Abstract
Purpose
Long delays in waiting lists have a negative impact on the principles of equity and providing timely access to care. This study aimed to assess waiting lists for abdominal wall hernia repair (incisional ventral vs. inguinal hernia) to define explicit prioritization criteria.
Methods
A cross-sectional single-center study was designed. Patients in the waiting list for incisional/ventral hernia (n = 42) and inguinal hernia (n = 50) repair were interviewed by phone and completed health-related quality of life (HRQoL) questionnaires (EQ-5D, COMI-hernia, HerQLes) as a measure of severity. Priority was measured as hernia complexity, patient frailty using the modified frailty index (mFI-11), and the consumption of analgesics for hernia.
Results
The mean (SD) time on the waiting list was 5.5 (3.2) months (range 1–14). Complex hernia was present in 34.8% of the patients. HRQoL was moderately poor in patients with incisional/ventral hernia (mean HerQL score 66.1), whereas it was moderately good in patients with inguinal hernia (mean COMI-hernia score 3.40). The use of analgesics was higher in patients with incisional/ventral hernia as compared with those with inguinal hernia (1.48 [0.54] vs. 1.31 [0.51], P = 0.021). Worst values of mFI were associated with inguinal hernia as compared with incisional/ventral hernia (0.21 [0.14] vs. 0.12 [0.11]; P = 0.010).
Conclusion
Explicit criteria for prioritization in the waiting lists may be the consumption of analgesics for patients with incisional/ventral hernia and frailty for patients with inguinal hernia. A reasonable approach seems to establish separate waiting lists for incisional/ventral hernia and inguinal hernia repair.
Similar content being viewed by others
Introduction
A number of public health care systems with universal health coverage use waiting lists as a rationing capacity to balance demand and access to services more equitable [1]. Long delays, however, can have widespread negative consequences and threaten the principles of equity and providing timely access to care. In publicly funded health systems, waiting lists include the provision of a wide range of services, such as medical consultations, specialized care, diagnostic studies, or therapeutic procedures [2].
Waiting times and lists for surgeries can be divided into essential and non-essential surgical procedures. Management of non-essential operations, such as abdominal wall hernia repair, face problems, and effective processes for triaging patients remain controversial [3, 4]. From a patients’ needs perspective, three important aspects should be considered such as: (1) severity as the level of impairment of health-related quality of life, (2) priority/urgent surgery according to the individual clinical characteristics and associated comorbid conditions, and (3) the waiting time as the delay assigned to the intervention based on severity/priority of the condition of each patient [5].
Currently, the management of abdominal wall surgery waiting lists in our environment is carried out according to the length of time on the list and the priority in days (preferential 90 days, medium 180 days, and low 365 days) according to criteria related to the patient’s clinical features and social conditions, risks associated with delayed surgery, and clinical effectiveness [6]. These priority criteria are usually established by specialists from the patient’s reference hospital in which surgery will be performed according to decisions and implicit evaluations performed by each surgeon. However, implicit decisions made by individual surgeons may be overly relying on interpersonal criteria that are by definition variable and may be influenced by chance. In this context, the use of explicit criteria for managing waiting lists for abdominal wall surgery seems to play a key role for prioritizing patients based on individual needs as well as to better allocation of resources in universal health care public systems in which resources are limited.
The objective of this study was to analyze waiting lists for abdominal wall hernia repair (incisional/ventral hernia vs. inguinal hernia) to identify explicit prioritization criteria by means of assessing the relationship between severity (time on the waiting list and quality of life) and priority (type of hernia and frailty of the patient).
Methods
Design and participants
This was a single-center cross-sectional study carried out at the Abdominal Wall Surgery Unit of Hospital Universitari Vall d’Hebron in Barcelona, Spain. Our institution is an acute-care 1146-bed university-affiliated hospital in the city of Barcelona, serving an urban population of approximately 400,000 people. The Abdominal Wall Surgery Unit is a reference unit for the surgical treatment of hernia patients either already assigned to the hospital or from elsewhere who due to technical complexity or comorbidities are not candidates for outpatient surgery or elective surgery with hospital admission in other health care centers of the region. The study was conducted over a 3-week period in May 2020 when the practice of non-essential surgeries was postponed in response to the COVID-19 pandemic.
All adult patients aged 18 years or older diagnosed with an abdominal wall incisional/ventral or inguinal hernia scheduled for surgery and included in the waiting list for elective hernia repair were eligible for a telephone interview. The contact and interview with the patient was carried out via a telephone call using the telephone numbers registered in the patients’ computerized medical records. The telephone call was made by surgeons who were staff members of the Abdominal Wall Surgery Unit. There were no limits for attempts, so that the necessary calls were made until contacting the patient. Verbal informed consent was obtained from all participants prior to the interview after they had been fully informed about the purpose of the study and agreed to take part. Participation in the study was voluntary and unpaid. Patient information was used in accordance with the Spanish Organic Law 15/1999 of December 13 on Protection of Personal Data that guaranteed and protected the processing of personal data.
Study procedures and data collection
Data collection for each patient included demographics (age, sex), anthropometric data (weight, height), and scores of the study questionnaires. The time in the waiting list was assessed in months and calculated from the date of inclusion in the waiting list to the date of the interview. Standard self-completion instruments for patient-centered outcome research [7] especially those with the fewest number of questions to reduce the time and burden for patients and interviewers, were selected. Severity was measured as the impact of the disease on health-related quality of life (HRQoL) using the EuroQol-5D (EQ-5D), the Core Outcome Measures Index adapted for patients with hernia (COMI-hernia) and the Hernia-Related Quality-of-Life Survey (HerQLes). Priority was measured as hernia complexity, patient frailty using the modified frailty index (mFI-11) and the consumption of analgesics for hernia-associated symptoms.
Briefly, a Spanish validated version of the EQ-5D [8] that can be administered either face-to-face or by telephone with minimal differences [9] was used. The EQ-5D describes an individual’s health status across five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, with five levels of severity (no, slight, moderate, severe and extreme problems) and comprises a visual analogue scale (VAS) numbered from 0 (the worst health you can imagine) to 100 (the best health you can imagine) and a preference-based index where 1 is the value of full health and 0 is a heath state equivalent to death. In patients with inguinal hernia, the COMI-hernia instrument [10] was used. It consists of 6 questions, the first question “How would you rate your groin pain on the last week?” is scored from 0 (no pain) to 100 (highest pain) and the remaining 5 questions are measured using a 5-point Likert scale, where higher scores are associated with greater impairment of HRQoL. The overall score ranges from 0 to 10 [10]. However, to facilitate the clinical applicability of COMI-hernia, four categories of HRQoL were defined: good (< 2.5), moderately good (2.5–5), moderately poor (5–7.5) and poor (> 7.5). In patients with incisional/ventral hernia, the HerQLes questionnaire [11] was administered. It is a 12-item instrument in which each item related to different aspects of quality of life is scored using a 6-point Liker scale, from “strongly disagree” to “strongly agree” with higher scores indicating worse quality of life. To generate a single summary measure, scores of the 12 items were escalated and averaged, with 100 as the worst possible score and 0 as the best possible score using the following formula:
where “i” is each one of the 12 questions. Also, four categories of HRQoL were defined: good (< 25), moderately good (25–50), moderately poor (50–75) and poor (> 75).
Criteria for definition of a complex abdominal hernia were those described by Slater et al. [12] but using only age and body mass index (BMI) as risk factors, and classified into simple, moderate and complex. Frailty was assessed with mFI of the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) [13, 14]. It consists of 11 variables associated with functional status, with the presence of each variable scored as 1 point (score ranges 0–11, with a score 0 representing absence of frailty and score 11 highest degree of frailty). The following multilevel categories were defined to facilitate the clinical applicability: low mFI (score ≤ 0.18 equal to 0–1 frailty variables), intermediate mFI (score 0.18–0.35 equal to 2–3 frailty variables) and high mFI (score ≥ 0.36 equal to ≥ 4 frailty variables). The use of analgesic medication for hernia was stratified into 1 (low), 2 (moderate) and 3 (high) according to the patient’s response to the question “Which is your level of consumption of analgesic medication to improve any symptom related to your hernia?”.
Statistical analysis
For the purpose of analysis, the length of time in the waiting list was divided into three periods of equal or less than 3 months, between 4 and 6 months, and more than 6 months to 12 months. A comparison of the distribution of variables between patients with incisional/ventral hernia and inguinal hernia was made. Categorical variables are expressed as frequencies and percentages, and continuous variables as mean and standard deviation (SD). The Chi-square test or the Fisher’s exact test was used for the comparison of categorical variables, and the Kruskal–Wallis test or the Mann–Whitney U test for the comparison of quantitative variables according to conditions of application. Statistical significance was set at P < 0.05. The Statistical Package for the Social Sciences (SPSS) version 23.0 (IBM Statistics, Chicago, IL, USA) was used for the analysis of data.
Results
During the study period, a total of 111 patients scheduled for incisional/ventral and inguinal hernia repair were found in the waiting list of our unit, but 19 patients (17.1%) (incisional/ventral hernia, n = 8; inguinal hernia, n = 11) could not be reached after various telephone call attempts. Therefore, the study population included 92 patients (78.3% men) with a mean (SD) age of 66 (13.3) years and mean body mass index (BMI) of 26.2 (3.2) kg/m2. A total of 42 patients were diagnosed with incisional/ventral hernia and the remaining 50 patients with inguinal hernia. The mean time on the waiting list was 5.5 (3.2) months (range 1–14) and globally it was higher for incisional/ventral hernia (6.1 months, P = 0.011). Scores of the EQ-5D questionnaire showed a mild impairment of HRQoL, with a mean EQ-5D VAS of 71.8 and preference-based index of 0.72 without differences between groups. In patients with inguinal hernia, HRQoL was moderately good, with a mean COMI-hernia score of 3.40, whereas in those with incisional/ventral hernia was moderately poor, with a mean HerQLes score of 66.1. Complex hernia was present in 34.8% of the patients, most of them associated with incisional/ventral hernia (P = 0.000). The global mFI score was low (mean 0.17), however, the worst values were significantly associated with inguinal hernia as compared with incisional/ventral hernia (0.21 [0.14] vs. 0.12 [0.11]; P = 0.010). The use of analgesics was also low (mean 1.34) with a meaningful increase in favor of incisional/ventral hernia as compared with inguinal hernia (1.48 [0.54] vs. 1.31 [0.51], P = 0.021). The mean BMI was significantly higher in patients with incisional/ventral hernia than in those with inguinal hernia (27.1 [2.8] vs. 25.4 [3.3] kg/m2; P = 0.003), whereas the group of inguinal hernia showed a higher percentage of men (90% vs. 64.3%; P = 0.003). Salient characteristics of the patients and comparison between the two groups are shown in Table 1.
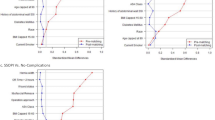
In the analysis of time on the waiting list for all 92 patients and divided by periods of ≤ 3 months, 4–6 months and > 6 to 12 months, significantly shorter times were found in older patients (P = 0.009) and in those with higher frailty (P = 0.039), whereas the duration was longer in patients with the lowest use of analgesics (P = 0.001) (Table 2). In patients with incisional/ventral hernia (Table 3), there were differences according to sex and consumption of analgesics, with a significantly higher percentage of men (75%) (P = 0.039) and lowest use of analgesics (P = 0.001) on waiting lists of 6 to 12 months. There was a trend for a shorter waiting list in patients with higher HerQLes scores but the difference was not significant (P = 0.094). In patients with inguinal hernia (Table 4), those with lower scores of EQ-5D VAS and those with higher frailty were found more frequently in the shortest length of the waiting list (P = 0.025 and P = 0.023, respectively).
Discussion
Based on results of the present study and from an overall perspective, patients with the shortest time on the waiting list were older and with higher frailty. Patients with the lowest consumption of analgesics were on the longest duration of the waiting list. Interestingly, waiting lists were different for patients with incisional/ventral hernia from those with inguinal hernia. In the group of incisional/ventral hernia, 83% of patients had moderate or complex hernias, moderately poor or poor HRQoL according to scores of the specific HerQLes questionnaire despite none or only one frailty variables, and those who consumed fewer analgesics for hernia remained in the waiting list for more time. In the group of inguinal hernia, the complexity of hernia was simple or moderate in 90% of patients, moderately good HRQoL based on scores of the specific COMI-hernia questionnaire and presented two or three frailty variables.
Differences in the waiting lists according to the type of abdominal wall hernia is an important consideration when lists are managed based only on the time on the waiting list combined with decisions of severity and prioritization according to implicit criteria of the individual surgeon. An approach from explicit criteria contributing to assess severity and prioritization objectively seems necessary to prevent as much as possible the influence of “chance” on the waiting lists.
Although the assessment of severity using HRQoL questionnaires is useful, generic instruments such as the EQ-5D show a lower sensitivity and discriminating capacity as compared to disease-specific questionnaires [15]. In this study, the combination of EQ-5D and specific questionnaires was particularly useful in the group of patients with incisional/ventral hernia in which HRQoL was scored as good or moderately good with the EQ-5D in contrast to poor or moderately poor with the specific HerQLes instrument. On the other hand, the assessment of prioritization based on the complexity of hernia, patients’ characteristics and comorbidities, and the need of analgesic medication to relief hernia-related pain was also useful. In this respect, measurement of frailty with instruments that indistinctly applicable to different surgical specialties, such as mFI index [13] rather than a simple analysis of age or number of comorbidities would be probably more convenient. The use of analgesics has also been found a useful variable in the prioritization of waiting lists in elective surgical procedures other than abdominal wall hernia repair [16]. From our point of view, the most appropriate values/scores to take into account in each group to reach an explicit prioritization criteria were the high analgesic consume in the case of incisional/ventral hernia and the higher mFI index in the case of inguinal hernia.
Although studies to investigate preoperative and perioperative characteristics among patients with an incisional hernia initially managed non-operatively who experienced acute incarceration have recently been published [17, 18], the present results are difficult to compare with data reported in the literature because a few studies focused on development of prioritization criteria have been previously published and none of them in the field of abdominal wall surgery. The Obesity Surgery Score (OSS) based on the BMI, obesity-related comorbidities and functional limitations has been proposed as a structure prioritization system in bariatric surgery [19]. A dynamic score and a vulnerability level based on a review of 20 biopsychosocial criteria have been developed for prioritization of patients in surgical waiting lists [20]. In patients on waiting lists for hip and knee replacement surgery, a priority criteria tool as a measure of surgeon-related urgency included a combination of VAS urgency, a maximum acceptable waiting time, the Western Ontario McMaster Osteoarthritis Index (WOMAC) and the ED-5D [21, 22]. In patients scheduled for cataract surgery, building of a discrete-event simulation model in the setting of the Spanish Health Care System reproducing the process of cataract, from incidence of need of surgery through demand, inclusion on a waiting list, and surgery, revealed that it was possible to shorten the waiting time by 1.55 months compared with the routinely used first-in, first-out (FIFO) system [23]. Moreover, the application of this prioritization system reduced the geographic variations thus improving equity [24].
Limitations of the study include the observational nature and the reduced number of patients included in the waiting list, as well as the fact that other variables have not been considered in the assessment of severity and prioritization of the patients. Other variables that may be relevant in the management of waiting lists may include social, economic and cultural levels, or geographical accessibility to the healthcare center. Prospective evaluation of a larger patient cohort with patient-based questionnaires would contribute to provide more conclusive findings. However, we expect that the present study may contribute to the assessment of patients from general waiting lists where multiple processes are combined (also including abdominal wall surgery), with thousands of cases examined using artificial intelligence techniques, which would allow a more precise evaluation of severity and prioritization [25, 26].
In conclusion, in patients with incisional/ventral hernia, HRQoL appears to be worse than in patients with inguinal hernia, although hernia complexity or frailty does not seem to be determinant factors for the duration of stay in the waiting list. Explicit criteria for prioritization in the waiting list appear to be the consumption of analgesics for patients with incisional/ventral hernia and frailty for patients with inguinal hernia. A reasonable approach seems to establish separate waiting lists for patients scheduled for incisional/ventral hernia repair and for those scheduled for inguinal hernia repair.
References
Curtis AJ, Russell CO, Stoelwinder JU, McNeil JJ (2010) Waiting lists and elective surgery: ordering the queue. Med J Aust 192:217–220
Chafe R, Coyte P, Sears NA (2010) Improving the management of waiting lists for long term care. Healthc Manag Forum 23:58–62. https://doi.org/10.1016/j.hcmf.2010.04.002
López Cano M, Saludes Serra J, Rosselló-Jiménez D, Pereira JA, Rodrigues Gonçalves V, García Alamino JM (2020) Abdominal wall surgery after SARS-CoV-2: time to reestablish postponed non-essential procedures? Cir Esp. https://doi.org/10.1016/j.ciresp.2020.04.011
Sutherland JM, Liu G, Crump RT, Karimuddin AA (2017) Waiting for surgery: is waiting bad for anyone or everyone? Hernia 21:933–940. https://doi.org/10.1007/s10029-017-1684-x
Peiró S (2000) Algunos elementos para el análisis de las listas de espera. Gest Clin Sanit 2:126–131
Llistes d’espera. CatSalut. Servei Català de la Salut. https://catsalut.gencat.cat/ca/coneix-catsalut/acces-sistema-salut/llistesespera/intervencions-quirurgiques/informacio/ Accessed 6 June 2020
Reeve BB, Wyrwich KW, Wu AW, Velikova G, Terwee CB, Snyder CF et al (2013) ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Qual Life Res 22:1889–1905. https://doi.org/10.1007/s11136-012-0344-y
Badia X, Roset M, Montserrat S, Herdman M, Segura A (1999) The Spanish version of EuroQol: a description and its applications. European Quality of Life scale. Med Clin (Barc) 112(Suppl 1):79–85
Wu AW, Jacobson DL, Berzon RA, Revicki DA, van der Horst C, Fichtenbaum CJ, Saag MS, Lynn L, Hardy D, Feinberg J (1997) The effect of mode of administration on medical outcomes study health ratings and EuroQol scores in AIDS. Qual Life Res 6:3–10. https://doi.org/10.1023/a:1026471020698
Staerkle RF, Villiger P (2011) Simple questionnaire for assessing core outcomes in inguinal hernia repair. Br J Surg 98:148–155. https://doi.org/10.1002/bjs.7236
Krpata DM, Schmotzer BJ, Flocke S, Jin J, Blatnik JA, Ermlich B, Novitsky YW, Rosen MJ (2012) Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215:635–642. https://doi.org/10.1016/j.jamcollsurg.2012.06.412
Slater NJ, Montgomery A, Berrevoet F, Carbonell AM, Chang A, Franklin M et al (2014) Criteria for definition of a complex abdominal wall hernia. Hernia 18:7–17. https://doi.org/10.1007/s10029-013-1168-6
Seib CD, Rochefort H, Chomsky-Higgins K, Gosnell JE, Suh I, Shen WT, Duh QY, Finlayson E (2018) Association of patient frailty with increased morbidity after common ambulatory general surgery operations. JAMA Surg 153:160–168. https://doi.org/10.1001/jamasurg.2017.4007
Velanovich V, Antoine H, Swartz A, Peters D, Rubinfeld I (2013) Accumulating deficits model of frailty and postoperative mortality and morbidity: its application to a national database. J Surg Res 183:104–110. https://doi.org/10.1016/j.jss.2013.01.021
EuroQol group (1990) EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 16(3):199–208. https://doi.org/10.1016/0168-8510(90)90421-9
Adam P, Alomar S, Espallargues M, Herdman M, Sanz L, Solà-Morales O et al (2010) Priorización entre procedimientos quirúrgicos electivos con lista de espera del sistema sanitario público en Catalunya. Agencia de Información, Evaluación y Calidad en Salud. Servicio Catalán de la Salud. Departamento de Salud. Generalitat de Catalunya, Barcelona
Huckaby LV, Dadashzadeh ER, Handzel R, Kacin A, Rosengart MR, van der Windt DJ (2020) Improved understanding of acute incisional hernia incarceration: implications for addressing the excess mortality of emergent repair. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2020.08.735
Dadashzadeh ER, Huckaby LV, Handzel R, Hossain MS, Sanin GD, Anto VP, Bou-Samra P, Moses JB, Cai S, Phelos HM, Simmons RL, Rosengart MR, van der Windt DJ (2020) The risk of incarceration during nonoperative management of incisional hernias: a population-based analysis of 30,998 patients. Ann Surg. https://doi.org/10.1097/SLA.0000000000003916
Casimiro Pérez JA, Fernández Quesada C, Del Val Groba Marco M, Arteaga González I, Cruz Benavides F, Ponce J, de Pablos Velasco P, Marchena Gómez J (2018) Obesity Surgery Score (OSS) for prioritization in the bariatric surgery waiting list: a need of public health systems and a literature review. Obes Surg 28:1175–1184. https://doi.org/10.1007/s11695-017-3107-6
Silva-Aravena F, Álvarez-Miranda E, Astudillo CA, González-Martínez L, Ledezma JG (2020) On the data to know the prioritization and vulnerability of patients on surgical waiting lists. Data Brief 29:105310. https://doi.org/10.1016/j.dib.2020.105310
Conner-Spady B, Estey A, Arnett G, Ness K, McGurran J, Bear R, Noseworthy T, Steering Committee of the Western Canada Waiting List Project (2004) Prioritization of patients on waiting lists for hip and knee replacement: validation of a priority criteria tool. Int J Technol Assess Health Care 20:509–515. https://doi.org/10.1017/s0266462304001436
Conner-Spady BL, Arnett G, McGurran JJ, Noseworthy TW, Steering Committee of the Western Canada Waiting List Project (2004) Prioritization of patients on scheduled waiting lists: validation of a scoring system for hip and knee arthroplasty. Can J Surg 47:39–46
Comas M, Castells X, Hoffmeister L, Román R, Cots F, Mar J, Gutierrez-Moreno S, Espallargues M (2008) Discrete-event simulation applied to analysis of waiting lists. Evaluation of a prioritization system for cataract surgery. Value Health 11:1203–1213. https://doi.org/10.1111/j.1524-4733.2008.00322.x
Román R, Comas M, Mar J, Bernal E, Jiménez-Puente A, Gutiérrez-Moreno S, Castells X, IRYSS Network Modelling Group (2008) Geographical variations in the benefit of applying a prioritization system for cataract surgery in different regions of Spain. BMC Health Serv Res 8:32. https://doi.org/10.1186/1472-6963-8-32
Klute B, Homb A, Chen W, Stelpflug A (2019) Predicting outpatient appointment demand using machine learning and traditional methods. J Med Syst 43:288. https://doi.org/10.1007/s10916-019-1418-y
Curtis C, Liu C, Bollerman TJ, Pianykh OS (2018) Machine learning for predicting patient wait times and appointment delays. J Am Coll Radiol 15:1310–1316. https://doi.org/10.1016/j.jacr.2017.08.021
Acknowledgements
We thank Marta Pulido, MD, PhD, for editing the manuscript and editorial assistance.
Funding
No direct or indirect financial support by extramural sources was received.
Author information
Authors and Affiliations
Contributions
ML-C and VRG contributed to the conception of the study, wrote the paper and were responsible for editorial decisions including the selection of the journal. ML-C, VRG, CP, DRJ, JSS and MAC extracted the data, analyze data, interpreted the results, and prepared the final draft. JMGA advised for methodology, analysis and interpretation of results and reviewed the article.
Corresponding author
Ethics declarations
Conflict of interest
M. López-Cano has received honoraria for consultancy, lectures, support for travels and participation in review activities from BD-Bard, Medtronic and Gore. V. Rodrigues Gonçalves, M. Verdaguer Tremolosa, C. Petrola Chacón, D. Rosselló Jiménez, J. Saludes Serra, M. Armengol Carrasco and Josep M. García Alamino have no conflicts of interest or financial ties to disclose.
Ethical approval
Ethical approval was not required as this was a retrospective study based on data collected prospectively in a database of the Surgery Department.
Human and animal rights
This article does not contain any study with animals performed by any of the authors.
Informed consent
Verbal informed consent was obtained from all participants prior to the interview after they had been fully informed about the purpose of the study and agreed to take part.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
López-Cano, M., Rodrigues-Gonçalves, V., Verdaguer-Tremolosa, M. et al. Prioritization criteria of patients on scheduled waiting lists for abdominal wall hernia surgery: a cross-sectional study. Hernia 25, 1659–1666 (2021). https://doi.org/10.1007/s10029-021-02378-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-021-02378-9