Abstract
Purpose
BCVI may lead to ischemic stroke, disability, and death, while being often initially clinically silent. Screening criteria for BCVI based on clinical findings and trauma mechanism have improved detection, with Denver criteria being most common. Up to 30% of patients do not meet BCVI screening criteria. The aim of this study was to analyze the effect of augmented Denver criteria on detection, and to determine the relative risk for ischemic stroke.
Methods
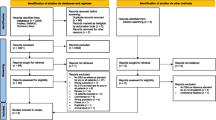
Denver screening criteria were augmented by any high-energy trauma of the cervical spine, thorax, abdomen, or pelvis. All acute blunt trauma WBCT including CT angiography (CTA) over a period of 38 months were reviewed retrospectively by two Fellowship-trained radiologists, as well as any cerebral imaging after the initial trauma.
Results
1544 WBCT studies included 374 CTA (m/f = 271/103; mean age 41.5 years). Most common mechanisms of injury were MVA (51.5%) and fall from a height (22.3%). We found 72 BCVI in 56 patients (15.0%), with 13 (23.2%) multiple lesions. The ICA was affected in 49 (68.1%) and the vertebral artery in 23 (31.9%) of cases. The most common injury level was C2, with Biffl grades I and II most common in ICA, and II and IV in VA. Interobserver agreement was substantial (Kappa = 0.674). Of 215 patients imaged, 16.1% with BCVI and 1.9% of the remaining cases had cerebral ischemic stroke (p < .0001; OR = 9.77; 95% CI 3.3–28.7). Eleven percent of patients with BCVI would not have met standard screening criteria.
Conclusions
The increase in detection rate for BCVI justifies more liberal screening protocols.
Similar content being viewed by others
Introduction
Blunt cerebrovascular injuries (BCVI) are uncommon but potentially devastating injuries in blunt trauma patients. The most common trauma mechanisms are stretching, direct impact, or shearing forces in areas where vessels are either fixed in place or run close to rigid or bony neighboring tissues, thus mainly affecting the internal carotid (ICA) and vertebral arteries (VA) [1, 2].
Most BCVI are initially asymptomatic and hence easily missed in clinical examination [2,3,4]. Associated traumatic brain injury (TBI) is common and may mask the signs of a vascular injury. The majority of BCVI-related ischemic cerebral infarcts occur during the first couple of days after the injury, but may develop even after weeks or months [5, 6].
Morbidity in blunt carotid injury ranges between 32 and 67% and in blunt vertebral artery injury between 14 and 24%, whereas mortality ranges between 13 and 38% and 8–18%, respectively [1, 7]. The risk of stroke depends on the grade of the injury [8] and is higher in ICA than in VA injuries [2, 9, 10]. Early treatment is shown to be safe and reduce BCVI-related neurologic sequelae. Current treatment methods include antiplatelet and anticoagulation therapy as well as endovascular treatment in patients with contraindications for thrombolysis [5, 6, 11].
Before the implementation of systematic screening protocols, overall incidence for BCVI in blunt polytrauma was reported to be at 0.1–1% [2, 12, 13], and is now believed to be at 1–2% [14, 15]. With more efficient and liberal screening, markedly higher detection rates of up to 2.7–9% in blunt polytrauma patients have been reported [3, 13, 14, 16, 17].
Digital subtraction angiography (DSA) is the reference standard for imaging due to its high resolution and the option to evaluate collaterals [2, 14]. It has, in clinical practice, been replaced by CT angiography (CTA) with at least 16-slice scanners, which is non-invasive, widely available, and cost-effective [2, 14, 17,18,19].
A wide spectrum of screening criteria for BCVI has been suggested, the most common being the modified Denver criteria consisting of clinical signs, symptoms, and trauma mechanisms that have been shown to correlate with BCVI (Table 1) [13, 20, 21]. Nevertheless, to as much as 30% of the BCVI patients, any of these clinical or radiological risk factors indicating BCVI do not apply, and it has been suggested that more liberal screening protocols are required to detect BCVI in these patients [22,23,24]. CTA screening of high-energy trauma patients can easily be included into whole-body CT (WBCT) for trauma [4, 13, 16, 25].
The purpose of this study was to assess the detection rate for BCVI based on augmented Denver criteria in high-energy blunt trauma patients presenting in a single level-one trauma center, and to evaluate the relative risk for ischemic stroke for these patients.
Materials and methods
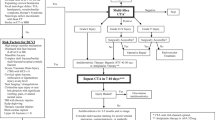
This study was conducted in a level-one trauma center with a catchment area of 1.6 million people. The study population consists of patients admitted to the emergency department after high-energy deceleration trauma such as MVA or fall from a height greater than 4 m. During this study, there were two routine trauma-WBCT protocols in use, both including an initial non-enhanced cranial CT scan. The standard WBCT protocol (sWBCT) continues with a non-enhanced CT of the cervical spine, followed by the thorax in the arterial and subsequently the abdomen in the portal venous phase. The alternative angio-protocol consists of a dual-phased WBCT (dWBCT) including a first pass from orbits to ischium in the arterial phase, and a second pass of the upper abdomen in the portal venous phase (Table 2). The latter protocol thus includes an angiogram of the carotid and vertebral arteries for the purpose of BCVI screening, while exposing the patient to an increased radiation dose. The attending trauma surgeon decided on using dWBCT protocol based on modified Denver criteria, augmented by the addition of suspected cervical spine injury on any level, and any high-energy deceleration trauma with impact on chest, abdomen, or pelvis.
All WBCT were performed on a 64-row MDCT scanner (Discovery CT750 HD, GE Medical Systems, Milwaukee, WI, USA). All WBCT for blunt trauma between October 2011 and December 2014 were reassessed retrospectively using Agfa Impax picture archiving and communications system (PACS; Impax 6.5, Agfa Gaevert, Mortsel, Belgium). All sWBCT were excluded. Two board-certified and Fellowship-trained trauma radiologists (with 12 and 8 years of experience, respectively) independently reviewed all dWBCT studies with focus on the carotid and vertebral arteries blinded to initial results. All BCVI were graded using the Biffl classification [8] (Table 3). Artery, injury level, as well as concomitant injuries were documented and are summarized in Table 4. For interobserver agreement we used kappa statistics, with kappa-values 0.01–0.20 indicating slight agreement, 0.21–0.40 fair agreement, 0.41–0.60 moderate agreement, 0.61–0.80 substantial agreement, and 0.80–0.99 almost perfect agreement [26]. Additionally, if patients were subject to any cranial CT and/or MRI studies after the initial trauma, these images were retrieved and evaluated for ischemic lesions. Analysis was performed using IBM SPSS Statistics v.23 (IBM Corp., Armonk, NY, USA). IRB approval was obtained.
Results
During 38 months, a total of 1544 WBCT studies were performed after blunt trauma, of which 374 included imaging of the craniocervical vessels in the arterial phase (m/f = 271/103; mean age 41.5 years). Most common mechanisms of injury were motor vehicle accident (MVA) (n = 192; 51.5%), fall from a height (n = 83; 22.3%), pedestrian vs. vehicle (n = 38; 10.2%), and bicycle accidents (n = 25; 6.7%). A total of 72 BCVI were identified in 56 patients (56/374; 15.0%), for an overall detection rate of 3.6% based on all trauma WBCT studies. Thirteen patients (13/56; 23.2%) had multiple BCVI. 68.1% of injuries (49/72) affected the internal carotid artery (ICA) and 31.9% (23/72) the vertebral artery (VA).
In ICA injuries, grades I and II and in VA injuries, grades II and IV were most common (ICA: G I 20/49; 40.8%; G II 15/49; 30.6%; G III 6/49; 12.2%; G IV 8/49; 16.3%; VA: G I 5/23; 21.7%; GII 8/23; 34.8%; GIII 2/23; 8.7% G IV 7/23; 30.4%; Figs. 1, 2, 3, and 4; Table 5). The most common level for BCVI was C2 in the ICA (16/49; 32.7%) and C4 in the VA (5/23; 21.7%). Figure 5 shows the number of BCVI by cervical vertebral level in both ICA and VA. Only a single grade V BCVI emerged, which was located in the basilar artery at the level of C0 (Table 6). In 3/56 (5.4%) of BCVI, there was clearly atherosclerosis present.
Interobserver agreement was overall substantial (Kappa = 0.674). In 41 of all cases, reviewers disagreed initially (11%). Differences concerned predominantly Grade I injuries (n = 25; 6.7%), thereof 13 false negative (3.5%) and 5 false positive lesions (1.3%). In grade II injuries, there was initial disagreement in 17 cases (4.5%), thereof 9 false negative (2.4%) and 4 false positive findings (1.1%). There was no interobserver disagreement for Biffl grades III through V.
Based on patients’ documented clinical findings and concomitant injuries on WBCT, 71 patients would have met the standard Denver criteria, of which 24 (34%) suffered a BCVI. BCVI was found in 32 (11%) of the 303 patients who would not have met these criteria.
Concomitant injuries affected most commonly the chest (66%), followed by head injuries (46%) and abdominal injuries (30%). Cervical spine and pelvic area were affected with 26% and 25%, respectively (Table 4).
Two hundred fifteen of the 374 patients subjected to CTA (57.4%) underwent brain imaging by either CT (n = 105; 48.8%), MRI (n = 38; 17.7%), or both CT and MRI (n = 72; 33.5%) up to 53 months after the initial trauma. The mean time from initial admission to repeat cranial imaging by MRI or CT was 147 days for people with BCVI, and 138 days for people without BCVI, with a median of 1 day for both groups. The majority of cases was imaged the following day (with BCVI n = 18; 47%, and without BCVI n = 71; 40%). Indications for imaging ranged from primary follow-up studies for the same initial trauma to newly acquired trauma, and also included imaging for unrelated conditions (Fig. 6).
Twenty one-year-old female with polytrauma after MVA; BCVI of both ICA. a Ischemic lesion and focal swelling in the area of the right caudate nucleus and lentiform nucleus, with an additional ischemic lesion in the right parietal cortex (1.5 T MRI; FLAIR). b Both lesions show decreased diffusion (arrowheads; 1.5 T MRI; DWI). c Grade IV BCVI of the right ICA (asterisk), and grade II lesion of the left ICA on the level of the skull base (arrowhead) on axial CTA images. Both VA remain open. d Wire stent of the right ICA placed under fluoroscopy guidance on DSA summation image (arrow). e 1.5 T MRA of the craniocervical arteries after stent placement demonstrating near normal patency. Signal loss caused by the metallic wire stent (arrow) in the right ICA. Residual grade II BCVI lesion of the left ICA (arrowhead)
There were cerebral ischemic lesions in 4% (n = 15) of all patients, with an incidence of n = 9 in BCVI patients (16.1%) and n = 6 in patients without BCVI (1.9%). Fisher’s exact test shows the difference in incidence between these groups to be statistically significant (p < .0001), with an odds ratio of 9.77 (95% CI 3.3–28.7). Of the 9 BCVI patients who developed an ischemic lesion, 3 (3/9; 33.3%) would have met the Denver criteria, while 6 (6/9; 66.7%) would not. Conversely, of the 6 patients with ischemic lesions and no BCVI finding, 1 (1/6; 16.7%) would have met the Denver criteria, and 5 (5/6; 83.3%) would not.
Discussion
Applying our augmented imaging criteria resulted in a markedly higher detection rate for BCVI compared to previous reports [3, 12, 13, 15, 17] while being high in the previously reported range with 3.6% when calculated based on the overall number of trauma patients, which indicates a favorable rate of selection for screening. This is in accordance with publications predicting a higher incidence of BCVI with more liberal screening [22, 27, 28].
Since the exact trauma mechanism may be difficult or even impossible to determine with certainty during the initial phase, this particular criterion might not be applicable for every patient. Correct recognition of clinical criteria on the other hand depends on the ER physician’s experience, as well as on the patient’s ability to cooperate. BCVI will often remain initially clinically silent or might be masked by concomitant injury or intoxication.
When retrospectively applying Denver screening criteria, 11% of BCVI patients in our cohort would not have been imaged, thereby resulting in these BCVI being missed with potentially disastrous consequences.
The distribution of BCVI follows the mechanical properties of the cervical spine and occipito-cervical junction. The highest incidence of BCVI in ICA was on the level of C2, where high mobility facilitates stretching and rotation, which are the major factors in the etiology of BCVI [1, 2, 29]. In the VA, BCVI is more evenly distributed, likely due to the support provided by the transverse foramina. The most common injury grades were grades I and II in the ICA and grades II and IV in the VA. The low number of grade III injuries in the VA might be due to the relatively small caliber of the transverse foramina, which might predispose for vessel occlusion rather than pseudoaneurysm formation. The singular grade V injury in our cohort does not reflect an actual low incidence, but rather the very high mortality rate associated with these injuries.
The predominant mechanisms of injury MVA, fall from a height, bicycle accident, and pedestrian in traffic represent the most common causes for ER admission due to blunt trauma, highlighting the broad spectrum of possible mechanisms leading to BCVI. Any high-energy deceleration event can potentially cause extension, flexion or rotation of the neck because of the inertia of the head, and warrants therefore inclusion into BCVI screening criteria. Blunt trauma to the chest is the second most common cause of death in polytrauma patients after CNS trauma, and may indicate that major deformation of the thoracic area has occurred during the time of impact [30], with the possibility of distortion of the neck.
The downside of including CTA in WBCT is slightly decreased image quality due to patients’ arms being raised during the scan in order to reduce imaging artifacts as well as radiation dose to the chest and abdomen, leading to increased image noise and imaging artifacts in the neck.
Interobserver agreement for BCVI was substantial with kappa = 0.674. Disagreements affected mainly grade I and II injuries, which are minimal lesions in the vessel walls and are especially hard to detect in the presence of image noise, artifacts, medical equipment, and concomitant injury. CTA as part of the initial WBCT has been shown to have a sensitivity up to 90% in more recent publications [25], with older articles claiming sensitivities of greater than 97% with a specificity of over 86% [31, 32]. Extending the contrast-enhanced scan to the skull base and neck takes only a minimal amount of additional time, especially if otherwise a non-enhanced CT of the cervical spine would have been performed. The high interobserver agreement for BCVI implies that inclusion of the cervical arteries into routine WBCT is an effective means of identifying BCVI in trauma patients.
The marked increase in ischemic CNS lesions found on cranial imaging in BCVI patients after the initial trauma compared to those without BCVI findings shows the delayed effects acute vascular injuries may have, and that these may occur even years after the initial trauma. Even though a direct correlation between the documented vascular injury and subsequent CNS ischemia cannot be established based on our data, there is a significant relative risk associated with previous BCVI. This emphasizes the importance of detecting these injuries to allow for adequate treatment.
Concomitant injury was most frequently found in the area of the chest at 66%, which emphasizes the importance of including injury to this area into the criteria for screening. Cervical spine injuries, somehow counterintuitively, were encountered by comparison considerably less frequently coinciding with BCVI at 26%. Also, head injury with 46% appears to be a more reliable indicator of BCVI than injury to the cervical spine.
When applying Denver criteria retrospectively to our data, the number to scan to find a BCVI in asymptomatic patients would be ten. Most likely, these patients would not have been imaged according to standard criteria, and their injuries would therefore almost certainly have been missed initially.
Limitations of this study include that due to it being retrospective, documentation was not completely uniform, and information like injury severity score (ISS) and Glasgow coma scale (GCS) could not be retrieved for all patients. Also, there was no DSA confirmation of either positive or negative findings, so specificity and sensitivity could not be calculated. Cranial imaging was not standardized for follow-up of the primary vascular lesions, and the etiology of ischemic lesions is impossible to trace conclusively to the primary trauma.
In conclusion, based on the high detection rate of BCVI using our modified Denver criteria, we recommend including CTA into WBCT for trauma in any high-energy deceleration trauma to the chest, abdomen, or pelvis in addition to the basic Denver criteria.
References
Sliker CW (2008) Blunt cerebrovascular injuries: imaging with multidetector CT angiography. Radiographics 28(6):1689–1708
Rutman AM, Vranic JE, Mossa-Basha M (2018) Imaging and management of blunt cerebrovascular injury. Radiographics 38(2):542–563
Burlew CC, Biffl WL, Moore EE, Barnett CC, Johnson JL, Bensard DD (2012) Blunt cerebrovascular injuries: redefining screening criteria in the era of noninvasive diagnosis. J Trauma Acute Care Surg 72(2):330–335
Bonatti M, Vezzali N, Ferro F, Manfredi R, Oberhofer N, Bonatti G (2013) Blunt cerebrovascular injury: diagnosis at whole-body MDCT for multi-trauma. Insights Imaging 4(3):347–355
Cothren CC, Moore JE, Biffl WL et al (2004) Anticoagulation is the gold standard therapy for blunt carotid injuries to reduce stroke rate. Arch Surg 139(5):540–545
Fabian TC, Patton JH Jr, Croce MA, Minard G, Kudsk KA, Pritchard FE (1996) Blunt carotid injury importance of early diagnosis and anticoagulant therapy. Ann Surg 223(5):513–525
Stein DM, Boswell S, Sliker CW, Lui FY, Scalea TM (2009) Blunt cerebrovascular injuries: does treatment always matter? J Trauma 66(1):132–143
Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Burch JM (1999) Blunt carotid arterial injuries: implications of a new grading scale. J Trauma 47(5):845–853
Miller PR, Fabian TC, Croce MA, Cagiannos C, Williams JS, Vang M, Qaisi WG, Felker RE, Timmons SD (2002) Prospective screening for blunt cerebrovascular injuries: analysis of diagnostic modalities and outcomes. Ann Surg 236(3):386–393
Fink KR, Fink JR, Cohen WA (2011) Cervical collaterals may protect against stroke after blunt vertebral artery injury. Emerg Radiol 18(6):545–549
Shahan CP, Magnotti LJ, McBeth PB et al (2016) Early antithrombotic therapy is safe and effective in patients with blunt cerebrovascular injury and solid organ injury or traumatic brain injury. J Trauma Acute Care Surg 81(1):173–177
Bromberg WJ, Collier BC, Diebel LN et al (2010) Blunt cerebrovascular injury practice management guidelines: the Eastern Association for the Surgery of Trauma. J Trauma 68(2):471–477
George E, Khandelwal A, Potter C et al (2018, 2018) Blunt traumatic vascular injuries of the head and neck in the ED. Emerg Radiol. https://doi.org/10.1007/s10140-018-1630-y
Brommeland T, Helseth E, Aarhus M et al (2018) Best practice guidelines for blunt cerebrovascular injury (BCVI). Scand J Trauma Resusc Emerg Med 26(1):90
Grigorian A, Kabutey NK, Schubl S, de Virgilio C, Joe V, Dolich M, Elfenbein D, Nahmias J (2018) Blunt cerebrovascular injury incidence, stroke-rate, and mortality with the expanded Denver criteria. Surgery 164(3):494–499
Jaevons C, Hacking C, Beenen LF, Gunn ML (2017) A review of split-bolus single pass CT in the assessment of trauma patients. Emerg Radiol 25:367–374
Biffl WL, Egglin T, Benedetto B, Gibbs F, Cioffi WG (2006) Sixteen-slice computed tomographic angiography is a reliable noninvasive screening test for clinically significant blunt cerebrovascular injuries. J Trauma 60(4):745–752
Liang T, Tso DK, Chiu RYW, Nicolaou S (2013) Imaging of blunt vascular neck injuries: a review of screening and imaging modalities. Am J Roentgenol 201(4):884–892
Roberts DJ, Chaubey VP, Zygun DA, Lorenzetti D, Faris PD, Ball CG, Kirkpatrick AW, James MT (2013) Diagnostic accuracy of computed tomographic angiography for blunt cerebrovascular injury detection in trauma patients. Ann Surg 257(4):621–632
Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Elliott JP, Burch JM (1999) Optimizing screening for blunt cerebrovascular injuries. Am J Surg 178:517–522
Biffl WL, Cothren CC, Moore EE, Kozar R, Cocanour C, Davis JW, McIntyre RC Jr, West MA, Moore FA (2009) Western Trauma Association critical decisions in trauma: screening for and treatment of blunt cerebrovascular injuries. J Trauma 67(6):1150–1153
Bruns BR, Tesoriero R, Kufera J, Sliker C, Laser A, Scalea TM, Stein DM (2014) Blunt cerebrovascular injury screening guidelines: what are we willing to miss? J Trauma Acute Care Surg 76(3):691–695
Kerwin J, Bynoe RP, Murray J et al (2001) Liberalized screening for blunt carotid and vertebral artery injuries is justified. J Trauma 51(2):308–314
Geddes AE, Burlew CC, Wagenaar AE, Biffl WL, Johnson JL, Pieracci FM, Campion EM, Moore EE (2016) Expanded screening criteria for blunt cerebrovascular injury: a bigger impact than anticipated. Am J Surg 212(6):1167–1174
Laser A, Kufera JA, Bruns BR, Sliker CW, Tesoriero RB, Scalea TM, Stein DM (2015) Initial screening test for blunt cerebrovascular injury: validity assessment of whole-body computed tomography. Surgery 158(3):627–635
Donker DK, Hasman A, Van Geijn HP (1993) Interpretation of low kappa values. Comput Int J Biomed 33:55–64
Jacobson LE, Ziemba-davis M, Herrera AJ (2015) The limitations of using risk factors to screen for blunt cerebrovascular injuries: the harder you look, the more you find. World J Emerg Surg 26(10):46
Grabkowski G, Robertson RN, Barton BM et al (2016) Blunt cerebrovascular injury in cervical spine fractures: are more liberal screening criteria warranted? Global Spine J 6:679–685
McKevitt EC, Kirkpatrick AW, Vertesi L et al (2002) Identifying patients at risk for intracranial and extracranial blunt carotid injuries. Am J Surg 183(5):566–570
Deutsche Gesellschaft für Unfallchirurgie (DGU) (2015) Trauma register DGU ® TR-DGU. Available from: http://www.traumaregister-dgu.de/fileadmin/user_upload/traumaregister-dgu.de/docs/Downloads/TR-DGU-Jahresbericht_2015.pdf
Malhotra AK, Camacho M, Ivatury RR, Davis IC, Komorowski DJ, Leung DA, Grizzard JD, Aboutanos MB, Duane TM, Cockrell C, Wolfe LG, Borchers CT, Martin NR (2007) Computed tomographic angiography for the diagnosis of blunt carotid / vertebral artery injury: a note of caution. Ann Surg 246(4):632–643
Eastman AL, Chason DP, Perez CL, McAnulty AL, Minei JP (2006) Computed tomographic angiography for the diagnosis of blunt cervical vascular injury: is it ready for primetime? J Trauma 60(5):925–929
Acknowledgements
Open access funding provided by University of Helsinki including Helsinki University Central Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Declaration of conflicting interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
OpenAccess This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Bensch, F.V., Varjonen, E.A., Pyhältö, T.T. et al. Augmenting Denver criteria yields increased BCVI detection, with screening showing markedly increased risk for subsequent ischemic stroke. Emerg Radiol 26, 365–372 (2019). https://doi.org/10.1007/s10140-019-01677-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-019-01677-0