molhoek SG, Bax JJ, van Erven L et al (2004) Comparison of benefits from cardiac resynchronization therapy in patients with ischemic cardiomyopathy versus idiopathic dilated cardiomyopathy. Am J Cardiol 93:860–863
Ypenburg C, Sieders A, Bleeker GB et al (2007) Myocardial contractile reserve predicts improvement in left ventricular function after cardiac resynchronization therapy. Am Heart J 154:1160–1165
Bleeker GB, Kaandorp TA, Lamb HJ et al (2006) Effect of posterolateral scar tissue on clinical and echocardiographic improvement after cardiac resynchronization therapy. Circulation 113:969–976
Ypenburg C, Schalij MJ, Bleeker GB et al (2006) Extent of viability to predict response to cardiac resynchronization therapy in ischemic heart failure patients. J Nucl Med 47:1565–1570
Tops LF, Schalij MJ, Holman ER, van Erven L, van der Wall EE, Bax JJ (2006) Right ventricular pacing can induce ventricular dyssynchrony in patients with atrial fibrillation after atrioventricular node ablation. J Am Coll Cardiol 48:1642–1648
Ypenburg C, Schalij MJ, Bleeker GB et al (2007) Impact of viability and scar tissue on response to cardiac resynchronization therapy in ischaemic heart failure patients. Eur Heart J 28:33–41
Ypenburg C, Roes SD, Bleeker GB et al (2007) Effect of total scar burden on contrast-enhanced magnetic resonance imaging on response to cardiac resynchronization therapy. Am J Cardiol 99:657–660
Molhoek SG, van Erven L, Bootsma M, Steendijk P, van der Wall EE, Schalij MJ (2004) QRS duration and shortening to predict clinical response to cardiac resynchronization therapy in patients with end-stage heart failure. Pacing Clin Electrophysiol 27:308–313
Ypenburg C, Westenberg JJ, Bleeker GB et al (2008) Noninvasive imaging in cardiac resynchronization therapy—part 1: selection of patients. Pacing Clin Electrophysiol 31:1475–1499
Ypenburg C, Van De Veire N, Westenberg JJ et al (2008) Noninvasive imaging in cardiac resynchronization therapy-Part 2: follow-up and optimization of settings. Pacing Clin Electrophysiol 31:1628–1639
Marsan NA, Bleeker GB, Van Bommel RJ et al (2009) Cardiac resynchronization therapy in patients with ischemic versus non-ischemic heart failure: differential effect of optimizing interventricular pacing interval. Am Heart J 158:769–776
Ypenburg C, van der Wall EE, Schalij MJ, Bax JJ (2008) Imaging in cardiac resynchronisation therapy. Neth Heart J 16:S36–S40
Bleeker GB, Schalij MJ, Van der Wall EE, Bax JJ (2006) Postero-lateral scar tissue resulting in non-response to cardiac resynchronization therapy. J Cardiovasc Electrophysiol 17:899–901
Taylor AJ, Elsik M, Broughton A et al (2010) Combined dyssynchrony and scar imaging with cardiac magnetic resonance imaging predicts clinical response and long-term prognosis following cardiac resynchronization therapy. Europace 12:708–713
Germans T, Nijveldt R, Brouwer WP et al (2010) The role of cardiac magnetic resonance imaging in differentiating the underlying causes of left ventricular hypertrophy. Neth Heart J 18:135–143
van der Wall EE, Siebelink HM, Bax JJ (2010) Evaluation of hypertrophic cardiomyopathy: new horizons for CMR? Neth Heart J 18:116–117
Adabag AS, Maron BJ, Appelbaum E et al (2008) Occurrence and frequency of arrhythmias in hypertrophic cardiomyopathy in relation to delayed enhancement on cardiovascular magnetic resonance. J Am Coll Cardiol 51:1369–1374
Kwon DH, Setser RM, Popović ZB et al (2008) Association of myocardial fibrosis, electrocardiography and ventricular tachyarrhythmia in hypertrophic cardiomyopathy: a delayed contrast enhanced MRI study. Int J Cardiovasc Imaging 24:617–625
Suk T, Edwards C, Hart H, Christiansen JP (2008) Myocardial scar detected by contrast-enhanced cardiac magnetic resonance imaging is associated with ventricular tachycardia in hypertrophic cardiomyopathy patients. Heart Lung Circ 17:370–374
Dimitrow PP, Klimeczek P, Vliegenthart R et al (2008) Late hyperenhancement in gadolinium-enhanced magnetic resonance imaging: comparison of hypertrophic cardiomyopathy patients with and without nonsustained ventricular tachycardia. Int J Cardiovasc Imaging 24:77–83
Schmidt A, Azevedo CF, Cheng A et al (2007) Infarct tissue heterogeneity by magnetic resonance imaging identifies enhanced cardiac arrhythmia susceptibility in patients with left ventricular dysfunction. Circulation 115:2006–2014
Wu KC, Weiss RG, Thiemann DR et al (2008) Late gadolinium enhancement by cardiovascular magnetic resonance heralds and adverse prognosis in nonischemic cardiomyopathy. J Am Coll Cardiol 51:2414–2421
Hombach V, Merkle N, Torzewski J et al (2009) Electrocardiographic and cardiac magnetic resonance imaging parameters as predictors of a worse outcome in patients with idiopathic dilated cardiomyopathy. Eur Heart J 30:2011–2018
Bogun FM, Desjardins B, Good E et al (2009) Delayed-enhanced magnetic resonance imaging in nonischemic cardiomyopathy: utility for identifying the ventricular arrhythmia substrate. J Am Coll Cardiol 53:1138–1145
Bernhardt P, Stiller S, Kottmair E et al (2010) Myocardial scar extent evaluated by cardiac magnetic resonance imaging in ICD patients: relationship to spontaneous VT during long-term follow-up. Int J Cardiovasc Imaging, 19 Oct 2010 [Epub ahead of print]
Fernandes VR, Wu KC, Rosen BD et al (2007) Enhanced infarct border zone function and altered mechanical activation predict inducibility of monomorphic ventricular tachycardia in patients with ischemic cardiomyopathy. Radiology 245:712–719
Yokokawa M, Tada H, Koyama K et al (2009) The characteristics and distribution of the scar tissue predict ventricular tachycardia in patients with advanced heart failure. Pacing Clin Electrophysiol 32:314–322
Di Bella G, Passino C, Aquaro GD et al (2010) Different substrates of non-sustained ventricular tachycardia in post-infarction patients with and without left ventricular dilatation. J Card Fail 16:61–68
Roes SD, Borleffs JW, van der Geest RJ et al (2009) Infarct tissue heterogeneity assessed with contrast-enhanced MRI predicts spontaneous ventricular arrhythmia in patients with ischemic cardiomyopathy and implantable cardioverter-defibrillator. Circ Cardiovasc Imaging 2:183–190
Atwater BD, Daubert JP (2010) Can we improve the identification of ventricular scar to guide substrate-based ventricular tachycardia ablation? J Cardiovasc Electrophysiol 21:685–687
de Groot NM, Zeppenfeld K, Wijffels MC et al (2006) Ablation of focal atrial arrhythmia in patients with congenital heart defects after surgery: role of circumscribed areas with heterogeneous conduction. Heart Rhythm 3:526–535
Wijnmaalen AP, Schalij MJ, Bootsma M et al (2009) Patients with scar-related right ventricular tachycardia: determinants of long-term outcome. J Cardiovasc Electrophysiol 20:1119–1127
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Editorial comment on to the article of Bernhardt et al. (doi:10.1007/s10554-010-9726-9).
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
van der Wall, E.E., Zeppenfeld, K., Bax, J.J. et al. CMR-determined scar volume: predictive for ventricular tachycardias?. Int J Cardiovasc Imaging 27, 989–993 (2011). https://doi.org/10.1007/s10554-010-9744-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-010-9744-7