Abstract
Background
Patient-reported outcomes (PROs) such as quality of life (QoL), patient satisfaction, and work impairment, are arguably the most important outcomes of any medical treatment. In 2011, Staerkle and Villiger developed the Core Outcome Measurements Index (COMI) to standardise PROs and PRO measurement for inguinal hernia patients, in an attempt to increase inter-study comparability. The aim of this study is to prospectively evaluate the short- and long-term postoperative QoL, function, patient well-being, pain, and social/work disability, after total extraperitoneal (TEP) inguinal hernia repair and to provide the first clinical experience with the COMI-hernia questionnaire.
Methods
Between January 2013 and December 2014, all patients ≥18 years that were scheduled for elective uni- or bilateral TEP in a regional hospital were approached to participate in this study. Measurements were taken preoperatively, and 6 weeks and 1 year postoperatively.
Results
One hundred and twenty patients (113 men, 7 women), mean age 59 years (SD ±12), completed the follow-up of 1 year. Ninety-seven percent of the population reported that the operation improved their complaints. QoL, function, well-being, and pain all improved after 6 weeks and 1 year after surgery. Patients experienced more social and work-related limitations 6 weeks after surgery compared to baseline measurements, though this improved to normal 1 year postoperatively. The incidence of chronic pain was 14% (VAS ≥ 2), which had a negative impact on the patients' sense of well-being.
Conclusion
Patients recovered well after TEP repair with a good quality of life and fast restore of function. Patient well-being was lower than expected due to a 14% incidence of chronic pain. The COMI-hernia scale provided reasonable insight into the patients' experience, though it was difficult to interpret for both patient and physician.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inguinal hernia repair is one of the most frequently performed operations [1]. In the Netherlands alone, as much as 30.000 elective procedures are performed each year [2]. Ever since the recurrence rates after inguinal hernia repair have dropped below 5%, the focus of scientific research has slowly shifted away from recurrence rates, surgical techniques, and postoperative complications towards ‘patient-reported outcomes’ (PROs). PROs are defined by the Food and Drug Administration (FDA) as ‘a measurement based on a report that comes directly from the patient (i.e. study subject) about the status of a patient’s health condition without amendment or interpretation of the patient’s response by a clinician’ [3, 4]. Quality of life (QoL) is one of the most reported PROs and can be measured using generic QoL questionnaires, such as the SF-36(v2) [5]. These questionnaires can be used in a wide variety of populations, which is both their strength and weakness. They provide extensive multidimensional insight in the QoL, though lack the specificity to address key problems in specific populations. This led to the development of Core Outcome Measurement Indexes (COMIs), which include a set of disease-specific PROs that are important for a specific population. In 2011, Staerkle and Villiger developed a core outcome questionnaire specifically for inguinal hernia patients, the COMI-hernia questionnaire [6]. This validated questionnaire compares well to generic questionnaires such as the EQ-5D or EQ-VAS, and focuses on the patients’ perspective of specific problems for inguinal herniorrhaphy such as groin pain, testicular pain, pain during urination, work impairment, sensory disturbances, and patient satisfaction [6].
Arguably, PROs are the most important outcomes of any medical treatment. Despite the importance of these data, a 2014 review of Antonescu et al. states that between 2008 and 2012 only 16% of the 770 clinical articles published in the top five general surgery journals used at least one PRO [7]. Only ten of these articles concerned hernia-related research. Despite an increase in published PRO data during the last 2 years, to our knowledge the COMI-hernia scale has never been used to evaluate the outcome of inguinal herniorrhaphy other than in the original validation paper of Staerkle et al. [6].
This study is the first clinical prospective, single centre analysis of PROs using the COMI-hernia scale. The aim of this study is to evaluate the short- and long-term postoperative quality of life, function, patient well-being, pain, and social/work disability after total extraperitoneal inguinal hernia repair (TEP) and provide the first clinical experience of the COMI-hernia questionnaire.
Methods
Between January 2013 and December 2014, all patients of at least 18 years old who were scheduled for elective uni- or bilateral TEP herniorrhaphy in day-care surgery at a local hospital (Elkerliek Hospital, Helmond, The Netherlands), were approached for inclusion at the outpatient clinic.
All operations were performed under general anaesthesia by four experienced surgeons (≥300 procedures/surgeon). TEP was performed using a conventional three-port midline technique without the use of a balloon dissector [8]. All patients received a pre-shaped anatomically curved polypropylene mesh (Bard Davol® Inc., 3DMax™) that was not fixed with tackers or glue and therefore complied with the draft 2016 European hernia guidelines that states that mesh fixation in TEP is not necessary in almost all cases [9, 10].
Patients were asked to fill out the COMI-hernia questionnaire during their preoperative consultation, the 6-week postoperative consultation at the outpatient clinic, and after 1-year postoperatively. The 1-year postoperative questionnaires were sent via mail, and patients were asked to return the questionnaire within 3 weeks. Patients who did not respond within this period received one reminder by telephone; in case the patient did not return the questionnaire after the reminder they were considered lost to follow-up for that measurement. All results were analysed by two authors simultaneously (EM and DH).
COMI-hernia questionnaire
The questionnaire consists of 6 preoperative questions and 12 postoperative questions. The COMI-hernia questionnaire addresses five main outcomes; ‘general QoL’, ‘function’, ‘patient well-being’, ‘pain’, and ‘social and work disability’. All outcomes, except social and work impairment, and pain, were measured by a single question using a five-point Likert scale. Social and work disability was measured by two questions and pain was measured on a visual analogue scale (VAS). A subscore can be calculated for each domain by converting the Likert scale into a ten-point scale as described in an article of Mannion et al. concerning the original COMI-spine questionnaire [11].
Quality of life was evaluated using a single question: ‘Please reflect on the last week. How would you rate your quality of life?’ Function was defined as the interference of the groin problem with normal work during the past week. Patient well-being was defined as the patient’s willingness to live the rest of his/her life with the current groin problem. Clinically relevant pain was defined as a VAS ≥2. Chronic pain was defined as a VAS ≥2 one-year postoperatively according to the Medical Research Council Laparoscopic Groin Hernia Trial Group [12]. Social and work disability was defined as the number of days the patients had to cut down on work or were kept from work during the past four weeks.
Statistical analysis
Statistical analysis was performed with SPSS version 22, SPSS Statistics for Windows, IBM Corp. Armonk, NY, released in 2013. The baseline characteristics were analysed using descriptive statistics. Comparison of ordinal outcome variables between the three measurements was performed using the Friedman test. In case of a statistically significant difference between the three groups (α = 0.017), Wilcoxon signed rank tests were performed to identify the statistically significant (α = 0.05) group. Continuous variables were compared using a one-way Anova test followed by post hoc analysis (Tukey’s HSD), α = 0.05. Comparison of core outcomes between uni- and bilateral inguinal hernia patients was performed using independent samples T tests and Levene’s test for equality of variances.
Results
The flow of patients through the study is shown in Fig. 1. One hundred and twenty patients (113 men, 7 women) with a median age of 61 years (range 32–86 years) and a complete follow-up period of 1 year were included in the analysis. Informed consent was obtained from all individual participants included in this study. Thirty-five patients underwent bilateral inguinal hernia repair, and the median operation time was 41 min (range 12–142 min) (Table 1). Three patients had peroperative bleeding of an epigastric vessel that was successfully sutured. Eight patients had a postoperative complication; haematoma (n = 6), seroma (n = 1), or urinary tract infection (n = 1). Six patients (5%) had a recurrence hernia within one year.
Quality of life
Six weeks after surgery, 94% of the population reported either ‘good' or ‘very good’ QoL compared to 58% before the surgery. None of the patients scored their QoL as ‘very bad’. One year after surgery, 97% of the population reported ‘good’ or ‘very good’ QoL. There were no statistically significant differences between the QoL scores of patients with a haematoma or seroma versus the remainder of the population.
Function
Preoperatively, 65% of the population experienced ‘a little bit’ or ‘moderate’ functional impairment and 10% reported ‘a lot’ or ‘extreme’ functional impairment. Six weeks after surgery, 66% reported no impairment and 33% ‘a little bit’ or ‘moderate’ function impairment. One year after surgery, 81% reported no impairment and 15% reported ‘a little bit’ of functional impairment.
Patient well-being
Preoperative patient well-being was low (64% ‘very dissatisfied’). Six weeks postoperatively, 76% of the population was satisfied with the result and 19% was either ‘somewhat dissatisfied’ or ‘very dissatisfied’. The percentage of dissatisfied patients hardly improved over time, as 15% of the patients remained somewhat or very dissatisfied one year after surgery. In terms of benefit from the operation, 97% of the population reported that the operation ‘helped’ or ‘helped a lot’ six weeks postoperatively. One year postoperatively, this percentage decreased to 93%. At this time, two patients reported that the operation made their complaints worse. During the preoperative period and the first six postoperative weeks, all patients were satisfied with their ‘overall medical care’. One year postoperative, all but three patients were satisfied with their overall medical care.
Pain
Seventy-one percent of the population (85 patients) reported preoperative pain. Postoperative pain was reported by 19% of the population (22 patients) after six weeks and 14% (17 patients) after one year. By definition, these patients had chronic pain (14% VAS ≥ 2; 10% VAS ≥ 3). There was no statistically significant difference in the incidence of chronic pain amongst patients treated by either one of the four surgeons [F(3,113) = 0.384, p = 0.765].
Roughly, half of the patients who reported pain one year after surgery, reported pain six weeks after surgery as well (8/17 patients). The remaining nine patients developed delayed-onset chronic pain sometime between the 6-week and 1-year measurement. One of these nine patients had a recurrent hernia.
The following specific forms of pain were reported six weeks after the operation: pain of the testicle 25%, pain during urination 4%, and pain during intercourse 2%. One year after surgery, the prevalence of these complaints was: pain of the testicle 12.5%, pain during urination 2.5%, and pain during intercourse 0%.
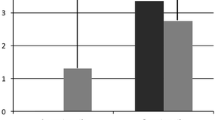
Social and work disability
Sixty-one percent of the patients experienced interference in their daily activities or work to some extent. Six weeks after surgery, 66% of patients reported limitations in their working ability, though the limitations they experienced were more severe compared to baseline (Fig. 2). Most limitations in work ability disappeared between the 6-week and 1-year measurement as one year postoperative 90% reported no limitation and 7% reported mild limitations during the past month.
Main outcome parameters of the COMI-hernia questionnaire. The average main outcome scores of the COMI-hernia questionnaire reported on a ten-point scale. A higher score correlates with a worse outcome. Asterisk score differs statistically significantly from the previous time of measurement; QoL preop. = 3.2 (SD ± 2.0), QoL 6 weeks postop. = 1.6 (SD ± 1.5), QoL 1 year postop. = 0.3 (SD ± 1.2) (pre vs 6 weeks p < 0.001; 6 weeks vs 1 year p < 0.001). Function preop. = 3.2 (SD ± 2.3), Function 6 weeks postop. = 1.0 (SD ± 1.6), Function 1 year postop. = 0.6 (SD ± 1.4) (pre vs 6 weeks p < 0.001; 6 weeks vs 1 year p = 0.017). Well-being preop. = 8.1 (SD ± 3.0), well-being 6 weeks postop. = 2.4 (SD ± 3.2), well-being 1 years postop. = 1.9 (SD ± 3.2) (pre vs 6 weeks p < 0.001; 6 weeks vs 1 year p = 0.337). Pain preop. VAS = 3.5 (SD ± 2.7), pain 6 weeks postop. = 1.0 (SD ± 1.7), pain 1 year postop. = 0.7 (SD ± 1.7) (pre vs 6 weeks p < 0.001; 6 weeks vs 1 year p = 0.017). So&wo disability preop. = 1.2 (SD ± 1.9), so&wo 6 weeks postop. = 2.1 (SD ± 2.6), so&wo 1 years postop. = 0.3 (SD ± 1.0) (pre vs 6 weeks p < 0.001; 6 weeks vs 1 years p < 0.001)
Comparison of uni- and bilateral hernias
All preoperative main outcome scores were higher in the bilateral group compared to the unilateral group. These differences were not statistically significant. The one year postoperative well-being score favoured the bilateral group (2.4 ± 3.5 vs 1.0 ± 2.5, p = 0.010). The remaining postoperative outcomes were comparable between the two groups.
Discussion
This prospective study measured five core PROs in 120 inguinal hernia patients undergoing TEP herniorrhaphy and observed that the majority of the population recovered well within the first six postoperative weeks. However, six weeks from surgery, patients still experienced clinically and statistically significant more interference in their social life and work, compared to baseline scores. This did not seem to have a negative impact on their perceived QoL or well-being scores, which notably improved six weeks after surgery. Ujiki et al. performed a similar prospective measurement of PROs after TEP repair and found that ‘social functioning’ and ‘pain’ did not improve immediately after surgery and may even worsen within the first three postoperative weeks [13]. In our series, ‘pain’ notably improved 6 weeks after surgery. These results indicate that postoperative pain seems to resolve somewhere between the third and sixth postoperative week, though social function remains impaired for a longer period of time. Both in our series as in the series of Ujiki et al. social function scores returned to normal one year after surgery. We recommend future studies to explore the timeframe between six weeks and one year postoperative in more detail to identify the duration of postoperative social and work impairment.
Our series showed no clinically significant differences between patients with a unilateral and bilateral hernia despite a better well-being score in the bilateral group one year postoperative, which can be explained by the vast majority of patients with chronic pain having a unilateral hernia (82%), which is consistent with the previously published randomised controlled trial of Peeters et al. that compared lightweight and heavyweight meshes for inguinal hernia repair in terms of quality of life. They did not observe any clinically or statistically significant differences between unilateral and bilateral hernia repairs in terms of QoL scores, return to work, or pain perception, 1, 3, 6, and 12 months after surgery, regardless of the mesh used [14].
In our series, eight patients developed delayed onset (≥6 weeks postoperative) of chronic groin pain, a phenomenon that was previously observed in anterior repairs by Delikoukos et al. [15]. They report that the origin of the delayed onset of pain can be found in mesh fixation and irritation of the ilioinguinal nerve, though this explanation does not translate well to endoscopic repairs, since the mesh is not fixed, making mechanical stimulation of the ilioinguinal nerve less likely [16]. Thermal irritation of the inguinal nerves has been suggested previously as a possible cause for the delayed onset of pain, though in our series no thermal cauterisation was used [17]. The delayed onset of the pain does suggest a neuropathic basis, therefore an inflammatory stimulation of the inguinal nerves or mechanical stimulation by ‘kinking’ of the inguinal nerves due to scar formation can serve as a possible explanation.
The overall incidence of chronic pain was slightly higher than anticipated (14% VAS ≥ 2; 10% VAS ≥ 3) and seemed to have a negative impact on the patient’s sense of well-being. However, this negative impact of chronic pain did not limit the patients in their perceived QoL, social or work function. Eighty-eight percent of the patients with chronic pain had preoperative pain versus 67% of the remaining population (p = 0.147 FEX), which could serve as an explanation for the relatively high incidence of chronic pain, since preoperative pain is a known risk factor for chronic postoperative pain [18, 19].
A previous study of Bansal et al. reported a lower incidence of chronic pain (1.25%, 3 months postoperative VAS ≥ 3) after TEP repair [4]. Other studies such as Ujiki et al. reported a chronic pain incidence <2% based on the Carolina Comfort Scale outcome, though using the SF-36 13% of the population reported more pain one year after surgery compared to baseline [13]. Burgmans et al. included 473 patients to evaluate postoperative pain with a VAS score and Inguinal Pain Questionnaire [20]. In their series, they found a chronic pain incidence of 10% defined as ‘any pain’ one year postoperative, as did Eklund et al. who reported a similar incidence of 10% chronic pain one year after surgery in their prospective trial of 665 patients [21]. A 2016 registry-based study of Gutlic et al. reported a 7.7% incidence of chronic pain using a cross-sectional analysis of 1110 patients [22]. Overall, the incidence of chronic pain after inguinal hernia repair varies from 0 to 54% in published literature [17, 23]. The wide variety of chronic pain incidence can be explained by the overwhelming amount of data concerning the complex, multidimensional problem of postoperative pain, combined with inconsistent outcome definitions and measurement tools [24]. This stipulates the need for standardised PROs, measured with standardised instruments to increase inter-study comparability.
The COMI-hernia questionnaire has made an attempt to standardise the most important PROs in inguinal hernia repair. The use of a single question to evaluate QoL worked well in clinical practice and seemed to provide an overall estimation of the self-perceived health status of the patient. However, the authors would argue that the COMI-hernia scale is difficult to interpret for the patient and the physician. The distinction between question five ‘during the past 4 weeks, how many days did you cut down on the things you usually do because of your groin problem’ and question six ‘during the past 4 weeks, how many days did your groin problem keep you from going to work (job, school, housework)’ confused the patients due to the similarity in outcome. Unemployed or retired patients frequently skipped question six because they felt it did not apply to them. Moreover, the subdomain ‘function’ defined as interference of the groin problem with normal work during the past week, closely resembles the subdomain of ‘work and social impairment’. A suitable alternative to the COMI-hernia questionnaire could be the EuraHS-QoL questionnaire which was recently validated for inguinal hernia patients [25]. This nine-item questionnaire is short, focuses on pain, function impairment, and cosmetic result.
The present study has limitations. Only 75% of the included patients (120 of 161 patients) completed the follow-up period of one year. The COMI-hernia questionnaire is a valid, reliable and relatively short questionnaire, though it is not a powerful tool in discriminating different origins of pain (i.e. during strenuous physical exercise, walking, or lifting heavy objects). The original COMI-hernia questionnaire is validated in German, though published in English. For the present study a Dutch translation was used. Despite these limitations, the authors feels that this prospective, single centre series with experienced surgeons and clear description of mesh and fixation method provides enough evidence for the following conclusion.
Conclusion
The vast majority of patients recovered well after TEP repair with a good quality of life, and fast restore of function. Patient well-being was lower than expected, possibly due to a relatively high incidence of chronic pain (VAS ≥ 2; 14% of the population). Chronic pain did not seem to affect long-term social and work disability. There were no clinically relevant differences between patients with a unilateral or bilateral hernias. The COMI-hernia questionnaire provided reasonable insight in the patient’s experience, though was difficult to interpret for both patient and physician.
References
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. The Lancet 362(9395):1561–1571
Simons MP et al (2003) The ‘Inguinal Hernia’ guideline of the Association of Surgeons of the Netherlands. Ned Tijdschr Geneeskd 147(43):2111–2117
Food and Drug Administration Center for Evaluation Research (2009) Guidance for industry patient-reported outcome measures: use in medical product development to support labeling claims, p 43. http://www.fda.gov. Accessed Aug 2016
Bansal VK et al (2013) A prospective, randomized comparison of long-term outcomes: chronic groin pain and quality of life following totally extraperitoneal (TEP) and transabdominal preperitoneal (TAPP) laparoscopic inguinal hernia repair. Surg Endosc 27(7):2373–2382
Ware JE Jr (2000) SF-36 health survey update. Spine (Phila Pa 1976) 25(24):3130–3139
Staerkle RF, Villiger P (2011) Simple questionnaire for assessing core outcomes in inguinal hernia repair. Br J Surg 98(1):148–155
Antonescu I et al (2014) Outcomes reported in high-impact surgical journals. Br J Surg 101(5):582–589. doi:10.1002/bjs.9450 Epub 2014 Feb 26
Lange JF et al (2002) The preperitoneal tissue dilemma in totally extraperitoneal (TEP) laparoscopic hernia repair. Surg Endosc Other Intervent Tech 16(6):927–930
Bell RC, Price JG (2003) Laparoscopic inguinal hernia repair using an anatomically contoured three-dimensional mesh. Surg Endosc 17(11):1784–1788
HerniaSurge (2016) HerniaSurge guidelines, statements and recommendations. http://herniasurge.com/contact/. Accessed Aug 2016
Mannion AF et al (2005) Outcome assessment in low back pain: how low can you go? Eur Spine J 14(10):1014–1026
Grant AM, Scott NW, O’Dwyer PJ (2004) Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Br J Surg 91(12):1570–1574
Ujiki MB et al (2015) Patient-centered outcomes following laparoscopic inguinal hernia repair. Surg Endosc 29(9):2512–2519
Peeters E et al (2010) Laparoscopic inguinal hernia repair in men with lightweight meshes may significantly impair sperm motility: a randomized controlled trial. Ann Surg 252(2):240–246
Delikoukos S et al (2008) Re-operation due to severe late-onset persisting groin pain following anterior inguinal hernia repair with mesh. Hernia 12(6):593–595
Reinpold W et al (2015) Retroperitoneal anatomy of the iliohypogastric, ilioinguinal, genitofemoral, and lateral femoral cutaneous nerve: consequences for prevention and treatment of chronic inguinodynia. Hernia 19(4):539–548
Poobalan AS et al (2003) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19(1):48–54
Poobalan AS et al (2001) Chronic pain and quality of life following open inguinal hernia repair. Br J Surg 88(8):1122–1126
Dennis R, O’Riordan D (2007) Risk factors for chronic pain after inguinal hernia repair. Ann R Coll Surg Engl 89(3):218–220
Burgmans JP et al (2015) Pain after totally extraperitoneal (TEP) hernia repair might fade out within a year. Hernia 19(4):579–585
Eklund A et al (2010) Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Br J Surg 97(4):600–608
Gutlic N et al (2016) Impact of mesh fixation on chronic pain in total extraperitoneal inguinal hernia repair (TEP): a nationwide register-based Study. Ann Surg 263(6):1199–1206
Nienhuijs S et al (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review. Am J Surg 194(3):394–400
Bhangu A et al (2015) A detailed analysis of outcome reporting from randomised controlled trials and meta-analyses of inguinal hernia repair. Hernia 19(1):65–75
Muysoms FE et al (2016) A prospective, multicenter, observational study on quality of life after laparoscopic inguinal hernia repair with ProGrip laparoscopic, self-fixating mesh according to the European Registry for Abdominal Wall Hernias Quality of Life Instrument. Surgery 160(5):1344–1357
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SN reports grants from Johnson and Johnson, and grants from Medtronic, outside the submitted work. All other authors declare that they have no conflict of interest.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Statement of human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was indeed obtained from all individual participant included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mommers, E.H.H., Hünen, D.R.M., van Hout, J.C.H.M. et al. Patient-reported outcomes (PROs) after total extraperitoneal hernia repair (TEP). Hernia 21, 45–50 (2017). https://doi.org/10.1007/s10029-016-1554-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1554-y