Abstract
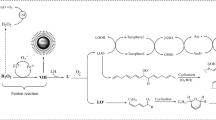
Hydrogen sulfide (H2S), a metabolic end product synthesized by the microbiota from l-cysteine, has been shown to act at low micromolar concentration as a mineral oxidative substrate in colonocytes while acting as an inhibitor of oxygen consumption at higher luminal concentrations (65 µM and above). From the previous works showing that polyphenols can bind volatile sulfur compounds, we hypothesized that different dietary proanthocyanidin-containing polyphenol (PACs) plant extracts might modulate the inhibitory effect of H2S on colonocyte respiration. Using the model of human HT-29 Glc–/+ cell colonocytes, we show here that pre-incubation of 65 µM of the H2S donor NaHS with the different polyphenol extracts markedly reduced the inhibitory effect of NaHS on colonocyte oxygen consumption. Our studies on HT-29 Glc–/+ cell respiration performed in the absence or the presence of PACs reveal rapid binding of H2S with the sulfide-oxidizing unit and slower binding of H2S to the cytochrome c oxidase (complex IV of the respiratory chain). Despite acute inhibition of colonocyte respiration, no measurable effect of NaHS on paracellular permeability was recorded after 24 h treatment using the Caco-2 colonocyte monolayer model. The results are discussed in the context of the binding of excessive bacterial metabolites by unabsorbed dietary compounds and of the capacity of colonocytes to adapt to changing luminal environment.
Similar content being viewed by others
References
Appeldoorn MM, Vincken JP, Aura AM, Hollman PC, Gruppen H (2009) Procyanidin dimers are metabolized by human microbiota with 2-(3,4-dihydroxyphenyl)acetic acid and 5-(3,4-dihydroxyphenyl)-gamma-valerolactone as the major metabolites. J Agric Food Chem 57:1084–1092
Arijs I, Vanhove W, Rutgeerts P, Schuit F, Verbeke K, De Preter V (2013) Decreased mucosal sulfide detoxification capacity in patients with Crohn’s disease. Inflamm Bowel Dis 19:E70–E72
Beaumont M, Andriamihaja M, Lan A, Khodorova N, Audebert M, Blouin JM, Grauso M, Lancha L, Benetti PH, Benamouzig R, Tome D, Bouillaud F, Davila AM, Blachier F (2016) Detrimental effects for colonocytes of an increased exposure to luminal hydrogen sulfide: the adaptive response. Free Radic Biol Med 93:155–164
Blachier F, Mariotti F, Huneau JF, Tome D (2007) Effects of amino acid-derived luminal metabolites on the colonic epithelium and physiopathological consequences. Amino Acids 33:547–562
Blachier F, Davila AM, Mimoun S, Benetti PH, Atanasiu C, Andriamihaja M, Benamouzig R, Bouillaud F, Tome D (2010) Luminal sulfide and large intestine mucosa: friend or foe? Amino Acids 39:335–347
Blachier F, Beaumont M, Andriamihaja M, Davila AM, Lan A, Grauso M, Armand L, Benamouzig R, Tome D (2017) Changes in the luminal environment of the colonic epithelial cells and physiopathological consequences. Am J Pathol 187:476–486
Bouillaud F, Blachier F (2011) Mitochondria and sulfide: a very old story of poisoning, feeding, and signaling? Antioxid Redox Signal 15:379–391
Carbonero F, Benefiel AC, Gaskins HR (2012) Contributions of the microbial hydrogen economy to colonic homeostasis. Nat Rev Gastroenterol Hepatol 9:504–518
Cires MJ, Wong X, Carrasco-Pozo C, Gotteland M (2016) The gastrointestinal tract as a key target organ for the health-promoting effects of dietary proanthocyanidins. Front Nutr 3:57
Cooper CE, Brown GC (2008) The inhibition of mitochondrial cytochrome oxidase by the gases carbon monoxide, nitric oxide, hydrogen cyanide and hydrogen sulfide: chemical mechanism and physiological significance. J Bioenerg Biomembr 40:533–539
De Preter V, Arijs I, Windey K, Vanhove W, Vermeire S, Schuit F, Rutgeerts P, Verbeke K (2012) Decreased mucosal sulfide detoxification is related to an impaired butyrate oxidation in ulcerative colitis. Inflamm Bowel Dis 18:2371–2380
Goubern M, Andriamihaja M, Nubel T, Blachier F, Bouillaud F (2007) Sulfide, the first inorganic substrate for human cells. FASEB J 21:1699–1706
Grasset E, Pinto M, Dussaulx E, Zweibaum A, Desjeux JF (1984) Epithelial properties of human colonic carcinoma cell line Caco-2: electrical parameters. Am J Physiol 247:C260–C267
Gu L, Kelm MA, Hammerstone JF, Beecher G, Holden J, Haytowitz D, Gebhardt S, Prior RL (2004) Concentrations of proanthocyanidins in common foods and estimations of normal consumption. J Nutr 134:613–617
Hidalgo IJ, Raub TJ, Borchardt RT (1989) Characterization of the human colon carcinoma cell line (Caco-2) as a model system for intestinal epithelial permeability. Gastroenterology 96:736–749
Jackson MR, Melideo SL, Jorns MS (2012) Human sulfide: quinone oxidoreductase catalyzes the first step in hydrogen sulfide metabolism and produces a sulfane sulfur metabolite. Biochemistry 51:6804–6815
Jenner AM, Rafter J, Halliwell B (2005) Human fecal water content of phenolics: the extent of colonic exposure to aromatic compounds. Free Radic Biol Med 38:763–772
Lagoutte E, Mimoun S, Andriamihaja M, Chaumontet C, Blachier F, Bouillaud F (2010) Oxidation of hydrogen sulfide remains a priority in mammalian cells and causes reverse electron transfer in colonocytes. Biochim Biophys Acta 1797:1500–1511
Leschelle X, Robert V, Delpal S, Mouille B, Mayeur C, Martel P, Blachier F (2002) Isolation of pig colonic crypts for cytotoxic assay of luminal compounds: effects of hydrogen sulfide, ammonia, and deoxycholic acid. Cell Biol Toxicol 18:193–203
Leschelle X, Goubern M, Andriamihaja M, Blottiere HM, Couplan E, Gonzalez-Barroso MD, Petit C, Pagniez A, Chaumontet C, Mignotte B, Bouillaud F, Blachier F (2005) Adaptative metabolic response of human colonic epithelial cells to the adverse effects of the luminal compound sulfide. Biochim Biophys Acta 1725:201–212
Li X, Bazer FW, Gao H, Jobgen W, Johnson GA, Li P, McKnight JR, Satterfield MC, Spencer TE, Wu G (2009) Amino acids and gaseous signaling. Amino Acids 37:65–78
Lodhia P, Yaegaki K, Khakbaznejad A, Imai T, Sato T, Tanaka T, Murata T, Kamoda T (2008) Effect of green tea on volatile sulfur compounds in mouth air. J Nutr Sci Vitaminol (Tokyo) 54:89–94
Mateos-Martin ML, Perez-Jimenez J, Fuguet E, Torres JL (2012) Profile of urinary and fecal proanthocyanidin metabolites from common cinnamon (Cinnamomum zeylanicum L.) in rats. Mol Nutr Food Res 56:671–675
Mimoun S, Andriamihaja M, Chaumontet C, Atanasiu C, Benamouzig R, Blouin JM, Tome D, Bouillaud F, Blachier F (2012) Detoxification of H2S by differentiated colonic epithelial cells: implication of the sulfide oxidizing unit and of the cell respiratory capacity. Antioxid Redox Signal 17:1–10
Perez-Jimenez J, Fezeu L, Touvier M, Arnault N, Manach C, Hercberg S, Galan P, Scalbert A (2011) Dietary intake of 337 polyphenols in French adults. Am J Clin Nutr 93:1220–1228
Portune KJ, Beaumont M, Davila AM, Tome D, Blachier F, Sanz Y (2016) Gut microbiota role in dietary protein metabolism and health-related outcomes: the two sides of the coin. Trends Food Sci Technol 57:213–232
Rodrigo R, Libuy M, Feliu F, Hasson D (2014) Polyphenols in disease: from diet to supplements. Curr Pharm Biotechnol 15:304–317
Scalbert A, Deprez S, Mila I, Albrecht AM, Huneau JF, Rabot S (2000) Proanthocyanidins and human health: systemic effects and local effects in the gut. BioFactors 13:115–120
Wong X, Carrasco-Pozo C, Escobar E, Navarrete P, Blachier F, Andriamihaja M, Lan A, Tome D, Cires MJ, Pastene E, Gotteland M (2016a) Deleterious effect of p-cresol on human colonic epithelial cells prevented by proanthocyanidin-containing polyphenol extracts from fruits and proanthocyanidin bacterial metabolites. J Agric Food Chem 64:3574–3583
Wong X, Madrid AM, Tralma K, Castillo R, Carrasco-Pozo C, Navarrete P, Beltran C, Pastene E, Gotteland M (2016b) Polyphenol extracts interfere with bacterial lipopolysaccharide in vitro and decrease endotoxemia in human volunteers. Funct Foods 26:406–416
Yoshioka Y, Akiyama H, Nakano M, Shoji T, Kanda T, Ohtake Y, Takita T, Matsuda R, Maitani T (2008) Orally administered apple procyanidins protect against experimental inflammatory bowel disease in mice. Int Immunopharmacol 8:1802–1807
Zeng QC, Wu AZ, Pika J (2010) The effect of green tea extract on the removal of sulfur-containing oral malodor volatiles in vitro and its potential application in chewing gum. J Breath Res 4:036005
Zweibaum A, Pinto M, Chevalier G, Dussaulx E, Triadou N, Lacroix B, Haffen K, Brun JL, Rousset M (1985) Enterocytic differentiation of a subpopulation of the human colon tumor cell line HT-29 selected for growth in sugar-free medium and its inhibition by glucose. J Cell Physiol 122:21–29
Acknowledgements
The authors wish to thank the financial support from Evaluation-Orientation de la Coopération Scientifique (Grant C12S01) and Fondecyt 1120290 as well as the financial support from AgroParisTech, INRA, Université Paris-Saclay, University of Chile in Santiago, and University of Concepcion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Andriamihaja, M., Lan, A., Beaumont, M. et al. Proanthocyanidin-containing polyphenol extracts from fruits prevent the inhibitory effect of hydrogen sulfide on human colonocyte oxygen consumption. Amino Acids 50, 755–763 (2018). https://doi.org/10.1007/s00726-018-2558-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-018-2558-y