Abstract
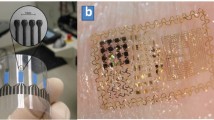
Continuous monitoring of aberrant electrical rhythms during heart injury and repair requires prolonged data acquisition. We hereby developed a wearable microelectrode membrane that could be adherent to the chest of neonatal mice for in situ wireless recording of electrocardiogram (ECG) signals. The novel dry-contact membrane with a meshed parylene-C pad adjacent to the microelectrodes and the expandable meandrous strips allowed for varying size of the neonates. The performance was evaluated at the system level; specifically, the ECG signals (μV) acquired from the microelectrodes underwent two-stage amplification, band-pass filtering, and optical data transmission by an infrared Light Emitting Diode (LED) to the data-receiving unit. The circuitry was prototyped on a printed circuit board (PCB), consuming less than 300 μW, and was completely powered by an inductive coupling link. Distinct P waves, QRS complexes, and T waves of ECG signals were demonstrated from the non-pharmacologically sedated neonates at ~600 beats per minutes. Thus, we demonstrate the feasibility of both real-time and wireless monitoring cardiac rhythms in a neonatal mouse (17–20 mm and <1 g) via dry-contact microelectrode membrane; thus, providing a basis for diagnosing aberrant electrical conduction in animal models of cardiac injury and repair.




Similar content being viewed by others
References
O. Bergmann, R.D. Bhardwaj, S. Bernard, S. Zdunek, F. Barnabe-Heider, S. Walsh, J. Frisen, Evidence for cardiomyocyte renewal in humans. Science 324(5923), 98–102 (2009). doi:10.1126/science.1164680
K. Bersell, S. Arab, B. Haring, B. Kuhn, Neuregulin1/ErbB4 signaling induces cardiomyocyte proliferation and repair of heart injury. Cell 138(2), 257–270 (2009). doi:10.1016/j.cell.2009.04.060
A.L. Bui, G.C. Fonarow, Home monitoring for heart failure management. J. Am. Coll. Cardiol. 59(2), 97–104 (2012)
H. Cao, S. Rao, S.-j. Tang, H.F. Tibbals, S. Spechler, J.-C. Chiao, Batteryless implantable dual-sensor capsule for esophageal reflux monitoring. Gastrointest. Endosc. 77(4), 649–653 (2013)
H. Cao, F. Yu, Y. Zhao, X. Zhang, J. Tai, J. Lee . . . N. C. Chi. Wearable multi-channel microelectrode membranes for elucidating electrophysiological phenotypes of injured myocardium. Integr Biol (2014)
Y.M. Chi, T.-P. Jung, G. Cauwenberghs, Dry-contact and noncontact biopotential electrodes: methodological review. IEEE Rev. Biomed. Eng. 3, 106–119 (2010)
P.C. Hsieh, V.F. Segers, M.E. Davis, C. MacGillivray, J. Gannon, J.D. Molkentin, R.T. Lee, Evidence from a genetic fate-mapping study that stem cells refresh adult mammalian cardiomyocytes after injury. Nat. Med. 13(8), 970–974 (2007). doi:10.1038/nm1618
G.N. Huang, J.E. Thatcher, J. McAnally, Y. Kong, X. Qi, W. Tan, J.A. Hill, C/EBP transcription factors mediate epicardial activation during heart development and injury. Science 338(6114), 1599–1603 (2012)
K. Kikuchi, J.E. Holdway, A.A. Werdich, R.M. Anderson, Y. Fang, G.F. Egnaczyk, K.D. Poss, Primary contribution to zebrafish heart regeneration by gata4+ cardiomyocytes. Nature 464(7288), 601–605 (2010)
S. Kulandavelu, D. Qu, N. Sunn, J. Mu, M.Y. Rennie, K.J. Whitelely … S.L. Adamson. Embryonic and neonatal phenotyping of genetically engineered mice. ILAR J. 47(2), 103–117 (2006). doi: 10.1093/ilar.47.2.s103
C.L. Lien, M.R. Harrison, T.L. Tuan, V.A. Starnes, Heart repair and regeneration: recent insights from zebrafish studies. Wound Repair Regen. 20(5), 638–646 (2012)
J. Narula, N. Haider, R. Virmani, T.G. DiSalvo, F.D. Kolodgie, R.J. Hajjar, B.-A. Khaw, Apoptosis in myocytes in end-stage heart failure. N. Engl. J. Med. 335(16), 1182–1189 (1996)
G. Olivetti, R. Abbi, F. Quaini, J. Kajstura, W. Cheng, J.A. Nitahara, S. Krajewski, Apoptosis in the failing human heart. N. Engl. J. Med. 336(16), 1131–1141 (1997)
E.R. Porrello, A.I. Mahmoud, E. Simpson, J.A. Hill, J.A. Richardson, E.N. Olson, H.A. Sadek, Transient regenerative potential of the neonatal mouse heart. Science 331(6020), 1078–1080 (2011)
P. Sun, Y. Zhang, F. Yu, E. Parks, A. Lyman, Q. Wu, T.K. Hsiai, Micro-electrocardiograms to study post-ventricular amputation of zebrafish heart. Ann. Biomed. Eng. 37(5), 890–901 (2009). doi:10.1007/s10439-009-9668-3
F. Yu, R. Li, E. Parks, W. Takabe, T.K. Hsiai, Electrocardiogram signals to assess zebrafish heart regeneration: implication of long QT intervals. Ann. Biomed. Eng. 38(7), 2346–2357 (2010). doi:10.1007/s10439-010-9993-6
F. Yu, Y. Zhao, J. Gu, K.L. Quigley, N.C. Chi, Y.-C. Tai, T.K. Hsiai, Flexible microelectrode arrays to interface epicardial electrical signals with intracardial calcium transients in zebrafish hearts. Biomed. Microdevices 14(2), 357–366 (2012)
Acknowledgments
The studies were supported by the National Institutes of Health R01HL-083015 (T.K.H.), R01HD069305-01 (N.C.C., T.K.H.), R01HL111437 (T.K.H.), and R01HL096121(C.L.L.).
Author information
Authors and Affiliations
Corresponding author
Additional information
Yu Zhao, Hung Cao and Tyler Beebe contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Video 1
Adult zebrafish are placed in a jacket with 4 electrodes proximal to the heart, similar to the neonatal mouse design in Fig 1. ECG signals are acquired by the electrode, and transmitted to the monitor where signals can be monitored in real-time. (MP4 108175 kb)
Rights and permissions
About this article
Cite this article
Zhao, Y., Cao, H., Beebe, T. et al. Dry-contact microelectrode membranes for wireless detection of electrical phenotypes in neonatal mouse hearts. Biomed Microdevices 17, 40 (2015). https://doi.org/10.1007/s10544-014-9912-y
Published:
DOI: https://doi.org/10.1007/s10544-014-9912-y