Abstract
The purpose of this study was the evaluation of trends in the antimicrobial resistance of Pseudomonas aeruginosa from intensive care unit (ICU) patients and urology patients in the Netherlands. From 1998 to 2010, 1,927 consecutive P. aeruginosa isolates from ICU (n = 1,393) and urology service patients (n = 534) of 14 university and referral hospitals all over the Netherlands were collected and their susceptibility to relevant antibiotics was determined according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines. Over time, a significant upward trend in the resistance of P. aeruginosa strains collected from ICUs to piperacillin (1.2 % to 10.6 %, p = 0.0175), piperacillin–tazobactam (1.2 % to 12.1 %, p = 0.0008), ceftazidime (1.2 % to 7.8 %, p = 0.0064), cefepime (4.8 % to 6.4 %, p = 0.0166), imipenem (6 % to 19.1 %, p < 0.0001), meropenem (8.3 % to 17 %, p = 0.0022) and ciprofloxacin (13.1 % to 31.2 %, p = 0.0024) was observed, as was the prevalence of multi-resistance (1.2 % to 8.5 %, p = 0.0002). For P. aeruginosa isolates from the urology services, the resistance to imipenem increased (4.1 % to 7.8 %, p = 0.0006) and to ciprofloxacin it decreased (22.4 % to 18.8 %, p = 0.025). Like in other countries, in the Netherlands, an increase in multi-resistant Gram-negatives is observed, suggesting the presence and dissemination of several mechanisms of resistance. Our findings emphasise the importance of local surveillance for the setting up of local antibiotic guidelines and to support optimal empiric therapy. With the observed increase in multi-resistance, the direct testing of alternative antibiotics like polymyxins and fosfomycin is essential. Our data also illustrate the importance of adequate outbreak control measures.
Similar content being viewed by others
Introduction
The rise in antibiotic resistance worldwide has played an important role in the establishment of different surveillance systems, such as those performed by the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC) and the European Centre for Disease Prevention and Control (ECDC) [1].
In 1998, a surveillance programme started in the Netherlands, which was later continued by the Dutch Antibiotic Resistance Surveillance Group (SWAB) [2]. One of the species included in this programme is Pseudomonas aeruginosa.
Data from the US National Nosocomial Infections Surveillance (NNIS) System showed that P. aeruginosa was the most frequent cause of ventilator-associated pneumonia and the third most important cause of urinary tract infection (UTI) in the intensive care unit (ICU) [3]. The NNIS data reported an increase in resistance to ceftazidime from 13 % to 23 % and to imipenem from 10 % to 20 % (1986–2003). At the department of urology, P. aeruginosa is the second most reported causative agent of UTI and accounts for 13 % of hospital-acquired UTIs [4].
For nosocomially acquired UTI, fluoroquinolones are the most often used antibiotics [5]. The prevalence of resistance of P. aeruginosa to fluoroquinolones reveals a great variation per country, with prevalences ranging from 0 % in Iceland, 3 % in Switzerland and Denmark to 47 % in Bosnia and Herzegovina and 55 % in Bulgaria [6].
For an optimal empiric therapy, up-to-date information of the local resistance patterns is essential. Continuous surveillance gives the possibility to reveal trends over time and to predict resistance development in the future. As no recent data on the resistance prevalence of P. aeruginosa from ICUs and urology services in the Netherlands are available, we analysed the prevalence of (oligo- or multi-)antibiotic-resistant P. aeruginosa strains from ICUs and urology services from 1998 to 2010. These data could serve as information to formulate future recommendations about the choice of empiric treatment of infections in the ICU and on the treatment of UTIs caused by P. aeruginosa.
Materials and methods
The intra-mural surveillance programme of the SWAB involved 14 hospitals, both university hospitals and large referral hospitals, geographically spread across the Netherlands [2].
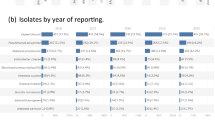
Yearly, in each hospital, the first 100 bacterial isolates of any species were collected from clinical samples of patients in ICUs and from urine samples of patients attending the urology services.
From January 1998 until January 2011, a total of 1,927 P. aeruginosa isolates were isolated: 1,393 were from ICU patients and 534 were from patients attending the urology services. Only the first P. aeruginosa isolated from a patient was included.
All isolates were identified to the species level by each laboratory’s existing protocol, stored at −20 °C in peptone glycerol (30 % w/v) and then sent to a central microbiology laboratory for quantitative antimicrobial susceptibility testing. From 1998 to 2002, the strains were tested in the Department of Medical Microbiology of the University of Nijmegen, and from 2003 until present, in the Department of Medical Microbiology of the Maastricht University Medical Center (MUMC).
Susceptibility testing
Antimicrobial susceptibilities [as minimum inhibitory concentration (MIC) values] were determined using the micro broth dilution method (http://www.eucast.org), with cation-adjusted Mueller–Hinton broth II (Becton, Dickinson and Company, Sparks, MD, USA), an inoculum of 5 × 105 cfu/mL and overnight incubation at 37 °C. The MIC plates with freeze-dried antibiotics were provided by MCS Diagnostics BV (Swalmen, the Netherlands), with a guaranteed shelf life of ∼1 year.
The antibiotics tested were (concentration range in mg/L): piperacillin (0.25–512), piperacillin–tazobactam (0.25/4–512/4), ceftazidime (0.06–128), cefepime (0.12–128), imipenem (0.06–64), meropenem (0.03–64), gentamicin (0.03–64), amikacin (0.12–256), tobramycin (0.06–128) and ciprofloxacin (0.008–16).
The MIC was defined as the lowest concentration showing no growth in the micro titre plates after 18 h of incubation at 37 °C.
Escherichia coli ATCC 35218 and ATCC 25922 were used as control strains.
For trend analysis, EUCAST breakpoints were used (piperacillin >16 mg/L, piperacillin–tazobactam >16 mg/L, ceftazidime >8 mg/L, cefepime >8 mg/L, imipenem >4 mg/L, meropenem >2 mg/L, gentamicin >4 mg/L, amikacin >8 mg/L, tobramycin >4 mg/L, ciprofloxacin >0.5 mg/L).
Multi-resistance was defined as resistance to antibiotics for three or more different classes of antibiotics (broad-spectrum penicillins; third- and fourth-generation cephalosporins; carbapenems; aminoglycosides and fluoroquinolones).
Statistical analysis
For statistical analysis, a logistic regression model was used, with the covariate ‘year’ taken to be continuous. In order to take into account the possible correlation within each year, a repeated statement was used in the GENMOD procedure to obtain the robust (or sandwich) estimates. The software used was SAS 9.2 with the GENMOD procedure.
A Chi-square test was used to compare ICU strains with strains from the urology service, and to compare the 1998–2003 urology strains with the 2004–2010 urology strains.
A p-value of <0.05 was considered to be statistically significant.
Results
Intensive care units
Resistance to all antibiotics, except aminoglycosides, increased significantly (Table 1). The resistance to imipenem increased the most significantly, from 6 % to 19.1 % (p < 0.0001). The highest prevalence of resistance was found for ciprofloxacin, which increased from 13.1 % in 1998 to 31.2 % in 2010 (p = 0.0024), obsoleting the use of ciprofloxacin for empirical therapy.
The piperacillin MIC distribution (Fig. 1a) was unimodal up to 2000, with a peak at an MIC of 2 mg/L and a smaller population with an MIC between 4 and 32 mg/L. In 2001, a small sub-population emerged with an MIC >64 mg/L. Up to 2000, the MIC distribution for gentamicin showed a unimodal curve, with MICs between 0.5 and 4 mg/L. In 2001, a small resistant sub-population with MICs above 16 mg/L appeared (Fig. 1b), which disappeared in 2007 and was observed again in 2008.
But the most remarkable finding was the increase in resistance for cefepime, as fourth-generation cephalosporins are rarely used in the Netherlands.
No upward trend in resistance was found for the combination of piperacillin, piperacillin–tazobactam or ceftazidime with an aminoglycoside (Fig. 2a). The mean resistance for the combination of piperacillin with gentamicin during the study period was 3.6 %, with amikacin 2.3 % and with tobramycin 3.1 %, and the mean resistance of ceftazidime with an aminoglycoside was less than 2 %. Cefepime showed a significant increase in resistance in combination with amikacin, from 0 % in 2000 to 3.5 % in 2010 (p = 0.0414).
a Prevalence of antibiotic resistance of P. aeruginosa from ICUs to a combination of antibiotics: piperacillin + gentamicin (pip + gen), piperacillin + ciprofloxacin (pip + cip), ceftazidime + gentamicin (caz + gen) and ceftazidime + ciprofloxacin (caz + cip). b Prevalence of antibiotic resistance of P. aeruginosa from ICUs to a combination of antibiotics: imipenem + gentamicin (imi + gen), imipenem + ciprofloxacin (imi + cip), meropenem + gentamicin (mero + gen) and meropenem + ciprofloxacin (mero + cip)
Also for the carbapenems, a combination with amikacin revealed an upward trend in resistance from 0 % in 2000 to 2.1 % (imipenem plus amikacin, p = 0.0474) and 2.8 % (meropenem plus amikacin, p = 0.0083) in 2010. The mean resistance to the combination with the other aminoglycosides was less than 2 %.
Over time, a significant increase in resistance was observed for all combinations of a beta-lactam antibiotic with ciprofloxacin, with the most significant increase in resistance for the combination with piperacillin–tazobactam (0–7.8 %, p < 0.0001) and imipenem (1.2–9.9 %, p < 0.0001) (Fig. 2b).
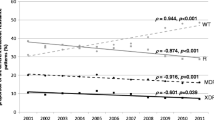
Similarly, the prevalence of multi-resistance increased from 1.2 % in 1998 to 8.5 % in 2010 (p = 0.0002) (Fig. 3).
Urology services
In contrast to the ICU isolates, no significant changes over time were observed for any of the antibiotics, except imipenem and ciprofloxacin (Table 2). The prevalence to imipenem resistance increased from 4.1 % in 1998 to 7.8 % in 2010 (p = 0.0006), and resistance to ciprofloxacin revealed a small but significant decrease over time (p = 0.025). The resistance to gentamicin was significantly higher in the first 6 years of the studied period (p = 0.010). Multi-resistance was only found sporadically, i.e. one strain each year in 2001, 2002 and 2008, and two strains in 2004 and 2010.
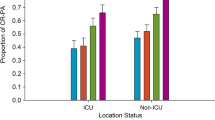
Intensive care units versus urology services
The prevalence of resistance of ICU isolates to all the tested antibiotics, except ciprofloxacin, was significantly higher than in urology strains (p < 0.05).
Discussion
P. aeruginosa is known for its ability to develop resistance to multiple classes of antibiotics, especially during prolonged treatment of an infection [8]. Often, resistance is caused by de-repression of chromosomally encoded AmpC β-lactamase, resulting in resistance to oxyimino-cephalosporins. Resistance to carbapenems is often the result of loss of the OprD porin [8, 9]. However, a worldwide increase of carbapenemase-producing P. aeruginosa strains is described, mostly metallo-β-lactamases (MBLs) [7]. The genes responsible for the production of MBLs are often located in resistance cassettes, i.e. integrons, often also harbouring other antibiotic resistance genes. Such strains have been responsible for nosocomial outbreaks in different countries [10].
Treatment options are often limited to last-resort antibiotics, such as polymyxins and fosfomycin [11, 12].
The apparent ease for P. aeruginosa to develop resistance makes continuous surveillance of resistance necessary. Therefore, we have evaluated the prevalence of resistance to relevant antibiotics among P. aeruginosa isolates from ICUs and urology services, during a 13-year period.
Among ICU strains, a significant upward trend in multi-resistance and resistance to all the tested antibiotics, except aminoglycosides, was found. Strains from urology departments revealed a significant increase in resistance to imipenem only, and a small but significant decrease in resistance to ciprofloxacin. ICU strains were significantly more resistant than urology strains, except for ciprofloxacin.
A positive aspect of the present study is the number of ICU strains, collected during a 13-year period from hospitals located all over the country. Further, the susceptibility testing was performed in a central laboratory facility; fluctuations due to differences in methodology are, thereby, eliminated.
A limitation of the study is the relatively small number of strains from urology departments, which might contribute to the large fluctuations. Other countries alike, the prevalence of resistance of P. aeruginosa from ICUs is increasing. This can be explained, at least in part, by the increase in the total consumption of antibiotics for systemic use in hospitals, from 47.2 defined daily doses (DDD)/100 patient-days in 1997 to 70.0 DDD/100 patient-days in 2009 [2, 13–15].
Although also the consumption of aminoglycosides increased, from 2.0 DDD/100 patient-days in 1997 to 4.2 DDD/100 patient-days in 2009, this had no significant influence on the prevalence of resistance. We have no clear explanation for the absence of trends.
In 2009, the majority of the carbapenem-resistant strains were isolated in a single centre: 20 out of 35 imipenem resistant strains (57.1 %), and 19 out of 28 meropenem strains (67.9 %). This is probably due to local transmission, as P. aeruginosa is known as an organism causing nosocomial outbreaks [16].
Also, the prevalence of multi-resistance was strongly influenced by strains obtained from this centre, since, in 2009, it was the origin of 17 out of 23 (74 %) of the multi-resistant isolates. Obviously, submissions from individual centres may bias the independence of the entire collection. This strong contribution to carbapenem- and multi-resistance prevalence might be caused by MBL-producing strains, which have been shown to be spreading throughout the Netherlands [17].
Also, the significant increase in resistance to a combination of cefepime with amikacin might be caused by the presence of MBL-producers [18].
Because of it’s per oral availability, ciprofloxacin is probably the most widely used antibiotic to treat UTIs caused by P. aeruginosa. Despite the increase in hospital use of ciprofloxacin, from 4.0 DDD/100 patient-days in 1997 to 9.3 DDD/100 patient-days in 2009, the prevalence of resistance in urology strains decreased. Remarkably, in the group of beta-lactam antibiotics, carbapenems had the highest resistance prevalence, although their consumption was lower than the consumption of ureidopenicillins or ceftazidime [2, 13–15]. The increased prevalence for carbapenems might also be due to the increased use of unrelated fluoroquinolones. Cross-resistance to carbapenems after the use of fluoroquinolones has been described, through the selection of mutants with up-regulated efflux of fluoroquinolones through MexEF-OprN efflux pumps, combined with the down-regulation of carbapenem-specific porin OprD [19–21].
Fluoroquinolones alike, the lower resistance prevalence for aminoglycosides in the second part of the study seems contradictory with the increase in use in hospitals. As expected, due to the higher antibiotic pressure, the overall resistance prevalence in ICU strains was much higher than in urology strains.
In conclusion, during the 13-year surveillance, we observed a significant increase in resistance for most antibiotics for ICU isolates. Urology isolates only revealed elevated resistance for ciprofloxacin.
The Netherlands, with a low methicillin-resistant Staphylococcus aureus (MRSA) prevalence, is often referred to as an example for its search-and-destroy policy. The presented increase in resistance to P. aeruginosa underscores the painful lack of such a programme for multi-resistant Gram-negative bacteria. Part of this programme should include the implementation of appropriate infection control practices [22].
Our data emphasises the importance of local surveillance for the setting up of local antibiotic guidelines and to support optimal empiric therapy, as appropriate empiric antibiotic treatment is associated with a significant reduction in all-cause mortality [23].
With the observed increase in multi-resistance, the direct testing of alternative antibiotics like polymyxins and fosfomycin in the surveillance is encouraged.
References
Kahlmeter G (2000) The ECO.SENS Project: a prospective, multinational, multicentre epidemiological survey of the prevalence and antimicrobial susceptibility of urinary tract pathogens—interim report. J Antimicrob Chemother 46(Suppl 1):15–22
SWAB, NethMap (2003) Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands. SWAB, Bilthoven
Gaynes R, Edwards JR; National Nosocomial Infections Surveillance System (2005) Overview of nosocomial infections caused by gram-negative bacilli. Clin Infect Dis 41(6):848–854
Bouza E, San Juan R, Muñoz P et al (2001) A European perspective on nosocomial urinary tract infections II. Report on incidence, clinical characteristics and outcome (ESGNI-004 study). European Study Group on Nosocomial Infection. Clin Microbiol Infect 7(10):532–542
Johansen TE, Cek M, Naber KG et al (2006) Hospital acquired urinary tract infections in urology departments: pathogens, susceptibility and use of antibiotics. Data from the PEP and PEAP-studies. Int J Antimicrob Agents 28(Suppl 1):S91–S107
European Antimicrobial Resistance Surveillance Network (EARS-Net). EARSS Annual reports. Home page at: http://www.rivm.nl/earss/
Miriagou V, Cornaglia G, Edelstein M et al (2010) Acquired carbapenemases in Gram-negative bacterial pathogens: detection and surveillance issues. Clin Microbiol Infect 16(2):112–122
Lister PD, Wolter DJ, Hanson ND (2009) Antibacterial-resistant Pseudomonas aeruginosa: clinical impact and complex regulation of chromosomally encoded resistance mechanisms. Clin Microbiol Rev 22(4):582–610
Livermore DM (1992) Interplay of impermeability and chromosomal beta-lactamase activity in imipenem-resistant Pseudomonas aeruginosa. Antimicrob Agents Chemother 36(9):2046–2048
Pitout JD, Chow BL, Gregson DB et al (2007) Molecular epidemiology of metallo-β-lactamase-producing Pseudomonas aeruginosa in the Calgary Health Region: emergence of VIM-2-producing Isolates. J Clin Microbiol 45(2):294–298
Jacquier H, Le Monnier A, Carbonnelle E et al (2012) In vitro antimicrobial activity of “last-resort” antibiotics against unusual nonfermenting gram-negative bacilli clinical isolates. Microb Drug Resist 18(4):396–401
Dinh A, Salomon J, Bru JP et al (2012) Fosfomycin: efficacy against infections caused by multidrug-resistant bacteria. Scand J Infect Dis 44(3):182–189
SWAB, NethMap (2005) Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands. SWAB, Bilthoven
SWAB, NethMap (2010) Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands. SWAB, Bilthoven
SWAB, NethMap (2011) Consumption of antimicrobial agents and antimicrobial resistance among medically important bacteria in the Netherlands. SWAB, Bilthoven
Yakupogullari Y, Otlu B, Dogukan M et al (2008) Investigation of a nosocomial outbreak by alginate-producing pan-antibiotic-resistant Pseudomonas aeruginosa. Am J Infect Control 36(10):e13–e18
Van der Bij AK, Van der Zwan D, Peirano G et al (2012) Metallo-β-lactamase-producing Pseudomonas aeruginosa in the Netherlands: the nationwide emergence of a single sequence type. Clin Microbiol Infect 18(9):E369–E372
Quinteira S, Sousa JC, Peixe L (2005) Characterization of In100, a new integron carrying a metallo-β-lactamase and a carbenicillinase, from Pseudomonas aeruginosa. Antimicrob Agents Chemother 49(1):451–453
Fukuda H, Hosaka M, Hirai K et al (1990) New norfloxacin resistance gene in Pseudomonas aeruginosa PAO. Antimicrob Agents Chemother 34(9):1757–1761
Aubert G, Pozzetto B, Dorche G (1992) Emergence of quinolone–imipenem cross-resistance in Pseudomonas aeruginosa after fluoroquinolone therapy. J Antimicrob Chemother 29(3):307–312
Livermore DM (2002) Multiple mechanisms of antimicrobial resistance in Pseudomonas aeruginosa: our worst nightmare? Clin Infect Dis 34:634–640
Deplano A, Denis O, Poirel L et al (2005) Molecular characterization of an epidemic clone of panantibiotic-resistant Pseudomonas aeruginosa. J Clin Microbiol 43(3):1198–1204
Paul M, Shani V, Muchtar E et al (2010) Systematic review and meta-analysis of the efficacy of appropriate empiric antibiotic therapy for sepsis. Antimicrob Agents Chemother 54(11):4851–4863
Acknowledgements
The authors would like to thank Mrs. Yvonne Beeuwkes for her assistance in the setting up and maintenance of the database. The participating centres and the Susceptibility Surveillance Study Group include (geographically from north to south): Medical Centre Leeuwarden, Martini Hospital Groningen, Isala Clinics Zwolle, Kennemer Gasthuis Haarlem, Onze Lieve Vrouwe Gasthuis Amsterdam, Medical Spectrum Twente Enschede, Bronovo Hospital Den Haag, St. Antonius Hospital Nieuwegein, Maasstad Hospital, Rotterdam, University Medical Centre St. Radboud Nijmegen, St. Elisabeth Hospital Tilburg, regional laboratory Zeeland Goes, VieCuri Medical Centre for North-Limburg Venlo and Maastricht University Medical Center.
Funding
This study was financially supported by the Dutch Working Party on Antibiotic Policy (SWAB).
Transparency declarations
None to declare.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Croughs, P.D., Li, B., Hoogkamp-Korstanje, J.A.A. et al. Thirteen years of antibiotic susceptibility surveillance of Pseudomonas aeruginosa from intensive care units and urology services in the Netherlands. Eur J Clin Microbiol Infect Dis 32, 283–288 (2013). https://doi.org/10.1007/s10096-012-1741-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1741-4