Abstract
Fosfomycin (FOS) administered intravenously has been recently rediscovered for the treatment of systemic infections due to multidrug-resistant bacteria. Its pharmacokinetic properties suggest a time-dependent dosing schedule with more clinical benefits from prolonged (PI) or continuous infusion (CI) than from intermittent infusion. We revised literature concerning PI and CI FOS to identify the best dosing regimen based on current evidence. We performed a MEDLINE/PubMed search. Ninety-one studies and their pertinent references were screened. Seventeen studies were included in the present review. The activity of FOS against Gram-negative and Gram-positive bacteria was evaluated in fourteen and five studies, respectively. Six studies evaluated FOS activity in combination with another antibiotic. Daily dosing of 12, 16, 18 or 24 g, administered with different schedules, were investigated. These regimens resulted active against the tested isolates in most cases. Emergence of resistant isolates has been shown to be preventable through the coadministration of another active antibiotic. FOS is a promising option to treat systemic infections caused by multidrug-resistant bacteria. Coadministration with another active molecule is required to prevent the emergence of resistant bacterial strains. The results of our review suggest that a therapeutic regimen including a loading dose of FOS 8 g followed by a daily dose of 16 g or 24 g CI could be the best therapeutic approach for patients with normal renal function. The dosing regimens in patients with renal insufficiency and CI or PI superiority compared with intermittent infusion in clinical settings should be further investigated.
Similar content being viewed by others
Introduction
The worrying increase of antimicrobial resistance, both in inpatients and outpatients, prompts clinicians to find new therapeutic options. Fosfomycin (FOS), administered intravenously, has been recently re-evaluated for the treatment of systemic infections caused by multidrug-resistant (MDR) bacteria. FOS acts with a unique mechanism of action on the bacterial wall. It is active against many aerobic Gram-negative and -positive bacterial strains (Table 1) [2], and it should be administered with (at least) another active drug to prevent the emergence of resistance [3, 4].
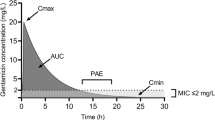
FOS is marketed both as oral (fosfomycin trometamol, fosfomycin calcium) and intravenous (fosfomycin disodium) formulation. Both time- and concentration-dependent activity have been suggested according to the bacteria evaluated, but due to its short half-life and rapid bactericidal action a time-dependent approach is more often employed [3, 5, 6]. FOS serum half-life is 4–5.7 h for oral formulation [7, 8] and approximately halved when administered intravenously [8, 9]. Although literature data on FOS volume of distribution are controversial (ranging from 40 to 136 L [6, 10]), an excellent tissue penetration is reported, including the central nervous system, soft tissues and bone tissues [6] (AUC0–4 ratio for muscle over plasma was 0.71 for patients with soft tissue infections [11]). FOS is an appealing therapeutic option also for lower respiratory tract infections, biliary tract infections and abscesses [12,13,14,15]. FOS is cleared non-metabolized by the kidney and reaches in urine concentrations higher than the minimum inhibitory concentrations (MICs) [8, 16, 17]. Urinary concentrations are higher when FOS is administered intravenously [8]. Its pharmacokinetic properties suggest a time-dependent dosing schedule, with potential clinical benefits deriving from prolonged (PI) or continuous infusion (CI) compared with intermittent infusion (II), the dosing schedule most frequently used to-date. Despite this, guidelines on the best dosing regimen for FOS are lacking. Therefore, we revised literature concerning FOS CI or PI to hypothesize the best dosing regimen based on the actual evidence.
Materials and methods
We performed a MEDLINE/PubMed search and the complete search string was as follows: “(fosfomycin[Text Word]) AND (continuous[Text Word] OR prolonged[Text Word] OR extended[Text Word]) AND (infusion[Text Word] OR intravenous[Text Word] OR pharmacodynamics[Text Word]OR pharmacokinetics[Text Word] OR “opat”[Text Word] OR outpatient[Text Word] OR elastomeric[Text Word] OR pump[Text Word])”. Ninety-one papers from inception to 4 November 2020 were identified and underwent title, abstract and full text screening. Papers written in languages other than English were excluded. Seventy-six papers were excluded for the aforementioned reasons. In addition, pertinent references of included papers and abstracts from international congresses (from 2016 to 2020) were reviewed and discussed. A total of seventeen papers were included in the present review.
Results
Seventeen papers (14 original articles, 4 of which clinical trials, 2 abstracts from international congress and 1 review) were reviewed and discussed. Preclinical and clinical studies evaluated in the present review are briefly listed in Table 2 and Table 3, respectively.
Fourteen studies investigated FOS dosing regimens in the setting of Gram-negative bacteria (2 in vivo studies, 8 simulation studies, 4 clinical trials, 1 review [4, 20,21,22,23,24,25,26,27,28,29,30,31,32]), while FOS dosing regimens against Gram-positive bacteria were evaluated in 5 studies (2 in vitro studies, 2 clinical trials, 1 review [18, 19, 27, 31, 32]). One study [33] did not evaluate the activity of FOS administered in CI since its objective was to report PK/PD parameters in healthy volunteers. Six studies [19, 20, 22,23,24, 26] evaluated FOS in combination with cefotaxime, ciprofloxacin, pefloxacin, meropenem, doripenem and polymyxin B.
With regard to CI, the daily dosing regimens in the setting of FOS monotherapy were 12 g [4, 22], 18 g [4] and 24 g [30, 33], while FOS in combination with carbapenems was evaluated at daily dose of 16 g [23], resulting active against Pseudomonas aeruginosa in two studies [23, 30] and Escherichia coli extended-spectrum beta-lactamase (ESBL)-producing, but not against carbapenem-resistant P. aeruginosa.
With regard to PI, seven different dosing regimens were evaluated. A schedule of 12 g per day (4g q8hr PI) was evaluated in two studies against non-MDR isolates, administered as monotherapy [23] or combination therapy [22]. FOS monotherapy 16 g per day, administered either as 4 g q6hr PI [28, 29] or 8 g q12hr PI [28], resulted active against non-MDR isolates in two studies. Administration of 18 g per day (6 g q8hr PI) was evaluated in a PK model simulation [25] and in the ZEUS trial [31, 32]. Finally, dosing regimens of 24 g per day, either as 4 g q4hr PI [23], 6 g q6hr PI [24, 26, 27], or 8 g q8hr PI [24, 27,28,29], resulted active also against MDR isolates.
When FOS given as monotherapy did not result to be active, this was due to the emergence of resistant strains [4, 22, 26]. FOS resistance occurred later when FOS was administered in CI compared with intermittent infusion [23, 26]. The administration of FOS with another active antibiotic was able to overcome resistance in most cases obtaining sustained bactericidal effect [23, 26].
PI resulted in 80–90% probability of target attainment (PTA) in studies simulating the efficacy of FOS against both P. aeruginosa and Enterobacterales [23,24,25, 28]. FOS administered in CI showed even better results, reaching 100% PTA against P. aeruginosa isolates in the study by Matzneller et al. [30].
Table 4 sums up the investigated dosing regimens and their effectiveness against the tested isolates.
Discussion and conclusion
This is the first systematic review evaluating FOS administered as CI or PI. Actual guidelines or expert opinions indicate slightly different dosages for the administration of FOS in CI [34, 35].
Our revision suggests that FOS 8 g loading dose followed by a daily dose of 16 g or up to 24 g CI is the best approach for patients with normal renal function. This dosage should be tailored considering the site of infection and the FOS MIC of the bacteria responsible of the infection. A critical evaluation of different dosing regimens should always be performed. For instance, evaluation of FOS penetration in abscesses reported a long half-life of the molecule (32 ± 39 h) in the pus, suggesting that FOS CI would not add any advantage compared with II in this scenario [36]. This is due to the fact that CI leads to higher AUC but reduced Cmax compared with II [30, 33].
FOS administered according to dosing regimens CI or PI is an option to keep in mind to treat systemic infections caused by MDR bacteria. Although FOS turned out to be well tolerated, thrombophlebitis and circumscribed paresthesia were reported to occur especially when the antibiotic is administered according to the CI or PI regimens [30, 33]. Administration of IV Ringer’s lactate simultaneously with FOS reduced the risk of thrombophlebitis in one study [33].
Dose adjustment according to renal function is required to keep the good safety profile of the drug, as acute or chronic kidney injury can cause a reduction in the glomerular filtration and therefore in the drug elimination [37, 38].
The emergence of resistant bacterial strains resulted in a weak activity of FOS in some series [4, 22, 26]. About this critical issue, CI delayed the development of resistance to FOS compared with II [4]. FOS has excellent synergistic properties [39] and these can lead to a long-lasting bactericidal effect [23, 26]. Furthermore, taking the advantages obtained by the synergism of FOS with other antibiotics, FOS can be considered for the combination treatment of some isolates intrinsically resistant to FOS or against which FOS has only a weak activity, i.e., P. aeruginosa or Acinetobacter spp. [23, 40,41,42,43]. Indeed, FOS represents a good option for combination therapies with antibiotics active against such bacteria.
Another advantage of PI or CI is the potential decrease of electrolyte imbalance if compared with rapid infusion [44]. In fact, the intravenous formulation contains 13.5 mEq/g of sodium; therefore, caution is needed to avoid hyopokalemia, especially in patients with heart insufficiency or who are undergoing dialysis [34].
Although few clinical studies evaluating FOS in CI or PI against Gram-positive bacteria are available to-date, this review suggests potential benefits from the use of this antibiotic in this setting [18, 19, 27, 31, 32]. This is interesting if we take into consideration the anti-biofilm properties of FOS, against both Gram-positive and Gram-negative bacterial strains [45, 46].
To the best of our knowledge, no study evaluated the efficacy of FOS prescribed as CI in outpatients through elastomeric pumps. Due to its long-term stability, intravenous FOS CI might be an option also for the outpatient parenteral antimicrobial therapy (OPAT), thus shortening hospitalization and its related risks and costs.
In summary, this systematic review suggests that FOS 8 g loading dose followed by a daily dose of 16 g or up to 24 g CI is a promising therapeutic regimen in the treatment of systemic infections including those due to MDR organisms. Future studies on FOS administered according to the CI regimen should include the evaluation of dosing regimens in patients with chronic renal failure and in haemodialysed patients. The efficacy of FOS according to the site of infection requires further investigation and expert advice should always be sought. Furthermore, as evaluation of PK/PD parameters on healthy volunteers after CI showed better results compared with II [30, 33], clinical trials comparing the superiority of CI or PI to II in different settings are desirable.
References
Sanford guide to antimicrobial therapy 2020 - pocket edition [Internet]. [cited 2020 21];https://store.sanfordguide.com/antimicrobial-therapy-2020-pocket-edition-4375-x-65-p151.aspx
Falagas ME, Kastoris AC, Kapaskelis AM, Karageorgopoulos DE (2010) Fosfomycin for the treatment of multidrug-resistant, including extended-spectrum beta-lactamase producing, Enterobacteriaceae infections: a systematic review. Lancet. Infect. Dis. 10:43–50. [cited 2019 17]. https://linkinghub.elsevier.com/retrieve/pii/S1473309909703251. https://doi.org/10.1016/S1473-3099(09)70325-1
Fransen F, Hermans K, Melchers MJB, Lagarde CCM, Meletiadis J, Mouton JW (2017) Pharmacodynamics of fosfomycin against ESBL- and/or carbapenemase-producing Enterobacteriaceae. J. Antimicrob. Chemother. 72:3374–3381. https://doi.org/10.1093/jac/dkx328
Louie A, Maynard M, Duncanson B, Nole J, Vicchiarelli M, Drusano GL (2018) Determination of the dynamically linked indices of fosfomycin for Pseudomonas aeruginosa in the hollow fiber infection model. Antimicrob. Agents Chemother. 1:62. https://doi.org/10.1128/AAC.02627-17
Roussos N, Karageorgopoulos DE, Samonis G, Falagas ME (2009) Clinical significance of the pharmacokinetic and pharmacodynamic characteristics of fosfomycin for the treatment of patients with systemic infections. Int. J. Antimicrob. Agents 34:506–515. [cited 2020 25]. https://pubmed.ncbi.nlm.nih.gov/19828298. https://doi.org/10.1016/j.ijantimicag.2009.08.013
Falagas ME, Vouloumanou EK, Samonis G, Vardakas KZ (2016) Fosfomycin. Clin. Microbiol. Rev. 29:321–347. [cited 2019 16]. http://www.ncbi.nlm.nih.gov/pubmed/26960938. https://doi.org/10.1128/CMR.00068-15
Patel SS, Balfour JA, Bryson HM (1997) Fosfomycin tromethamine. A review of its antibacterial activity, pharmacokinetic properties and therapeutic efficacy as a single-dose oral treatment for acute uncomplicated lower urinary tract infections. Drugs 53:637–656. [cited 2020 9]. https://pubmed.ncbi.nlm.nih.gov/9098664/. https://doi.org/10.2165/00003495-199753040-00007
Bergan T, Thorsteinsson SB, Albini E (1993) Pharmacokinetic profile of fosfomycin trometamol. Chemotherapy 39:297–301. [cited 2020 9]. https://pubmed.ncbi.nlm.nih.gov/8370321/. https://doi.org/10.1159/000239140
Soraci AL, Perez DS, Martinez G, Dieguez S, Tapia MO, Amanto F, et al. Disodium-fosfomycin pharmacokinetics and bioavailability in post weaning piglets. Res. Vet. Sci. [Internet] 2011 [cited 2020 9];90:498–502. https://pubmed.ncbi.nlm.nih.gov/20696447/: https://doi.org/10.1016/j.rvsc.2010.07.011
Rizek C, Ferraz JR, van der Heijden IM, Giudice M, Mostachio AK, Paez J, et al. In vitro activity of potential old and new drugs against multidrug-resistant gram-negatives. J. Infect. Chemother. [Internet] 2015 1 [cited 2020 9];21:114–7. https://pubmed.ncbi.nlm.nih.gov/25456893: https://doi.org/10.1016/j.jiac.2014.10.009
Joukhadar C, Klein N, Dittrich P, Zeitlinger M, Geppert A, Skhirtladze K, et al. Target site penetration of fosfomycin in critically ill patients. J. Antimicrob. Chemother. [Internet] 2003 1 [cited 2020 9];51:1247–52. https://pubmed.ncbi.nlm.nih.gov/12668580/: https://doi.org/10.1093/jac/dkg187
Matzi V, Lindenmann J, Porubsky C, Kugler SA, Maier A, Dittrich P, et al. Extracellular concentrations of fosfomycin in lung tissue of septic patients. J. Antimicrob. Chemother. [Internet] 2010 12 [cited 2020 9];65:995–8. https://pubmed.ncbi.nlm.nih.gov/20228081/: https://doi.org/10.1093/jac/dkq070
Lastra CF, Mariño EL, Barrueco M, Gervós MS, Gil AD. Disposition of phosphomycin in patients with pleural effusion. Antimicrob. Agents Chemother. [Internet] 1984 [cited 2020 9];25:458–62. https://pubmed.ncbi.nlm.nih.gov/6732214/doi: https://doi.org/10.1128/AAC.25.4.458
Müller O, Rückert U, Walter W, Haag R, Sauer W. Fosfomycin concentrations in serum and bile. Infection [Internet] 1982 [cited 2020 9];10:18–20. https://pubmed.ncbi.nlm.nih.gov/7068230/doi: https://doi.org/10.1007/BF01640831
Dijkmans AC, Zacarías NVO, Burggraaf J, Mouton JW, Wilms EB, van Nieuwkoop C, et al. Fosfomycin: pharmacological, clinical and future perspectives [Internet]. Antibiotics 2017 1 [cited 2020 9];6. /pmc/articles/PMC5745467/?report=abstract: https://doi.org/10.3390/antibiotics6040024
Loose M, Naber KG, Hu Y, Coates A, Wagenlehner FME. Urinary bactericidal activity of colistin and azidothymidine combinations against mcr-1-positive colistin-resistant Escherichia coli. Int. J. Antimicrob. Agents [Internet] 2019 1 [cited 2020 23];54:55–61. http://www.ncbi.nlm.nih.gov/pubmed/31034939doi: https://doi.org/10.1016/j.ijantimicag.2019.04.011
Michalopoulos AS, Livaditis IG, Gougoutas V. The revival of fosfomycin [Internet]. Int. J. Infect. Dis. 2011 [cited 2020 9];15. https://pubmed.ncbi.nlm.nih.gov/21945848/doi: https://doi.org/10.1016/j.ijid.2011.07.007
Guggenbichler JP, Berchtold D, Allerberger F, Bonatti H, Hager J, Pfaller W, et al. In vitro and in vivo effect of antibiotics on catheters colonized by staphylococci. Eur. J. Clin. Microbiol. Infect. Dis. [Internet] 1992 [cited 2020 18];11:408–15. http://link.springer.com/10.1007/BF01961855doi: https://doi.org/10.1007/BF01961855
Chavanet P, Beloeil H, Pechinot A, Duigou F, Buisson JC, Duong M et al (1995) In vivo activity and pharmacodynamics of cefotaxime or ceftriaxone in combination with fosfomycin in fibrin clots infected with highly penicillin- resistant Streptococcus pneumoniae. Antimicrob. Agents Chemother. 39:1736–1743. https://doi.org/10.1128/AAC.39.8.1736
Xiong YQ, Potel G, Caillon J, Stephant G, Jehl F, Bugnon D et al (1995) Comparative efficacies of ciprofloxacin and pefloxacin alone or in combination with fosfomycin in experimental endocarditis induced by multidrug-susceptible and -resistant Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 39:496–499. https://doi.org/10.1128/AAC.39.2.496
Bugnon D, Potel G, Xiong YQ, Caillon J, Navas D, Gras C, et al. Bactericidal effect of pefloxacin and fosfomycin against Pseudomonas aeruginosa in a rabbit endocarditis model with pharmacokinetics of pefloxacin in humans simulated in vivo. Eur. J. Clin. Microbiol. Infect. Dis. [Internet] 1997 [cited 2020 24];16:575–80. http://link.springer.com/10.1007/BF02447919doi: https://doi.org/10.1007/BF02447919
Docobo-Pérez F, Drusano GL, Johnson A, Goodwin J, Whalley S, Ramos-Martín V, et al. Pharmacodynamics of fosfomycin: insights into clinical use for antimicrobial resistance. Antimicrob. Agents Chemother. [Internet] 2015 1 [cited 2020 11];59:5602–10. https://pubmed.ncbi.nlm.nih.gov/26124169/doi: https://doi.org/10.1128/AAC.00752-15
Asuphon O, Montakantikul P, Houngsaitong J, Kiratisin P, Sonthisombat P. Optimizing intravenous fosfomycin dosing in combination with carbapenems for treatment of Pseudomonas aeruginosa infections in critically ill patients based on pharmacokinetic/pharmacodynamic (PK/PD) simulation. Int. J. Infect. Dis. 2016 1;50:23–9. https://doi.org/10.1016/j.ijid.2016.06.017
Albiero J, Sy SKB, Mazucheli J, Caparroz-Assef SM, Costa BB, Alves JLB, et al. Pharmacodynamic evaluation of the potential clinical utility of fosfomycin and meropenem in combination therapy against KPC-2-producing Klebsiella pneumoniae. Antimicrob. Agents Chemother. [Internet] 2016 1 [cited 2020 27];60:4128–39. https://pubmed.ncbi.nlm.nih.gov/27139468/doi: https://doi.org/10.1128/AAC.03099-15
Bhavnani SM, Trang M, Rubino CM, Lepak AJ, Andes DR, Flamm RK, et al. Pharmacokinetics-pharmacodynamics (PK-PD) target attainment analyses to support ZTI-01 (fosfomycin for injection) dose selection for patients with complicated urinary tract infections (cUTI).
Diep JK, Sharma R, Ellis-Grosse EJ, Abboud CS, Rao GG. Evaluation of activity and emergence of resistance of polymyxin B and ZTI-01 (fosfomycin for injection) against KPC-producing Klebsiella pneumoniae. 2018 [cited 2020 24];https://doi.org/10.1128/AAC.01815-17.doi:https://doi.org/10.1128/AAC.01815-17
Rodríguez-Gascón A, Canut-Blasco A. Deciphering pharmacokinetics and pharmacodynamics of fosfomycin [Internet]. Rev. Esp. Quimioter. 2019 1 [cited 2020 1];32:19–24. /pmc/articles/PMC6555163/?report=abstract
Leelawattanachai P, Wattanavijitkul T, Paiboonvong T, Plongla R, Chatsuwan T, Usayaporn S, et al. Evaluation of intravenous fosfomycin disodium dosing regimens in critically ill patients for treatment of carbapenem-resistant Enterobacterales infections using Monte Carlo simulation. Antibiotics [Internet] 2020 18 [cited 2020 26];9:615. https://www.mdpi.com/2079-6382/9/9/615doi: https://doi.org/10.3390/antibiotics9090615
Merino-Bohórquez V, Docobo-Pérez F, Sojo J, Morales I, Lupión C, Martín D, et al. Population pharmacokinetics and pharmacodynamics of fosfomycin in non-critically ill patients with bacteremic urinary infection caused by multidrug-resistant Escherichia coli. Clin. Microbiol. Infect. [Internet] 2018 1 [cited 2020 1];24:1177–83. https://pubmed.ncbi.nlm.nih.gov/29649596/doi: https://doi.org/10.1016/j.cmi.2018.02.005
Matzneller Peter, al Jalali Valentin, Wulkersdorfer Beatrix, Koch Birgit CP, Chou Scharon, Mouton Johan, et al. Continuous infusion of fosfomycin in healthy volunteers. 2019;
Eckburg PB, Skarinsky D, Das A, Ellis-Grosse EJ. Phenotypic antibiotic resistance in ZEUS: a multi-center, randomized, double-blind phase 2/3 study of ZTI-01 vs. piperacillin-tazobactam (P-T) in the treatment of patients with complicated urinary tract infections (cUTI) including acute pyelonephritis (AP). Open Forum Infect. Dis. [Internet] 2017 1 [cited 2020 1];4:S522–S522. https://academic.oup.com/ofid/article/4/suppl_1/S522/4295818doi: https://doi.org/10.1093/ofid/ofx163.1360
Kaye KS, Rice LB, Dane AL, Stus V, Sagan O, Fedosiuk E, et al. Fosfomycin for injection (ZTI-01) versus piperacillin-tazobactam for the treatment of complicated urinary tract infection including acute pyelonephritis: ZEUS, a phase 2/3 randomized trial. Clin. Infect. Dis. [Internet] 2019 27 [cited 2020 1];69:2045–56. https://pubmed.ncbi.nlm.nih.gov/30861061/doi: https://doi.org/10.1093/cid/ciz181
al Jalali V, Matzneller P, Wulkersdorfer B, Chou S, Bahmany S, Koch B C P, et al. Clinical pharmacokinetics of fosfomycin after continuous infusion compared with intermittent infusion: a randomized crossover study in healthy volunteers. Antimicrob. Agents Chemother. [Internet] 2020 26 [cited 2020 4];http://aac.asm.org/lookup/doi/10.1128/AAC.01375-20doi: https://doi.org/10.1128/AAC.01375-20
Mensa J, Barberán J, Soriano A, Llinares P, Marco F, Cantón R, et al. Antibiotic selection in the treatment of acute invasive infections by Pseudomonas aeruginosa: Guidelines by the Spanish society of chemotherapy. Rev. Esp. Quimioter. [Internet] 2018 1 [cited 2020 26];31:78–100. /pmc/articles/PMC6159363/?report=abstract
Candel FJ, Matesanz David M, Barberán J. New perspectives for reassessing fosfomycin: applicability in current clinical practice [Internet]. Rev. Esp. Quimioter. 2019 1 [cited 2020 14];32:1–7. /pmc/articles/PMC6555164/?report=abstract
Sauermann R, Karch R, Langenberger H, Kettenbach J, Mayer-Helm B, Petsch M, et al. Antibiotic abscess penetration: fosfomycin levels measured in pus and simulated concentration-time profiles. Antimicrob. Agents Chemother. [Internet] 2005 [cited 2020 26];49:4448–54. http://aac.asm.org/doi: https://doi.org/10.1128/AAC.49.11.4448-4454.2005
ten Doesschate T, van Haren E, Wijma RA, Koch BCP, Bonten MJM, van Werkhoven CH. The effectiveness of nitrofurantoin, fosfomycin and trimethoprim for the treatment of cystitis in relation to renal function. Clin. Microbiol. Infect. [Internet] 2020 1 [cited 2020 11];26:1355–60. https://pubmed.ncbi.nlm.nih.gov/32165321/doi: https://doi.org/10.1016/j.cmi.2020.03.001
Parker S, Lipman J, Koulenti D, Dimopoulos G, Roberts JA. What is the relevance of fosfomycin pharmacokinetics in the treatment of serious infections in critically ill patients? A systematic review [Internet]. Int. J. Antimicrob. Agents 2013 [cited 2020 11];42:289–93. https://pubmed.ncbi.nlm.nih.gov/23880170/doi: https://doi.org/10.1016/j.ijantimicag.2013.05.018
Antonello RM, Principe L, Maraolo AE, Viaggi V, Pol R, Fabbiani M, et al. Fosfomycin as partner drug for systemic infection management: a systematic review of its synergistic properties from in vitro and in vivo studies [Internet]. Antibiotics 2020 1 [cited 2020 11];9:1–74. https://pubmed.ncbi.nlm.nih.gov/32785114/doi: https://doi.org/10.3390/antibiotics9080500
Ku NS, Lee SH, Lim Y soun, Choi H, Ahn JY, Jeong SJ, et al. In vivo efficacy of combination of colistin with fosfomycin or minocycline in a mouse model of multidrug-resistant Acinetobacter baumannii pneumonia. Sci. Rep. [Internet] 2019 1 [cited 2020 12];9:17127. http://www.ncbi.nlm.nih.gov/pubmed/31748527doi: https://doi.org/10.1038/s41598-019-53714-0
Flamm RK, Rhomberg PR, Lindley JM, Sweeney K, Ellis-Grosse EJ, Shortridge D. Evaluation of the bactericidal activity of fosfomycin in combination with selected antimicrobial comparison agents tested against Gram-negative bacterial strains by using time-kill curves. Antimicrob. Agents Chemother. [Internet] 2019 1 [cited 2020 12];63. http://www.ncbi.nlm.nih.gov/pubmed/30858207doi: https://doi.org/10.1128/AAC.02549-18
Zhu W, Wang Y, Cao W, Cao S, Zhang J. In vitro evaluation of antimicrobial combinations against imipenem-resistant Acinetobacter baumannii of different MICs. J. Infect. Public Health [Internet] 2018 1 [cited 2020 12];11:856–60. http://www.ncbi.nlm.nih.gov/pubmed/30057349doi: https://doi.org/10.1016/j.jiph.2018.07.006
Cuba G, Rocha-Santos G, Cayô R, Streling A, Nodari C, Gales A, et al. In vitro synergy of ceftolozane/tazobactam in combination with fosfomycin or aztreonam against MDR Pseudomonas aeruginosa. J. Antimicrob. Chemother. [Internet] 2020 [cited 2020 20];https://pubmed.ncbi.nlm.nih.gov/32240299/doi: https://doi.org/10.1007/s40265-013-0168-2
Florent A, Chichmanian RM, Cua E, Pulcini C. Adverse events associated with intravenous fosfomycin [Internet]. Int. J. Antimicrob. Agents 2011 [cited 2020 11];37:82–3. https://pubmed.ncbi.nlm.nih.gov/21074377/doi: https://doi.org/10.1016/j.ijantimicag.2010.09.002
Yu W, Zhang J, Tong J, Zhang L, Zhan Y, Huang Y, et al. In vitro antimicrobial activity of fosfomycin, vancomycin and daptomycin alone, and in combination, against linezolid-resistant Enterococcus faecalis. Infect. Dis. Ther. [Internet] 2020 [cited 2020 14];https://pubmed.ncbi.nlm.nih.gov/32964392/doi: https://doi.org/10.1007/s40121-020-00342-1
Wang L, Di Luca M, Tkhilaishvili T, Trampuz A, Gonzalez Moreno M. Synergistic activity of fosfomycin, ciprofloxacin, and gentamicin against Escherichia coli and Pseudomonas aeruginosa biofilms. Front. Microbiol. [Internet] 2019 6 [cited 2020 12];10:2522. http://www.ncbi.nlm.nih.gov/pubmed/31781056doi: https://doi.org/10.3389/fmicb.2019.02522
Availability of data and material
As described in the Methods.
Code availability
Not applicable.
Funding
Open access funding provided by Università degli Studi di Trieste within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Conception and design: R.M.A., S.D.B., A.E.M., R.L.; Analysis and interpretation of data: R.M.A, S.D.B.; Drafting the article: R.M.A.; Revising the article for critically important intellectual content and final approval of the version to be published: S.D.B., A.E.M., R.L.
Corresponding author
Ethics declarations
Ethical approval
Not required for this kind of publication. Not applicable.
Consent to participate
As this is a systematic review of literature, consent to participate was not necessary. Not applicable.
Consent for publication
All authors agree for publication in European Journal of Clinical Microbiology and Infectious Diseases.
Conflict of interests
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Antonello, R.M., Di Bella, S., Maraolo, A.E. et al. Fosfomycin in continuous or prolonged infusion for systemic bacterial infections: a systematic review of its dosing regimen proposal from in vitro, in vivo and clinical studies. Eur J Clin Microbiol Infect Dis 40, 1117–1126 (2021). https://doi.org/10.1007/s10096-021-04181-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-021-04181-x