Abstract
Background
Currently, the trajectory for insertion of an external ventricular drain (EVD) is mainly determined using anatomical landmarks. However, non-assisted implantations frequently require multiple attempts and are associated with EVD malpositioning and complications. The authors evaluated the feasibility and accuracy of a novel smartphone-guided, angle-adjusted technique for assisted implantations of an EVD (sEVD) in both a human artificial head model and a cadaveric head.
Methods
After computed tomography (CT), optimal insertion angles and lengths of intracranial trajectories of the EVDs were determined. A smartphone was calibrated to the mid-cranial sagittal line. Twenty EVDs were placed using both the premeasured data and smartphone-adjusted insertion angles, targeting the center of the ipsilateral ventricular frontal horn. The EVD positions were verified with post-interventional CT.
Results
All 20 sEVDs (head model, 8/20; cadaveric head, 12/20) showed accurate placement in the ipsilateral ventricle. The sEVD tip locations showed a mean target deviation of 1.73° corresponding to 12 mm in the plastic head model, and 3.45° corresponding to 33 mm in the cadaveric head. The mean duration of preoperative measurements on CT data was 3 min, whereas sterile packing, smartphone calibration, drilling, and implantation required 9 min on average.
Conclusions
By implementation of an innovative navigation technique, a conventional smartphone was used as a protractor for the insertion of EVDs. Our ex vivo data suggest that smartphone-guided EVD placement offers a precise, rapidly applicable, and patient-individualized freehand technique based on a standard procedure with a simple, cheap, and widely available multifunctional device.
Similar content being viewed by others
Introduction
Insertion of an external ventricular drain (EVD) is one of the most commonly performed procedures in daily neurosurgical practice [6, 7]. The standard technique is still the traditional non-navigation-assisted freehand placement exclusively guided by anatomical landmarks [2, 7, 28]. By this method, an EVD is usually inserted at Kocher’s point [9] and directed towards the nasion in the sagittal plane, and the tragus or slightly anterior in the coronal plane [13, 23]. However, imprecise EVD placement often occurs [3].
The desire for greater precision of ventriculostomy has led to various technical innovations and use of additional gadgets such as neurosonography [24], frameless stereotaxy [27], endoscopy [29], guiding protractors [8, 12], robotic [16] or electromagnetic neuronavigation [17], and fluoroscopy [4] or CT guidance [7]. Even a smartphone augmented-reality mobile device application (app), with or without a ventricular catheter-guiding tool, has already been developed [5, 25, 28].
Although all these techniques may lead to improved insertion accuracy, they are also associated with various disadvantages including additional time to perform the procedures, the need for head fixation, higher costs of materials, lack of ubiquitous availability of appropriate equipment, as well as time and effort for training and handling the systems. Moreover, neurosurgeons prefer methods that are quick and easy to use and barely differ from established clinical routine [24].
Taking these considerations into account and encouraged by results from an iPod-based navigation procedure described previously [11, 18], we developed a novel smartphone-guided, angle-adjusted technique for implantation of an EVD (sEVD). We systematically assessed its feasibility and accuracy in both a human artificial head model and a cadaver head.
Methods and materials
CT-based trajectory planning
A total of 20 EVD trajectories in a human artificial gel-filled head model with inserted ventricles (Classic Human Skull Model; 3B Scientific GmbH, Hamburg, Germany) (8/20) and a human formalin-fixed cadaveric head (Institute of Anatomy, University of Bern, Bern, Switzerland) (12/20) were determined on native multiplanar reformatted CT images (Somatom Definition Edge; Siemens Healthcare, Forchheim, Germany). A commercially available picture archiving and communication system (PACS) workstation (IDS7, Sectra AB, Linköping, Sweden) was used to analyze the images. In the PACS workstation, the native images of the cadaveric head and the head model were displayed in 3 planes: sagittal, coronal, and transversal. Each of 8 different insertion point was measured as determined on the head model 2.5 cm lateral to the midline and on a trajectory towards the upper edge of the external acoustic meatus at 10, 11, 12, and 13 cm posterior to the nasion. On the cadaveric head, 12 insertion points were measured as determined 2 and 3.5 cm paramedially, and 10, 12, and 14 cm behind the nasion, respectively. For each determined insertion point, the coronal image plain was adjusted to include three external landmarks: the insertion point as well as the upper edge of the tragi bilaterally. These three points represented the coronal insertion plain. There, the center of the ipsilateral frontal horn according to the sagittal and transversal ventricle diameters represented the optimal target for the sEVD tip. A trajectory was drawn from the insertion point on the skin of the human’s head and surface of the head model, respectively, to the center of the ipsilateral ventricle.
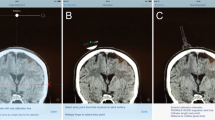
Finally, the angles between the sagittal midline and the trajectory, and the distances between the cranial entry point and the center of the ventricle, were measured as depicted in Fig. 1. The angle and the distance between entry point and target point in the center of the ipsilateral ventricle were noted to be at hand for the EVD placement.
Planning of sEVD insertion trajectories on multiplanar 3D reformatted native CT. Coronal (left) and sagittal (right) images of a human cadaveric head demonstrate determination of the sEVD insertion point located 12 cm distally to the nasion and 2 cm paramedially. The trajectory shown is tilted 12° laterally with a 5.22-cm insertion length. Note post-mortem intracranial air inclusion after anatomical fixation and loss of cerebrospinal fluid
Preparations for EVD placement
A smartphone (iPhone 4S, iOS 7.1.2; Apple Inc., Cupertino, CA, USA) was encased in a sterile cover (SteriPhone; Merete Medical GmbH, Berlin, Germany). A commercially available angle-measuring app (Clinometer; Plaincode App Development, Stephanskirchen, Germany) was installed on the smartphone as a protractor tool.
The heads (model and cadaver) were placed supine. The mid-cranial sagittal line and the insertion points were marked on the surface of both the model and the head. With a measuring tape, the insertion points determined were marked on the surface of both the model and cadaveric head. Additionally, electrocardiographic adhesive patches were placed on the nasion, the midline, and the tragus serving as palpable fiducials. To simulate clinical conditions, drapes were taped around Kocher’s point. The anatomical reference points were finally marked and a line between each insertion point and the upper edge of the external acoustic meatus was drawn on the drapes. This curvilinear line represented the shortest distance from the insertion point to the tragus. This line was adjusted at the CT-based trajectory planning in the sagittal and coronal plane as described above (Fig. 1).
For sEVD placement, the surgeon’s viewing direction was orientated on the coronal insertion plane including the curvilinear line, thereby the curvilinear line appeared straight. The base of the smartphone was positioned on this line and the surface of the smartphone-display was aligned to the coronal insertion plane allowing the most accurate sEVD insertion.
EVD placement
The longitudinal smartphone axis was aligned with the marked midline in the coronal insertion plane calibrated as 0° lateral deviation with the app (Fig. 2). The smartphone could be set to announce the lateral angle verbally, obviating visual control of the display. Especially because the angle-measuring app is still investigational and not labeled for neurosurgical use thus far, the accurate angle specification of the app was additionally verified by tilting the iPhone along the set-up triangle with specified angles.
Moreover, on the cadaveric head, a linear incision of 1 cm was made at each insertion point. With a twist drill (Cranial Access Kit; Integra NeuroSciences, Plainsboro, NJ, USA) a burr hole trephination was carried out.
One surgeons hand held the smartphone whereas the other hand attached the twist drill to it. The angulation of the drill was measured and adjusted with the protractor app of the smartphone orientated along the predefined coronal insertion plane (Fig. 3). Thus, the smartphone could be tilted laterally, but still remained in the same insertion plane, and the lateral angle and the twist drill could be controlled and adjusted.
Marking of midline in the sagittal plane, determination of the coronal insertion plan and angle-adjusted trephination. The insertion plane is represented by the curvilinear line that crosses the midline and the insertion point. The axis of the drill was routinely guided within the coronal insertion plane under visual control. It was tilted laterally toward the planned angle with the aid of the smartphone apps verbal angle specification. Placement of the twist drill was followed by angle-adjusted trephination
After trephination, the dura of the cadaveric head was perforated. The EVD (Bactiseal EVD Catheter system; Codman, Raynham, MA, USA) was tightly attached to the longitudinal axis of the smartphone and the planned lateral insertion angle was adjusted.
Each sEVD was inserted along the predetermined distance of the scaled catheter (Fig. 4). Durations of all procedures from the time of skin incision to final sEVD insertion in the head were measured.
Smartphone-navigated placement of the EVD. The drain was angle-adjusted with the smartphone and inserted into the ventricle. The midline is marked in the sagittal plane. The insertion plane is represented by the curvilinear line that crosses the midline and the insertion point. The axis of the catheter was always guided within the coronal insertion plane under visual control. It was tilted laterally toward the planned angle with the aid of the smartphone apps verbal angle specification
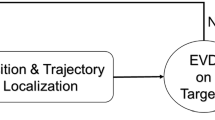
Post-interventional assessment
To analyze the results in the model and head, pre- and post-insertion CT images were used to assess accuracy and precision of sEVD insertions in a digital imaging and communications in medicine (DICOM) viewer. First, the images were multiplanar 3D reformatted. Then, the final position of each catheter insertion point, the planned trajectory, and the intracranial positions of the tips were marked. The insertion angle towards the planned trajectory and the lateral deviation in the coronal plane were determined. In addition, the deviation of the catheter tip from the target trajectory in the center of the ventricle was measured. The position of the catheter tips was graded as located either ipsi- or contra-lateral, and intra- or extra-ventricular. Occurrence of kinking was also noted. Additionally, the accuracy of each burr hole location behind the nasion and lateral to the midline and the actual intracranial insertion depth of the catheters was measured.
Data analysis
Results are provided as both mean values and standard deviation (SD). The following parameters were calculated: planned pre-insertional lateral implantation angles, inserted catheter lengths, locations of catheter tips and burr holes, and their accuracy and deviations from the optimal trajectories measured on CT. Statistical analyses were performed using the commercially available software SPSS Statistics, Version 22 (IBM Corp, Armonk, NY, USA).
Results
Head model
In the artificial head, the optimal lateral pre-insertional angles planned in the coronal plane averaged 10.54° (SD ± 5.37, range 4° to 19.6°), whereas the average angles measured on post-interventional CT imaging were 11.34° (SD ± 4.34, range 0.69° to 19.4°). After insertion, the mean deviation from the pre-insertional planned lateral angles was 1.73° (SD ± 1.12, range 0.15° to 3.1°). The post-interventional CT imaging showed that the catheter tips deviated on average 0.12 cm (SD ± 0.08, range 0.01–0.22 cm) from the initially planned optimal trajectory (Table 1).
All the sEVD burr holes were located on average 0.16 cm (SD ± 0.1, range 0–0.24 cm) more anteriorly and 0.04 cm (SD ± 0.02, range 0.01–0.07 cm) more medially than planned pre-interventionally. The planned mean optimal trajectory length was 4.1 cm (SD ± 0.12, range 3.9–4.3 cm) and, on post-insertional CT imaging, it averaged 4.03 cm (SD ± 0.13, range 3.8–4.23 cm). The mean deviation of the inserted catheter lengths was 0.13 cm (SD ± 0.12, range 0.04–0.4 cm) (Table 2). No instances of catheter kinking were observed after sEVD placement in the head model.
Cadaveric head
In the human head, the optimal lateral pre-insertional angles planned in the coronal plane averaged 26.8° (SD ± 14.87, range 8° to 49.3°), whereas the post-interventional angles measured on CT imaging were 26.58° (SD ± 13.88, range 9.3° to 45.9°). After insertion, the mean deviation from the planned pre-insertional lateral angles was 3.45° (SD ± 2.04, range 0.7° to 7.2°) (Table 1). The post-interventional CT imaging showed that the catheter tips deviated on average 0.33 cm (SD ± 0.21, range 0.06–0.81 cm) from the initially planned optimal trajectory (Table 1).
All the sEVD burr holes were located on average 0.7 cm (SD ± 0.09, range 0.6–0.81 cm) more anteriorly and 0.07 cm (SD ± 0.05, range 0.01–0.19) more medially than planned pre-interventionally. The planned mean optimal trajectory length was 5.34 cm (SD ± 0.5, range 4.7–6.45 cm) and, on post-insertional CT imaging, it averaged 5.63 cm (SD ± 0.44, range 5.0–6.64 cm). The mean deviation of the catheter lengths was 0.4 cm (SD ± 0.23, range 0.09–0.76 cm) (Table 2).
On post-interventional CT imaging, we observed 5 sEVDs with intracranial kinking (Table 1). These cases were excluded from further analysis. In the remaining 7 cases, the planned optimal lateral pre-insertional angles in the coronal plane averaged 20.13° (SD ± 12.51, range 8–43°), whereas post-interventional angles measured on CT imaging were 20.70° (SD ± 13.38, range 9.3–45.8°). After insertion, the mean deviation from the planned pre-insertional lateral angles was 2.1° (SD ± 1.05, range 0.7–4°). The catheter tips deviated on average 0.19 cm (SD ± 0.10, range 0.06–0.39 cm) from the optimal trajectory planned (Table 3). The planned mean optimal trajectory lengths were on average 5.37 cm (SD ± 0.34, range 5.01–6.05 cm) and on post-insertional imaging controls averaged 5.54 cm (SD ± 0.34, range 5.0–6.2 cm). The mean deviation of the catheter lengths was 0.35 cm (SD ± 0.19, range 0.09–0.6 cm) (Table 3).
Duration of procedure
The mean time taken for preoperative radiological measurement of planned cranial insertion points, lateral angles in the coronal plane, and optimal trajectory lengths was 3.23 min (SD ± 0.57, range 2.8–5 min) in both the human head model and the cadaveric head.
Only the human cadaveric head was used for determination of drilling time due to its comparability with real clinical conditions. The total time required for skin incisions, bone drilling, dura perforation, and smartphone-assisted insertion of the sEVDs was 108 min for 12 sEVDs, and 9 min on average for each insertion (SD ± 1.11, range 8.3–12 min).
Discussion
In daily neurosurgical practice, especially in emergency settings with critically ill patients, the patient’s outcome might substantially depend on immediate, safe, and sufficient EVD implantations [10]. Therefore, an accurate and rapid procedure is essential to reduce the consequences of uncontrolled intracranial pressure and associated morbidity or mortality [7, 14].
Ventricular diameter, angle, and target deviation and duration of procedure
An average anatomical diameter of unilateral ventricular frontal horns between 2.61 and 3.78 cm was determined in 150 healthy subjects [22]. In subgroups with pathological narrowing, the unilateral ventricular diameters may range from only 0.1 to 1.6 cm [16]. In contrast, in hydrocephalic patients, the bifrontal distances could be longer, varying from 2.6 to 4.8 cm [12].
In the present study, we measured a mean sEVD tip deviation from the target point of 0.33 cm in the human cadaveric head, including cases with kinking (12/20). After exclusion of catheters with kinking, the deviation of the remaining 7/20 sEVDs target was even less (0.19 cm).
Earlier studies on conventional, non-assisted freehand techniques have reported a mean deviation from the target of 0.97 cm [19], 1.43 cm [7], and 1.6 cm [10]. In studies on freehand ventriculostomy, a lateral angular variation of up to 5° in 51% and up to 15° in 90% of cases was documented by Abdoh et al. [1] Using CT-guided insertion, Gautschi et al. reported a deviation from the target of 0.96 cm [7]. O’Leary and colleagues documented 0.37-cm deviation with the Ghajar-Guide [19], whereas Reinertsen et al. reported a deviation from the target of less than 0.3 cm with a 3D-ultrasound-guidance for EVD insertions [24]. An average deviation of 0.16 cm of the EVD tip from the planned target in a study of smartphone-supported navigation planning, and use of a ventricular catheter-guiding tool was reported by Thomale and co-workers [28]. Finally, both Lollis et al. and Stieglitz and co-workers reported a mean distance of the catheter tip from the target of 0.15 cm after frameless navigated catheter insertion [16, 27]. Regarding the assignment of the determined entry point between CT and head, the plausibility of surface-matching using anatomical landmarks was expressed with a mean error of 0.35 to 0.5 cm [20, 21, 30]. The inaccuracy of angle measurement was correspondingly lower.
Duration of procedure
In the present study, measurements of the optimal insertion angle and intracranial length of catheters lasted on average 3.23 min. Gautschi et al. reported an average time of 3.8 min for planning of a neuronavigation-assisted EVD placement in a cadaver study [7].
Our average EVD insertion time-including drilling, durotomy, and smartphone-assisted insertion-was 9 min. Mahan et al. reported a total of 17 min on average, whereas Krötz and his colleagues reported a duration of 17 to 20 min for conventional EVD insertion [15, 17]. Furthermore, optimal placement of the catheter in a single pass compensates for the time for trajectory planning and decreases procedure-related complications [7, 14, 26, 31].
Advantages
Young neurosurgeons especially junior residents with limited experience very often perform insertions of an EVD while a successful implantation preferably at first attempt is imperative to reduce patient’s morbidity. An adequate preparation can essentially help to achieve this aim. The main advantage of the simple method described here is that it increases the probability of accurate one-time EVD insertion, especially if the ventricles are narrow, dislocated, or deformed. Furthermore, the technique applied is easy to learn, not time-consuming, corresponds well to previous conventional EVD implantation methods, and requires barely additional equipment and costs. Basically, the EVD may be inserted as usually, but the aligned and sterile-packed smartphone provides the possibility to display the optimal lateral insertion angle and this increases accuracy and patient safety.
Limitations
There are several important study limitations and caveats. First, the technique described has been evaluated exclusively in an ex vivo artificial human head model and formalin-fixed human cadaveric head. Although, in principle, we would expect our method to be transferable to clinical application, because smartphone-guided angle-control merely adds a sterile smartphone to conventional freehand insertions, its accuracy would need to be tested in a real clinical setting. Second, although our preliminary results are promising and suggest that the proposed method can offer a supplementary or alternative option to freehand ventricular catheterization, our values might be subject to bias. Both artificial head models and formalin-fixed human heads have a higher consistency than in a living human, contain no cerebrospinal fluid, but rather intraventricular air, increased atrophies, indurated sulci, and carry a higher risk of catheter kinking. The problem of kinking has already been reported as being associated with a significantly increased target deviation risk when compared with non-kinked catheters [7]. Furthermore, the small experimental sample size and number of EVD insertions decreases the statistical power of our study and decisive conclusions cannot be reached. Finally, for definite validation of its viability, testing of the method versus other and well-established techniques is of utmost importance.
Conclusions
The idea of useful medical apps uploaded on conventional mobile phones as portable and convenient operating tools for neurosurgeons led us to evaluate a smartphone device as a clinical guiding instrument for EVD insertions. Our data suggests that smartphone-assisted adjustment of the lateral insertion angle allows reliable EVD placement tailored to the individual patient.
Abbreviations
- app :
-
Augmented-realty mobile device application
- cm :
-
Centimeter
- CT :
-
Computed tomography
- DICOM :
-
Digital imaging and communications in medicine
- EVD :
-
External ventricular drain
- Fig :
-
Figure
- M :
-
Mean values
- PACS :
-
Picture archiving and communicating system
- SD :
-
Standard deviation
- sEVD :
-
Smartphone-navigated placed external ventricular drain
References
Abdoh MG, Bekaert O, Hodel J, Diarra SM, Le Guerinel C, Nseir R, Bastuji-Garin S, Decq P (2012) Accuracy of external ventricular drainage catheter placement. Acta Neurochir 154:153–159. https://doi.org/10.1007/s00701-011-1136-9
Bender M, Schwarm F, Stein M, Uhl E, Reinges MH (2019) Placement of external ventricular drain: comparison of two methods. J Neurol Surg A 80:116–121. https://doi.org/10.1055/s-0038-1676576
Brand C, Pala A, Kielhorn W, Wirtz CR, Kapapa T (2019) Do complication rates of ventricular drain placement differ between twist drill and burr hole in acute hydrocephalus? J Neurol Surg A 80(04):277–284. https://doi.org/10.1055/s-0039-1685195
Coluccia D, Anon J, Rossi F, Marbacher S, Fandino J, Berkmann S (2016) Intraoperative fluoroscopy for ventriculoperitoneal shunt placement. World Neurosurg 86:71–78
Eftekhar B (2016) App-assisted external ventricular drain insertion. J Neurosurg 125(3):754–758. https://doi.org/10.3171/2015.6.JNS1588
Fichtner J, Jilch A, Stieglitz LH, Beck J, Raabe A, Z’ Graggen WJ (2014) Infection rate of emergency bolt-kit vs. non-emergency conventional implanted silver bearing external ventricular drainage catheters. Clin Neurol Neurosurg 122:70–76. https://doi.org/10.1016/j.clineuro.2014.04.018
Gautschi OP, Smoll NR, Kotowski M, Schatlo B, Tosic M, Stimec B, Fasel J, Schaller K, Bijlenga P (2014) Non-assisted versus neuro-navigated and XperCT-guided external ventricular catheter placement: a comparative cadaver study. Acta Neurochir 156:777–785; discussion 785. https://doi.org/10.1007/s00701-014-2026-8
Ghajar JB (1985) A guide for ventricular catheter placement. Technical note. J Neurosurg 63:985–986. https://doi.org/10.3171/jns.1985.63.6.0985
Greenberg MSMD (2016) Handbook of Neurosurgery, 8th edn. Thieme, New York
Huyette DR, Turnbow BJ, Kaufman C, Vaslow DF, Whiting BB, Oh MY (2008) Accuracy of the freehand pass technique for ventriculostomy catheter placement: retrospective assessment using computed tomography scans. J Neurosurg 108:88–91. https://doi.org/10.3171/JNS/2008/108/01/0088
Jost GF, Bisson EF, Schmidt MH (2013) iPod touch-assisted instrumentation of the spine: a technical report. Neurosurgery 73:ons233-237; discussion ons237. https://doi.org/10.1227/neu.0000000000000023
Kim D, Son W, Park J (2015) Guiding protractor for accurate freehand placement of ventricular catheter in ventriculoperitoneal shunting. Acta Neurochir 157:699–702. https://doi.org/10.1007/s00701-015-2349-0
Kirkman MA, Muirhead W, Sevdalis N (2016) The relative efficacy of 3 different freehand frontal ventriculostomy trajectories: a prospective neuronavigation-assisted simulation study. J Neurosurg:1–8. https://doi.org/10.3171/2016.1.JNS152263
Kleffmann J, Pahl R, Deinsberger W, Ferbert A, Roth C (2016) Intracranial pressure changes during intrahospital transports of neurocritically ill patients. Neurocrit Care:1–6. https://doi.org/10.1007/s12028-016-0274-6
Krötz M, Linsenmaier U, Kanz K, Pfeifer K, Mutschler W, Reiser M (2004) Evaluation of minimally invasive percutaneous CT-controlled ventriculostomy in patients with severe head trauma. Eur Radiol 14:227–233. https://doi.org/10.1007/s00330-003-2134-y
Lollis SS, Roberts DW (2008) Robotic catheter ventriculostomy: feasibility, efficacy, and implications. J Neurosurg 108(2):269–274. https://doi.org/10.3171/JNS/2008/108/2/0269
Mahan M, Spetzler RF, Nakaji P (2013) Electromagnetic stereotactic navigation for external ventricular drain placement in the intensive care unit. J Clin Neurosci 20:1718–1722. https://doi.org/10.1016/j.jocn.2013.03.005
Oertel MF, Wolfla C, Park P (2013) iPod touch-assisted instrumentation of the spine: a technical report COMMENTS. Lippincott Williams & Wilkins, Philadelphia. https://doi.org/10.1227/neu.0000000000000023
O'Leary ST, Kole MK, Hoover DA, Hysell SE, Thomas A, Shaffrey CI (2000) Efficacy of the Ghajar Guide revisited: a prospective study. J Neurosurg 92:801–803. https://doi.org/10.3171/jns.2000.92.5.0801
Omara AI, Wang M, Fan Y, Song Z (2014) Anatomical landmarks for point-matching registration in image-guided neurosurgery. Int J Med Robot Comput Assist Surg 10:55–64. https://doi.org/10.1002/rcs.1509
Pfisterer WK, Papadopoulos S, Drumm DA, Smith K, Preul MC (2008) Fiducial versus nonfiducial neuronavigation registration assessment and considerations of accuracy. Oper Neurosurg 62:ONS201–ONS208. https://doi.org/10.1227/01.neu.0000317394.14303.99
Poudel D, Lamichhane HP, Paudel S, Chand RB (2015) Evaluation of size of ventricles of human brain using magnetic resonance imaging technique. J Inst Sci Technol 20:6–14. https://doi.org/10.3126/jist.v20i1.13904
Raabe C, Fichtner J, Beck J, Gralla J, Raabe A (2017) Revisiting the rules for freehand ventriculostomy: a virtual reality analysis. J Neurosurg:1–8. https://doi.org/10.3171/2016.11.JNS161765
Reinertsen I, Jakola AS, Friderichsen P, Lindseth F, Solheim O, Selbekk T, Unsgard G (2012) A new system for 3D ultrasound-guided placement of cerebral ventricle catheters. Int J Comput Assist Radiol Surg 7:151–157. https://doi.org/10.1007/s11548-011-0622-0
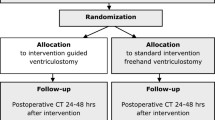
Sarrafzadeh A, Smoll N, Schaller K (2014) Guided (VENTRI-GUIDE) versus freehand ventriculostomy: study protocol for a randomized controlled trial. Trials 15:478. https://doi.org/10.1186/1745-6215-15-478
Soleman J, Marbacher S, Fandino J, Fathi AR (2012) Is the use of antibiotic-impregnated external ventricular drainage beneficial in the management of iatrogenic ventriculitis? Acta Neurochir 154:161–164. https://doi.org/10.1007/s00701-011-1156-5
Stieglitz LH, Giordano M, Samii M, Luedemann WO (2010) A new tool for frameless stereotactic placement of ventricular catheters. Neurosurgery 67:ons131–ons135; discussion ons135. https://doi.org/10.1227/01.NEU.0000382964.72262.9A
Thomale UW, Knitter T, Schaumann A, Ahmadi SA, Ziegler P, Schulz M, Miethke C (2013) Smartphone-assisted guide for the placement of ventricular catheters. Child’s Nerv Syst 29:131–139. https://doi.org/10.1007/s00381-012-1943-1
Villavicencio AT, Leveque JC, McGirt MJ, Hopkins JS, Fuchs HE, George TM (2003) Comparison of revision rates following endoscopically versus nonendoscopically placed ventricular shunt catheters. Surg Neurol 59:375–379; discussion 379-380. https://doi.org/10.1016/S0090-3019(03)00070-3
Woerdeman PA, Willems PW, Noordmans HJ, Tulleken CA, van der Sprenkel JWB (2007) Application accuracy in frameless image-guided neurosurgery: a comparison study of three patient-to-image registration methods. J Neurosurg 106:1012–1016. https://doi.org/10.3171/jns.2007.106.6.1012
Woernle CM, Burkhardt J-K, Bellut D, Krayenbuehl N, Bertalanffy H (2011) Do iatrogenic factors bias the placement of external ventricular catheters?—a single institute experience and review of the literature—. Neurol Med Chir 51:180–186. https://doi.org/10.2176/nmc.51.180
Acknowledgments
We would like to thank Lisa-Marie Wittler, Prof. Dr. med. Valentin Djonov, PD Dr. med. Matthias Bergmann and Dr. med. Kathrin Engler (✝), who served as scientific advisors, and Nane Boemke, Barbara Krieger, Nicole Schwendener, and Nicole Söll, who critically reviewed the study proposal for their invaluable support and contribution to this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The manuscript does not contain clinical studies or patient data. For this type of study formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgical technique evaluation
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Eisenring, C.V., Burn, F., Baumann, M. et al. sEVD—smartphone-navigated placement of external ventricular drains. Acta Neurochir 162, 513–521 (2020). https://doi.org/10.1007/s00701-019-04131-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04131-9