Abstract
Enterovirus 71 (EV71) is the major causative agent of hand-foot-and-mouth disease (HFMD) and many neurological manifestations. Recently, this virus has become a serious concern because of consecutive epidemics in the Asia-Pacific region. However, no effective vaccine for EV71 has been discovered except two EV71 vaccines which are being used in local communities of China. To develop a safe and efficient EV71 vaccine candidate, we generated inactivated EV71 and evaluated its efficacy with γ-PGA/Chitosan nanoparticles (PC NPs), which are safe, biodegradable and effective as an adjuvant. The subcutaneous administration of inactivated EV71 with PC NPs adjuvant induces higher levels of virus-specific humoral (IgG, IgG1, and IgG2a) and cell-mediated immune responses (IFN-γ and IL-4). Additionally, inactivated EV71 with PC NPs adjuvant induces significantly higher virus neutralizing antibody responses compared to the virus only group, and resulted in a long lasting immunity without any noticeable side effects. Together, our findings demonstrate that PC NPs are safe and effective immunogenic adjuvants which may be promising candidates in the development of more efficacious EV71 vaccines.
Similar content being viewed by others
Introduction
Enterovirus 71 (EV71) is a non-enveloped, single strand positive sense RNA virus which has similar characteristics to poliovirus. It is classified within the species Enterovirus A genus Enterovirus of the family Picornaviridae [1]. Humans are the only known natural host of this virus and EV71 is a highly pathogenic virus causing sporadic outbreaks of HFMD (Hand-Foot-and-Mouth Disease) [2]. HFMD is characterized by usual fever, oral lesions, papulovesicular or maculopapular exanthem on the hands, feet, buttocks, knees and elbows. Children aged from 6 months to 5 years are at the highest risk of infection. Although HFMD is usually a self-limiting mild illness, severe complications can be associated with poliomyelitis-like acute flaccid paralysis, brainstem encephalitis, aseptic meningitis and severe systemic disorders like pulmonary oedema [3]. This virus was first found in California, USA in 1969 and is now a major public health issue across the Asia-Pacific region and beyond [2]. Because of this sudden significant increase in EV71 epidemics, it has attracted immense global health care attention.
There are a number of different approaches that have been taken to develop an effective treatment for EV71 infections. In particular, an inactivated whole virus vaccine approach has demonstrated advancements in recent years [4,5,6,7,8,9]. In addition to an inactivated whole virus vaccine, several other types of vaccines have also been evaluated for their efficacy. Arita et al. (2005) demonstrated that an EV71 mutant live attenuated vaccine (genotype A), which is characterized by attenuated neurovirulence and limited spread of virus, could confer effective protection against lethal EV71 infection. However, cynomolgus monkeys who were immunized with the vaccine still displayed mild neurological symptoms [10,11,12]. Initiatives to produce several types of EV71 subunit vaccine, using VP1 which contains the main neutralizing epitopes of EV71, have been attempted to address shortcomings associated with attenuated vaccines as well as problems such as reverse virulence [5]. VP1-expressing transgenic tomatoes, transgenic mouse milk and VP1 protein epitope-based peptide vaccines have also been evaluated as oral subunit vaccines [13, 14]. Furthermore, virus like particles (VLP) are emerging as vaccine candidates as they contain conserved, fully-conformational epitopes. VLPs pose no risk of virulence and EV71 VLPs have successfully been produced [15,16,17]. All the above approaches exhibit some positive effects in controlling EV71. In addition, inactivated virus vaccines have the potential to protect neonatal mice by passive transmission via serum from immunized adult mice and maternal antibodies [4, 5, 7].
Vaccine adjuvants are exceedingly important in enhancing vaccine immune responses. An ideal vaccine adjuvant should be biologically safe, highly immunogenic, easy to use, readily available and inexpensive. They should effectively deliver antigen to antigen presenting cells (APC) and improve the antigen processing and presentation by APCs. In addition, they need to induce the production of immunomodulatory cytokines and reduce the amount of antigen needed in the vaccine and the frequency of immunization required to confer protection. Currently, aluminum based mineral salts (alum) are widely used for clinical use. However, in spite of their immunogenicity and enhanced adjuvant properties, aluminum salts can cause several adverse effects, particularly in people with immunological and neurological complications [18,19,20,21,22,23]. In addition, alum adjuvant is known to be a weak stimulator of cellular immune responses. These issues suggest that it is important to explore alternative options for vaccine adjuvants.
Poly-γ-glutamic acid (γ-PGA) is a promising biodegradable polymer which is naturally produced by Bacillus subtilis isolated from Korean traditional fermented soybean paste, “chungkookjang”. This substance is water soluble, anionic, biodegradable, edible and relatively high in molecular weight (> 2000 kDa). Currently γ-PGA is used in a diverse range of applications which including the food industry, cosmetics and drug delivery [24]. In particular, γ-PGA/Chitosan nano particles (PC NPs) have demonstrated efficient adjuvant capabilities in delivering different antigens [25,26,27,28,29].
In this study, we generated inactivated EV71 and evaluated its vaccine efficacy with γ-PGA/Chitosan nanoparticles (PC NPs). The subcutaneous administration of inactivated EV71 with PC NPs adjuvant induced specific humoral, cell-mediated immune responses and significantly higher virus neutralizing antibody responses in mice.
Material and methods
Cell culture
African green monkey kidney (Vero) cells (ATCC CCL-81) and murine macrophage (Raw264.7) cells (ATCC TIB-71) were maintained in Dulbecco’s modified minimum essential medium (DMEM) (Gibco, USA) containing 10% fetal bovine serum (FBS) (Gibco, USA) and 1% antibiotic/antimycotic (A.A) (Gibco, USA) at 37 °C with 5% CO2 until use.
Murine bone marrow derived dendritic cells (BMDC) were prepared. Briefly, the femurs and tibia were collected from 6-8 week old BALB/c mice under aseptic conditions and washed with 70% alcohol followed by PBS washing. Each epiphysis was cut off and flushed with RPMI (Gibco, USA) medium to collect bone marrow cells. The cell suspension was filtered through a 40 µm cell strainer (BD Falcon, USA) and centrifuged at 1200 rpm for 3 min to collect the cell pellet. The collected cell pellet was then re-suspended with 200 µl of RBC lysis buffer to obtain RBC free bone marrow cells. The purified cells were then seeded in cell culture flasks and stimulated with RPMI medium containing GM-CSF and IL-4 and maintained for 6-7 days at 37 °C with 5% CO2 until dendritic cells (DC) were formed.
Peripheral blood mononuclear cells (PBMC) were isolated from different vaccinated animals. Mice were anaesthetized and blood samples were collected by cardiac puncture and PBMC were separated as described previously [30].
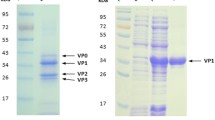
Purification and inactivation of EV71
The Enterovirus 71 (TW98-4643) was kindly provided by the microbiology laboratory, Faculty of Medicine, University of Ulsan, South Korea. Virus was amplified in Vero cells containing serum free DMEM for 48-72 hrs. The amplified virus was then layered on a 20% sucrose column and ultra-centrifuged at 36000 rpm for 6 hrs using an SW41 rotor (Beckman, USA). The purified virus pellet was then re-suspended in TNE buffer, filtered through a 0.22 µm syringe filter and the viral titer was determined using TCID50. The purified virus was then inactivated by adding 37% formaldehyde (Sigma, USA) at a 1:4000 (v/v) ratio and incubating at 37 °C for 14 days.
Preparation of γ-PGA/Chitosan nano particles
Preparation of the PC NPs was performed by a simple ionic interaction as described previously, with some modifications [24]. The low molecular weight (LMW) chitosan (Sigma–Aldrich) was first dissolved in distilled water and then chloridized by adding HCl (pH 4). Then, the chloridized chitosan was treated with chitosanase to achieve a lower molecular mass (< 15 kDa). The high molecular weight (HMW) γ-PGA was prepared by collecting the supernatant from B. subtilis sub sp. Chungkookjang culture broth and mixing it with 3 volumes of ethanol to precipitate. The precipitated γ-PGA was lyophilized, dissolved in 10 mM Tris–HCl buffer (pH 7.5), treated with proteinase K, and dialyzed against distilled water. Following dialysis, γ-PGA was purified using an ion-exchange chromatography. First, a dialyzed γ-PGA sample was subjected to a Sep-Pak Plus Waters Accell Plus QMA cartridge (Millipore, USA) equilibrated with distilled water. After washing with distilled water, the cartridge column charged with γ-PGA was developed stepwise with NaCl solutions, from 0.1 to 1.0 M. For the preparation of PC NPs, chitosan was prepared at 0.98 mg/ml in 0.9% NaCl solution (pH 5-5.2) and HMW γ-PGA was prepared at 1.4 mg/ml in 0.9% saline (pH 6.2-6.8). After filtering both solutions, the chitosan (0.98 mg/ml) and γ-PGA (1.4 mg/ml) were mixed together into the agitated mixture by dripping. The particle size of NPs was evaluated using a dynamic light scattering (DLS) method with a Zetasizer Nano ZS (Malvern Instruments, UK).
Elisa
PC NPs treated BMDC and Raw264.7 cell culture supernatant were collected at 12 hrs and 24 hrs post treatment and IL-6, IL-12 and IFN-β secretion were measured using commercialized ELISA kits (BD biosciences, USA). The levels of anti-EV71 specific antibodies in the serum were detected by indirect ELISA. Plates were coated with 100 µl/well of 105 TCID50 inactivated EV71-4643 virus in carbonate-coating buffer (15 mM Na2CO3, 35 mM NaHCO3, pH 9.8) and incubated at 4 °C overnight, which was followed by a 1hr room temperature incubation with 10% skim milk. Diluted sera (1:1000) from immunized mice were added into the plate and incubated for 1.5 hrs at room temperature. After three consecutive washes, horseradish peroxidase (HRP) conjugated goat anti-mouse IgG antibody (1:2000) was added into each well. The reaction was developed by 100 µl TMB substrate (3, 3′, 5, 5′-etramethylbenzidine) for 10 min in the dark and the reaction was terminated by adding 50 µl 2M H2SO4. The optical densities at 450 nm were determined with a microplate absorbance reader.
qPCR
Murine PBMC cells were collected and stimulated with inactivated EV71 virus. Total mRNA was isolated from cells using an RNeasy Mini Kit (Qiagen) and cDNA was synthesized using a commercially available reverse transcriptase kit (TOYOBO). The gene induction of different targets was quantified by quantitative polymerase chain reaction (qPCR) by using Quanti-tect SYBR Green PCR kit according to the manufacturer’s instructions (Qiagen) and gene induction value was obtained using the 2−ΔΔCT method as described previously [31]. The primer sequences used for qPCR are displayed in Table 1.
Mice immunization
Female 6 weeks old BALB/c mice were purchased (Samtako, Korea) and grouped according to the experimental plan. Mice were housed in ventilated cages and maintained with pelleted feed and tap water ad libitum. Mice immunization was carried out with different treatment combinations as displayed in Table 2. Blood samples were collected from the retro-orbital sinus at different time points as described in the vaccination schedule (Fig. 2A). The collected blood samples were then centrifuged at 12000 rpm for 10 min at 4 °C and the serum was separated and stored at −20 °C until use. At day 42 following the first immunization, five mice from each group were sacrificed to collect splenocytes and PBMC.
Enzyme-linked immunosorbent spot (ELISPOT) assay
ELISPOT assay was performed as described previously [32] with some modifications. Briefly, ELISPOT plates (BD Bioscience, San Diego, USA) were coated either with gamma interferon (IFN-γ) or Interleukin-4 (IL-4) antibodies and incubated at 4 °C for overnight. Subsequently, wells were washed with appropriate buffers and blocked with RPMI media containing 10% FBS. Mice were euthanized and splenocytes were freshly isolated. Subsequent to blocking, plates were washed and splenocytes were added into wells (5 × 105 cells/well) along with either phytohemagglutinin 10 μg/ml (Gibco, USA) or heat inactivated virus (3 μg/ml). After 24 hr incubation at 37 °C with 5% CO2, detection antibodies (Biotinylated anti-mouse IFN-γ or IL-4) were added. Plates were then conjugated with streptavidin-HRP for one hour followed by washing and finally ELISPOT AEC substrate was added. At the time of optimum spot development, the reaction was terminated by adding distilled water and plates were dried at room temperature. Finally, the spots were enumerated by the ELISPOT plate reader (CTL-Immunospot S5 UV analyzer, Cellular technologies, USA).
Lymphoproliferation assay
Immunized mice were euthanized at 42 days post-immunization and splenocytes were collected. Then RBC-lysed splenocytes were cultured in flat-bottom 96-well plates either with EV71 inactivated virus (3 μg/ml) or phytohemagglutinin/PHA (10 μg/ml) for 72 hrs. The proliferation of EV71 specific lymphocytes were evaluated using MTT assay (Roche Applied Science, USA) as described previously [33].
Virus neutralization assay
Sera from vaccinated mice were heat inactivated at 56 °C for 30 min and serially two fold diluted with DMEM. The diluted sera were then mixed with an equal volume of 100 TCID50 EV71. The mixture was incubated at 4 °C for 18-24 hrs to neutralize the virus. Subsequently, 100 µl from the mixture was added into each well of 96 well plates containing Vero cells. After 4-5 days of incubation at 37 °C with 5% CO2, the cytopathic effect (CPE) was observed and the TCID50 value was calculated. The 50% neutralization inhibition dose was calculated as the reciprocal of the serum dilution that yielded a 50% reduction in the virus titer using the Reed-Muench method [34].
Cell cytotoxicity assay
Vero cells or Raw264.7 cells were treated with different concentrations of PC NPs and cell cytotoxicity was assessed using the MTT cell cytotoxicity assay (Roche, USA) in Vero cells or by a trypan blue cell viability test in Raw264.7 cells.
Results
PC NPs induce cytokines in murine bone marrow derived dendritic cells (BMDC) and Raw264.7 cells
Previous studies have demonstrated enhanced immune responses with γ-PGA treatment. Specifically, γ-PGA induces TLR2 and TLR4 signaling pathways and upregulates cytokine production [35]. Here we demonstrate the ability of PC NPs to induce different types of cytokines in murine bone marrow derived dendritic cells (BMDC) and murine macrophages (Raw 264.7) in comparison to LPS or recombinant mouse IFN-β (mIFN-β) treatment. We assessed the cytokine induction by PC NPs (1 mg/ml) and compared the efficacy with 100 ng/ml of LPS or 1000 units/ml of mIFN-β treatment. As shown in Fig. 1A and 1B, the secreted IFN-β, IL-6 and IL-12 from PC NPs treated BMDC were comparable to levels induced by LPS treatment. The cytokine secretion by PC NPs treated Raw264.7 cells was also comparable to LPS or mIFN-β treatments. These results suggest that PC NPs possess a potent immune stimulatory effect which is a key feature of an effective vaccine adjuvant. These secreted cytokines would increase the activity of various APCs and enhance antigen presentation.
Characterization of PC NPs in vitro. A and B. Cytokine induction in murine BMDCs and murine macrophages (Raw264.7) upon stimulation with LPS (100 ng/ml) or mIFN-β (1000 units/ml) or PC NPs (1 mg/ ml). At 12 hrs and 24 hrs post treatment, supernatant was collected and IL-6, IFN-β and IL-12 production was measured using ELISA, “x” axis denoted different treatment groups and “y” axis denoted cytokines induction (pg/ml). C and D. The cytotoxic effects of PC NPs in Vero cells and Raw264.7 cells in response to serial concentrations of PC NPs (10 mg/ml to 0.156 mg/ml) were measured by MTT assay and Trypan blue exclusion test respectively. Cells treated with DMEM containing 10% FBS + 1% A.A were used as the positive control. Bars denote mean ± S.D
Evaluation of the stability and safety of PC NPs in vitro
Stability and biosafety are top priorities in the development of any vaccine adjuvant. γ-PGA and chitosan are naturally synthesized and biodegradable in nature. However, to confirm their suitability as a treatment in our study, we evaluated the level of cytotoxicity by treating Vero cells or Raw264.7 cells with different concentrations. According to the MTT assay, none of the tested PC NPs solutions (0.156 mg/ml to 10 mg/ml) showed cytotoxicity in Vero cells (epithelial cells) (Fig. 1C). Trypan blue cell viability assay also showed steady cell viability in Raw264.7 cells (immune cells) across the different concentrations that were tested (Fig. 1D). These results collectively demonstrate the high compatibility and safety of PC NPs for biological use.
Mice vaccinated with inactivated EV71 virus and PC NPs trigger higher humoral immunity
For these experiments we first purified and inactivated EV71 (see material and methods). Inactivation of EV71 was confirmed through the absence of cytopathic effect (CPE) in vitro (data not shown). To assess whether the mice vaccinated with inactivated EV71 and PC NPs could induce sufficient level of humoral immune responses, we measured the anti-EV71 serum IgG and its neutralizing activity against EV71. We compared these results with alum adjuvanted EV71 vaccine or with an inactivated virus only group. The immunization and serum collection was conducted as scheduled (Fig. 2A). Sera were diluted 1:1000 and indirect ELISA was performed to measure the anti-EV71 specific serum IgG level in different groups. As shown in Fig. 2B, during the 8th week of the first vaccination, all groups reached their highest serum antibody levels and both alum and PC NPs adjuvanted groups induced similar levels of total serum IgG, significantly more than the virus only group (P < 0.05). To determine the virus neutralizing activity in the sera of vaccinated animals, the same sera were serially (two-fold) diluted and treated against 100 TCID50 of virulent EV71 virus (Fig. 2C). Interestingly, alum and PC NPs adjuvant groups elicited similar levels of anti-EV71 neutralizing activity reaching up to log211-212 while the virus only vaccinated group only achieved log28. This elevated antibody level suggests that inactivated EV71 virus vaccine with a PC NPs adjuvant can induce sufficient levels of humoral immune induction, and these levels are comparable to the effects of alum adjuvant.
Humoral immune activation in vaccinated mice. A. A schematic representation of the animal experiments. The mice were grouped and received subcutaneous vaccinations as mentioned in Table 2. The close arrows (pointing down) indicate immunization. The open arrows pointing down indicate the time of ELISPOT and Th cell proliferation assays. Similarly, the open arrows pointing up indicate the time of serum collection. Sera were collected on weeks 0, 2, 4, 6, 8 after the 1st vaccination and at week 24 (6-months) following the 2nd vaccination (for long lasting antibody, as shown in fig. 4). Spleens and PBMC were collected on week 6 after 1st vaccination to evaluate cellular immune responses and Th cell proliferation (shown in fig. 3). B. Anti-EV71 serum IgG levels for the differently vaccinated animal groups. Sera were collected every 2 weeks for up to 8 weeks and tested for anti-EV71 IgG antibodies using indirect ELISA, “x” axis denotes weeks post immunization while the “y” axis denotes anti-EV71 serum IgG OD value at 450 nm. C. The same heat inactivated sera were tested for neutralizing activity against 100 TCID50 of pathogenic EV71. The 50% neutralization inhibition dose was calculated as the reciprocal of the serum dilution that yielded a 50% reduction in the virus titer using the Reed-Muench method, “x” axis denotes weeks post immunization while the “y” axis denotes EV71 neutralizing titer. D. The sera of vaccinated animals from the 2nd, 4th and 8th week after 1st vaccination was evaluated for IgG iso-types. IgG1 and IgG2a were tested by indirect ELISA with the “x” axis denoting weeks post immunization and the “y” axis denoting anti-EV71 serum IgG1 and IgG2a levels respectively. Bars denote mean ± S.D. The asterisks indicate significant differences between groups (p > 0.05)
Iso-typing of serum IgG of vaccinated mice
Having shown that the PC NPs adjuvanted EV71 vaccinated group demonstrated a high cell mediated immune response, we evaluated the specific IgG iso-types in the sera of vaccinated mice. As shown in Fig. 2D, both PC NPs and alum adjuvanted EV71 vaccinated groups showed higher IgG1 levels compared to IgG2a. However, IgG2a induction in the PC NP group was greater than in the alum group or virus only group. Since IgG2a level in sera is a good indicator of Th1 cell function, these findings suggest that PCNP is able to efficiently activate Th1 subset cells, in comparison to other vaccine groups.
The inactivated EV71 vaccine candidate with PC NPs induced higher cytotoxic T-lymphocyte (CTL) responses
An effective vaccine should ideally induce high cellular and humoral immune responses to defend against pathogenic infections. Notably, cell mediated immune responses are important to eliminate intracellular pathogens by killing infected cells. Therefore, we investigated the Th1 cell secreting IFN-γ levels in different vaccinated groups by stimulating splenocytes, either with inactivated virus or mitogen (positive control) (Fig. 3A). Our results show that mice immunized with antigen and PC NPs could induce significantly higher levels of IFN-γ when compared to the virus only vaccinated group (p > 0.05) (Fig. 3A). These elevated IFN-γ levels reflect elevated CD8+ T cell (CTL) activity and subsequent rapid clearance of infected cells. Additionally, we performed the IL-4 ELISPOT assay to check for Th2 cell activity. The group of mice with inactivated virus mixed with PC NPs showed a higher induction of IL-4 compared to the virus only-vaccinated group but not the alum adjuvanted group. Based on these results, we suggest that our vaccine can induce efficient activation of humoral and cell mediated immune responses in immunized mice.
Cellular immune responses in vaccinated mice. A. IFN-γ and IL-4 ELISPOT assay. Splenocytes from vaccinated mice were collected at 6 weeks post vaccination and re-stimulated either with mitogen (Phytohaemagglutinin/ PHA) or with heat inactivated EV71 for 24 hrs and IFN-γ and IL-4 secretion from T-lymphocytes were evaluated by ELISPOT assay. DMEM only media was used as a negative stimulator. The number of spots per well were enumerated using the ELISPOT plate reader, with the “x” axis denoting stimulation of splenocytes from vaccinated mice and the “y” axis denoting the number of spots per 5 × 105 splenocytes. B. Lymphoproliferation assay. Splenocytes from mice were collected at 6 weeks post vaccination and stimulated either with PHA or heat inactivated EV71 for 3 days. Cell proliferation was detected using MTT cell proliferation assay kit by measuring the absorbance at 570 nm. The “x” axis denotes stimulation of splenocytes from vaccinated mice while the “y” axis denotes OD value at 570 nm. C. Gene induction of Th1 related cytokines (IFN-γ and IL-2) and Th2 related cytokines (IL-10 and IL-4). PBMCs of vaccinated mice were collected at 6 weeks after vaccination using ficoll-paque density gradient centrifugation. Isolated PBMCs were cultured in 24 well plates and stimulated with inactivated EV71 for 24 hrs. PBMCs from non-vaccinated mice were used as a negative control. Total mRNA was extracted and cDNA was synthesized using reverse transcriptase. IFN-γ, IL-2, IL-10 and IL-4 mRNA relative fold induction was assessed using qPCR analysis. The “x” axis denotes re-stimulators of PBMC from vaccinated mice with inactivated EV71 virus while the “y” axis denotes mRNA fold values. Bars denote mean ± S.D. The asterisks indicate significant differences between groups (p > 0.05)
Mice vaccinated with inactivated EV71-PC NPs elicit an enhanced T lymphocyte proliferation
To investigate the antigen specific T lymphocyte proliferation in vaccinated animals, splenocytes were collected at 6 weeks after immunization (3 weeks after the 1st boost) and assessed for antigen specific T cell proliferation. PHA stimulation was used as a positive control for general polyclonal responses to nonspecific antigen stimulation. As shown in Fig. 3B, mice vaccinated with inactivated virus mixed with PC NPs showed a high EV71 specific T cell proliferation. As the strength of the T cell response to the ex vivo proliferation assay is an indicator of CD4+ T cell activation, this result suggests that the PC NPs adjuvant is able to activate T cells and thus induce cellular immunity.
PBMCs from mice vaccinated with PC NPs-adjuvanted vaccine showed high induction of Th1 and Th2 cytokine mRNAs
To further evaluate the function of our vaccine with PC NPs on the cellular and humoral immune responses, we evaluated Th1 and Th2 related cytokines at the mRNA level. For this purpose, we collected the PBMCs of vaccinated animals at 6 weeks after vaccination, cultured them in 96-well plates and re-stimulated them with inactivated EV71 virus. After 12 hrs stimulation, total mRNA was extracted, cDNA was synthesized and then analyzed using qPCR. IL-2 and IFN-γ gene induction were measured as a marker of Th1 activation, while IL-10 and IL-4 genes were measured as a marker of Th2 activation. Our results demonstrated that PBMCs from mice vaccinated with the PC NPs-adjuvanted vaccine group had high levels of Th1 and Th2 related cytokine gene induction, when compared to virus only vaccinated group (Fig. 3C). These results suggest that our vaccine can induce higher cellular and humoral immune responses.
PC NPs-adjuvanted EV71 vaccine can induce long-lasting immunity
The duration of immunity conferred by a vaccine is a key aspect of its effectiveness and potency. We measured the longevity of our vaccine response by assessing serum IgG levels and neutralizing capability 6 months after final vaccination. As shown in Fig. 4A and 4B, the PC NP-adjuvanted EV71 vaccine induced high levels of serum IgG and high neutralizing activity, comparable to the effects of alum-adjuvanted vaccine. Furthermore, the IgG iso-types within the vaccinated animals demonstrated that the PC NPs-adjuvanted EV71 vaccine could maintain comparatively higher levels of IgG2a for a longer period demonstrating the ability of our vaccine to activate Th1 subset cells for a prolonged duration (Fig. 4C).
Long-lasting immune induction following vaccination. A. Long-lasting anti-EV71 serum IgG antibody levels in vaccinated mice. Six months after the 2nd vaccination, sera were collected and tested for anti-EV71 IgG antibodies using indirect ELISA. The “x” axis denotes vaccinated groups 6 months after the 2nd vaccination while the “y” axis denotes anti-EV71 serum IgG OD values at 450 nm. B. The same sera were tested for neutralizing activity against 100 TCID50 of pathogenic EV71; “x” axis denotes vaccinated groups 6 months after the 2nd vaccination while the “y” axis denotes EV71 neutralizing titers. C. Serum IgG isotyping of vaccinated mice. Sera from mice 6 months after the 2nd immunization were collected and IgG1 and IgG2a isotypes were tested; “x” axis denotes vaccinated groups 6 months after the 2nd vaccination and “y” axis denotes anti-EV71 serum IgG1 and IgG2a levels respectively. Bars denote mean ± S.D. The asterisks indicate the significantly different groups (p > 0.05)
Discussion
Since the first discovery of vaccine adjuvants in the 1920s, adjuvants have been widely used in different vaccines to enhance their efficacy [36]. These vaccine adjuvants are important in increasing antibody responses, enhancing cellular immunity, reducing the dose of antigen required, reducing the frequency of vaccination and boosting immune responses in young or elderly people, especially those who respond poorly to vaccines. Although many vaccine adjuvants have been discovered, very few of them are able to use in humans due to safety concerns. There are many controversial ideas concerning commercially available, FDA-approved vaccine adjuvants such as aluminum salts, and many studies are underway to determine the safety risk of those adjuvants [21]. Insoluble aluminum salts (alum) have been widely used in human vaccines for many decades. These alum adjuvants can absorb antigens, stabilize and slowly release to enhance the immune system for longer periods, making them an efficient delivery system. However, alum induces relatively weak cell mediated immune responses. Additionally, aluminum is a known heavy metal and some studies have proven its side effects as a neurotoxin or immunocompromising agent [18, 20, 37,38,39,40,41]. Furthermore, the mechanism of action of alum is not fully understood [42]. Therefore, it is worthwhile to conduct in-depth safety assessments and explore other low risk alternatives for vaccine adjuvants.
Poly-gamma-glutamic acid is an anionic biodegradable substance and an edible capsular polymer secreted by B.subtilis which is generally regarded as a safe organism [43]. Currently γ-PGA is used in a diverse range of applications: in the food industry as a health food, thickener and stabilizer; as a moisturizer in cosmetics; a chelating agent in waste water treatment; as a hydrogel (especially super absorbent polymer, SAP) for environmental, agricultural, and biomedical product applications; as a biodegradable packing material; for drug delivery; as an osteoporosis preventing factor; a gene vector; curative biological adhesive; dispersant and enzyme immobilizing material [24]. Besides these applications, it has been used as a potent immunomodulation agent. Chitosan is also a cationic polysaccharide derived from chitin and is a safe and biocompatible polymer. Chitosan has already been tested as a potential nano carrier for delivering antigens in animal models and has been shown to promote effective immune responses [44,45,46,47].
In particular, γ-PGA/Chitosan nano particles (PC NPs) have demonstrated efficient adjuvant capabilities. Previously we reported the biological functions of PC NPs as effective mucosal adjuvants and evaluated the protective ability of recombinant proteins with PC NPs as influenza vaccine candidates [27, 28]. In the current study, we used PC NPs as a safe and effective adjuvant for an inactivated, whole EV71 virus, vaccine candidate administered subcutaneously - determining its effectiveness by assessing different immune responses.
First, we confirmed that PC NPs induce various inflammatory cytokines and type I interferon in APCs (Fig. 1A). High secretion of IL-12 can induce IFN-γ secretion by T cells and activate cytotoxic T lymphocytes, macrophages, NK cells and Th1 cell differentiation [48]. Moreover, the activated CTLs and NK cells continue to secrete IFN-γ, leading to macrophage activation which kill pathogens through phagocytosis [49]. In addition, increased levels of type I interferons result in the dampening of viral replication by activating several interferon stimulatory genes (ISGs) and enhancing antiviral protein production. Previously, Liu et al. (2005) showed type I interferons can protect mice against lethal EV71 infections [50]. In addition, type I interferons can enhance MHC class I molecules and activate CD8+ T cells. The activation of these various signaling pathways and cell mediated immune responses results in the rapid clearance of intracellular pathogens [51]. Based on our results, the PC NPs-adjuvanted group clearly displayed enhanced cell mediated immune responses when compared to the alum adjuvant group (Fig. 3A). These results are consistent with the results of previous studies published by Okamoto et al which showed significantly higher cellular immune responses with PCNPs when they used it together with an influenza hemagglutinin vaccine [52]. Intriguingly, Chang et al. (2006) demonstrated that induction of the Th1 cellular response is critical for EV71 vaccine development against severe infections. This is because pathogenic EV71 infections can drastically reduce host cellular immune responses, especially in younger children who are genetically determined with low levels of cellular immunity [53]. Therefore, our EV71 vaccine candidate, with PC NPs, could address these issues, particularly during active outbreaks, as it can effectively induce cell-mediated immunity.
Induction of humoral immunity is also a main priority for many vaccines. This controls extracellular pathogens through antibody binding and neutralization. Our virus neutralization assay showed the PC NPs-adjuvanted EV71 vaccinated group could neutralize pathogenic EV71 activity as effectively as the alum-adjuvanted group (Fig. 2C). According to Cao et al. (2013), the IgG1 subclass is the main player in EV71 virus neutralizing activity [54]. This explains the similar neutralizing capacity of the alum and PC NPs vaccines as they induced similar levels of IgG1 (Fig. 2D). The elevated Th2 activity reflects the enhanced IgG1 levels in both groups. IL-4 and IL-10 are the main inducers of Th2 cell development from naive CD4+ T helper cells. Interestingly, we observed comparable IL-4 and IL-10 induction in re-stimulated PBMCs in the vaccinated groups (Fig. 3C).
The development of a commercial EV71 vaccine is a significant milestone. For the EV71 vaccine, enhanced delivery options such as nano-particles and superior immunogenic adjuvants with less or no adverse effects are required. Consequently, in this study we evaluated the efficacy and the immunogenicity of PC NPs as a potent adjuvant for the EV71 vaccine. PC NPs may be promising candidates in the development of more efficacious EV71 vaccines.
References
Chua KB, Kasri AR (2011) Hand foot and mouth disease due to enterovirus 71 in Malaysia. Virol Sin 4:221–228
Solomon T, Lewthwaite P, Perera D, Cardosa MJ, McMinn P, Ooi MH (2010) Virology, epidemiology, pathogenesis, and control of enterovirus 71. Lancet Infect Dis 10:778–790
Lee KY (2016) Enterovirus 71 infection and neurological complications. Korean J Pediatr 59:395–401
Yu CK, Chen CC, Chen CL, Wang JR, Liu CC, Yan JJ, Su IJ (2000) Neutralizing antibody provided protection against enterovirus type 71 lethal challenge in neonatal mice. J Biomed Sci 7:523–528
Wu CN, Lin YC, Fann C, Liao NS, Shih SR, Ho MS (2001) Protection against lethal enterovirus 71 infection in newborn mice by passive immunization with subunit VP1 vaccines and inactivated virus. Vaccine 20:895–904
Foo DG, Alonso S, Chow VT, Poh CL (2007) Passive protection against lethal enterovirus 71 infection in newborn mice by neutralizing antibodies elicited by a synthetic peptide. Microbes Infect 9:1299–1306
Bek EJ, Hussain KM, Phuektes P, Kok CC, Gao Q, Cai F, Gao Z, McMinn PC (2011) Formalin-inactivated vaccine provokes cross-protective immunity in a mouse model of human enterovirus 71 infection. Vaccine 29:4829–4838
Chen CW, Lee YP, Wang YF, Yu CK (2011) Formaldehyde-inactivated human enterovirus 71 vaccine is compatible for co-immunization with a commercial pentavalent vaccine. Vaccine 29:2772–2776
Ong KC, Devi S, Cardosa MJ, Wong KT (2010) Formaldehyde-inactivated whole-virus vaccine protects a murine model of enterovirus 71 encephalomyelitis against disease. J Virol 84:661–665
Arita M, Shimizu H, Nagata N, Ami Y, Suzaki Y, Sata T, Iwasaki T, Miyamura T (2005) Temperature-sensitive mutants of enterovirus 71 show attenuation in cynomolgus monkeys. J Gen Virol 86:1391–1401
Arita M, Ami Y, Wakita T, Shimizu H (2008) Cooperative effect of the attenuation determinants derived from poliovirus sabin 1 strain is essential for attenuation of enterovirus 71 in the NOD/SCID mouse infection model. J Virol 82:1787–1797
Arita M, Nagata N, Iwata N, Ami Y, Suzaki Y, Mizuta K, Iwasaki T, Sata T, Wakita T, Shimizu H (2007) An attenuated strain of enterovirus 71 belonging to genotype a showed a broad spectrum of antigenicity with attenuated neurovirulence in cynomolgus monkeys. J Virol 81:9386–9395
Chen HF, Chang MH, Chiang BL, Jeng ST (2006) Oral immunization of mice using transgenic tomato fruit expressing VP1 protein from enterovirus 71. Vaccine 24:944–2951
Chen HL, Huang JY, Chu TW, Tsai TC, Hung CM, Lin CC, Liu FC, Wang LC, Chen YJ, Lin MF, Chen CM (2008) Expression of VP1 protein in the milk of transgenic mice: a potential oral vaccine protects against enterovirus 71 infection. Vaccine 26:2882–2889
Hu YC, Hsu JT, Huang JH, Ho MS, Ho YC (2003) Formation of enterovirus-like particle aggregates by recombinant baculoviruses co-expressing P1 and 3CD in insect cells. Biotechnol Lett 25:919–925
Chung YC, Huang JH, Lai CW, Sheng HC, Shih SR, Ho MS, Hu YC (2006) Expression, purification and characterization of enterovirus-71 virus-like particles. World J Gastroenterol 12:921–927
Chung YC, Ho MS, Wu JC, Chen WJ, Huang JH, Chou ST, Hu YC (2008) Immunization with virus-like particles of enterovirus 71 elicits potent immune responses and protects mice against lethal challenge. Vaccine 26:1855–1862
Keith LS, Jones DE, Chou CH (2002) Aluminum toxicokinetics regarding infant diet and vaccinations. Vaccine 20(Suppl 3):S13–S17
Clements CJ, Griffiths E (2002) The global impact of vaccines containing aluminium adjuvants. Vaccine 20(Suppl 3):S24–S33
Jefferson T, Rudin M, Di Pietrantonj C (2004) Adverse events after immunisation with aluminium-containing DTP vaccines: systematic review of the evidence. Lancet Infect Dis 4:84–90
Tomljenovic L, Shaw CA (2011) Aluminum vaccine adjuvants: are they safe? Curr Med Chem 18:2630–2637
Meiri H, Banin E, Roll M (1991) Aluminum ingestion—is it related to dementia? Rev Environ Health 9:191–205
Mold M, Shardlow E, Exley C (2016) Insight into the cellular fate and toxicity of aluminium adjuvants used in clinically approved human vaccinations. Sci Rep 6:31578
Lin YH, Chung CK, Chen CT, Liang HF, Chen SC, Sung HW (2005) Preparation of nanoparticles composed of chitosan/poly-gamma-glutamic acid and evaluation of their permeability through Caco-2 cells. Biomacromolecules 6:1104–1112
Hamasaki T, Uto T, Akagi T, Akashi M, Baba M (2010) Modulation of gene expression related to Toll-like receptor signaling in dendritic cells by poly(gamma-glutamic acid) nanoparticles. Clin Vaccine Immunol 17:748–756
Kim S, Yang JY, Lee K, Oh KH, Gi M, Kim JM, Paik DJ, Hong S, Youn J (2009) Bacillus subtilis-specific poly-gamma-glutamic acid regulates development pathways of naive CD4(+) T cells through antigen-presenting cell-dependent and -independent mechanisms. Int Immunol 21:977–990
Moon HJ, Lee JS, Talactac MR, Chowdhury MY, Kim JH, Park ME, Choi YK, Sung MH, Kim CJ (2012) Mucosal immunization with recombinant influenza hemagglutinin protein and poly gamma-glutamate/chitosan nanoparticles induces protection against highly pathogenic influenza A virus. Vet Microbiol 160:277–289
Chowdhury MY, Kim TH, Uddin MB, Kim JH, Hewawaduge CY, Ferdowshi Z, Sung MH, Kim CJ, Lee JS (2017) Mucosal vaccination of conserved sM2, HA2 and cholera toxin subunit A1 (CTA1) fusion protein with poly gamma-glutamate/chitosan nanoparticles (PC NPs) induces protection against divergent influenza subtypes. Vet Microbiol 201:240–251
Yang J, Shim SM, Nguyen TQ, Kim EH, Kim K, Lim YT, Sung MH, Webby R, Poo H (2017) Poly-γ-glutamic acid/chitosan nanogel greatly enhances the efficacy and heterosubtypic cross-reactivity of H1N1 pandemic influenza vaccine. Sci Rep 7:44839
Baine MJ, Mallya K, Batra SK (2013) Quantitative real-time PCR expression analysis of peripheral blood mononuclear cells in pancreatic cancer patients. Methods Mol Biol 980:157–173
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25(4):402–408
Yamada A, Ziese MR, Young JF, Yamada YK, Ennis FA (1985) Influenza virus hemagglutinin-specific cytotoxic T cell response induced by polypeptide produced in Escherichia coli. J Exp Med 162:663–674
Khajuria A, Gupta A, Singh S, Malik F, Singh J, Suri KA, Satti NK, Qazi GN, Srinivas VK, Gopinathan Ella K (2007) RLJ-NE-299A: a new plant based vaccine adjuvant. Vaccine 25:2706–2715
Brown WF (1964) Variance estimation in the Reed-Muench fifty per cent end-point determination. Am J Hyg 79:37–46
Broos S, Lundberg K, Akagi T, Kadowaki K, Akashi M, Greiff L, Borrebaeck CA, Lindstedt M (2010) Immunomodulatory nanoparticles as adjuvants and allergen-delivery system to human dendritic cells: Implications for specific immunotherapy. Vaccine 28:5075–5085
Pasquale AD, Preiss S, Silva FTD, Garçon N (2015) Vaccine Adjuvants: from 1920 to 2015 and Beyond. Vaccines 3:320–343
Shaw CA, Tomljenovic L (2013) Aluminum in the central nervous system (CNS): toxicity in humans and animals, vaccine adjuvants, and autoimmunity. Immunol Res 56:304–316
Shaw CA, Li Y, Tomljenovic L (2013) Administration of aluminium to neonatal mice in vaccine-relevant amounts is associated with adverse long term neurological outcomes. J Inorg Biochem 128:237–244
Tomljenovic L (2011) Aluminum and Alzheimer’s disease: after a century of controversy, is there a plausible link? J Alzheimers Dis 23:567–598
Crepeaux G, Eidi H, David MO, Baba-Amer Y, Tzavara E, Giros B, Authier FJ, Exley C, Shaw CA, Cadusseau J, Gherardi RK (2017) Non-linear dose-response of aluminium hydroxide adjuvant particles: Selective low dose neurotoxicity. Toxicology 375:48–57
Exley C (2016) The toxicity of aluminium in humans. Morphologie 100:51–55
Marrack P, McKee AS, Munks MW (2009) Towards an understanding of the adjuvant action of aluminium. Nat Rev Immunol 9:287–293
Poo H, Park C, Kwak MS, Choi DY, Hong SP, Lee IH, Lim YT, Choi YK, Bae SR, Uyama H, Kim CJ, Sung MH (2010) New biological functions and applications of high-molecular-mass poly-gamma-glutamic acid. Chem Biodivers 7:1555–1562
Bacon A, Makin J, Sizer PJ, Jabbal-Gill I, Hinchcliffe M, Illum L, Chatfield S, Roberts M (2000) Carbohydrate biopolymers enhance antibody responses to mucosally delivered vaccine antigens. Infect. Immun. 68:5764–5770
Gogev S, de Fays K, Versali MF, Gautier S, Thiry E (2004) Glycol chitosan improves the efficacy of intranasally administrated replication defective human adenovirus type 5 expressing glycoprotein D of bovine herpesvirus 1. Vaccine 22:1946–1953
Jabbal-Gill I, Fisher AN, Rappuoli R, Davis SS, Illum L (1998) Stimulation of mucosal and systemic antibody responses against Bordetella pertussis filamentous haemagglutinin and recombinant pertussis toxin after nasal administration with chitosan in mice. Vaccine 16:2039–2046
Westerink MA, Smithson SL, Srivastava N, Blonder J, Coeshott C, Rosenthal GJ (2001) ProJuvant (Pluronic F127/chitosan) enhances the immune response to intranasally administered tetanus toxoid. Vaccine 20:711–723
Duque GA, Descoteaux A (2014) Macrophage cytokines: involvement in immunity and infectious diseases. Front Immunol 5:491
Denkers EY, Ricardo T, Gazzinelli RT (1998) Regulation and function of T-cell-mediated immunity during Toxoplasma gondii infection. Clin Microbiol Rev 11:569–588
Liu ML, Lee YP, Wang YF, Lei HY, Liu CC, Wang SM, Su IJ, Wang JR, Yeh TM, Chen SH, Yu CK (2005) Type I interferons protect mice against enterovirus 71 infection. J Gen Virol 86:3263–3269
Welsh RM, Bahl K, Marshall HD, Stina L (2012) Type 1 interferons and antiviral CD8 T-cell responses. PLoS Pathog 8:e1002352
Okamoto S, Yoshii H, Akagi T, Akashi M, Ishikawa T, Okuno Y et al (2007) Influenza hemagglutinin vaccine with poly(gamma-glutamic acid) nanoparticles enhances the protection against influenza virus infection through both humoral and cell-mediated immunity. Vaccine 25(49):8270–8278
Chang LY, Hsiung CA, Lu CY, Lin TY, Huang FY, Lai YH, Chiang YP, Chiang BL, Lee CY, Huang LM (2006) Status of cellular rather than humoral immunity is correlated with clinical outcome of enterovirus 71. Pediatr Res 60:466–471
Cao RY, Dong DY, Liu RJ, Han JF, Wang GC, Zhao H, Li XF, Deng YQ, Zhu SY, Wang XY, Lin F, Zhang FJ, Chen W, Qin ED, Qin CF (2013) Human IgG subclasses against enterovirus Type 71: neutralization versus antibody dependent enhancement of infection. PLoS One 8:e64024
Acknowledgements
This work was supported by Chungnam National University
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants by any of the authors. All animal experiments were conducted strictly in accordance with Guide for the Care and Use of Laboratory Animals (National Research Council, 2011) with the approval of Institutional Animal Care and Use committee of Bioleaders Corporation, Daejeon, South Korea. (reference number: BSL-ABSL-14-000).
Additional information
Handling Editor: Tim Skern.
Rights and permissions
About this article
Cite this article
Pathinayake, P.S., Gayan Chathuranga, W.A., Lee, HC. et al. Inactivated enterovirus 71 with poly-γ-glutamic acid/Chitosan nano particles (PC NPs) induces high cellular and humoral immune responses in BALB/c mice. Arch Virol 163, 2073–2083 (2018). https://doi.org/10.1007/s00705-018-3837-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-018-3837-3