Abstract
Purpose
To determine whether posterior implant removal prevents stress-shielding-induced vertebral osteopenia within the posterior fusion area in surgically treated patients with adolescent idiopathic scoliosis (AIS).
Methods
Eighteen patients with major thoracic AIS (mean age, 43.3 years; range, 32–56 years; mean follow-up, 28.8 years, range, 20–39 years) who underwent posterior spinal fusion (PSF) alone between 1973 and 1994 were included. Participants were divided into implant removal (group R, n = 10, mean interval until implant removal, 50 months) and implant non-removal groups (group NR, n = 8). Bone mineral density was evaluated using the Hounsfield units (HU) of the computed tomography image of the full spine. The HU values of the UIV−1 (one level below the uppermost instrumented vertebra), apex, LIV+1 (one level above the lowermost instrumented vertebra), and LIV−1 (one level below the lowermost instrumented vertebra; as a standard value) were obtained. Stress-shielding-induced osteopenia was assessed as the UIV−1/LIV−1, apex/LIV−1, and LIV+1/LIV−1 HU ratios (× 100).
Results
Overall (median, 25th–75th percentile), the apex (144.7, 108.6–176.0) and LIV+1 (159.4, 129.7–172.3) demonstrated lower HU values than LIV−1 (180.3, 149.2–200.2) (both comparisons, p < .05). Comparison of groups R and NR showed no significant differences in the scoliosis correction rate, bone mineral density of the proximal femur, the HU absolute values of all investigated vertebrae, or in the HU ratios of the investigated vertebrae to LIV−1.
Conclusion
Instrumented PSF causes stress-shielding-induced osteopenia of the vertebral body within the fusion area in adulthood, which cannot be prevented by posterior implant removal, probably due to firm fusion mass formation.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.



Similar content being viewed by others
References
Cheng JC, Guo X, Sher AH (1999) Persistent osteopenia in adolescent idiopathic scoliosis. A longitudinal follow up study. Spine 24:1218–1222
Hung VW, Qin L, Cheung CS et al (2005) Osteopenia: a new prognostic factor of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am 87:2709–2716
Ishida K, Aota Y, Mitsugi N et al (2015) Relationship between bone density and bone metabolism in adolescent idiopathic scoliosis. Scoliosis 10:19
McAfee PC, Farey ID, Sutterlin CE et al (1989) Device-related osteoporosis with spinal instrumentation. Spine 14:919–926
Ito M, Fay LA, Ito Y et al (1997) The effect of pulsed electromagnetic fields on instrumented posterolateral spinal fusion and device-related stress shielding. Spine 22:382–388
Schreiber JJ, Anderson PA, Rosas HG et al (2011) Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am 93:1057–1063
Pervaiz K, Cabezas A, Downes K et al (2013) Osteoporosis and shoulder osteoarthritis: incidence, risk factors, and surgical implications. J Shoulder Elbow Surg 22:e1–e8
Pickhardt PJ, Pooler BD, Lauder T et al (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med 158:588–595
Meredith DS, Schreiber JJ, Taher F et al (2013) Lower preoperative Hounsfield unit measurements are associated with adjacent segment fracture after spinal fusion. Spine 38:415–418
Krappinger D, Bizzotto N, Riedmann S et al (2011) Predicting failure after surgical fixation of proximal humerus fractures. Injury 42:1283–1288
Schreiber JJ, Hughes AP, Taher F et al (2014) An association can be found between Hounsfield units and success of lumbar spine fusion. HSS J 10:25–29
Lenke LG, Betz RR, Harms J et al (2001) Adolescent idiopathic scoliosis. A new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83-A:1169–1181
Ylikoski M (2003) Height of girls with adolescent idiopathic scoliosis. Eur Spine J 12:288–291
Ohashi M, Hirano T, Watanabe K et al (2018) Bone Mineral density after spinal fusion surgery for adolescent idiopathic scoliosis at a minimum 20-year follow-up. Spine Deform 6:170–176
Szalay EA, Bosch P, Schwend RM et al (2008) Adolescents with idiopathic scoliosis are not osteoporotic. Spine 33:802–806
Zagra A, Lamartina C, Pace A et al (1988) Posterior spinal fusion in scoliosis: computer-assisted tomography and biomechanics of the fusion mass. Spine 13:155–161
Zagra A, Lamartina C, Pace A et al (1990) Computer-assisted tomography of scoliosis operated with or without Harrington’s rod. Biomechanics aspects of the fusion. Spine 15:796–802
Demir Ö, Öksüz E, Deniz FE et al (2017) Assessing the effects of lumbar posterior stabilization and fusion to vertebral bone density in stabilized and adjacent segments by using Hounsfield unit. J Spine Surg 3:548–553
Obid P, Richter A, Ubeyli H et al (2012) Spontaneous bilateral pedicle fracture 30 years after Harrington instrumentation for idiopathic scoliosis: a case report. J Med Case Rep 6:29
Tribus CB, Bradford DS (1993) Bilateral pedicular stress fractures after successful posterior spinal fusion for adult idiopathic scoliosis. Spine 18:1222e5
Knight RQ, Chan DP (1992) Idiopathic scoliosis with unusual stress fracture of the pedicle within solid fusion mass: a case report. Spine 17:849e51
Chaki O, Yoshikata I, Kikuchi R et al (2000) The predictive value of biomechanical markers of bone turnover for bone mineral density in postmenopausal Japanese women. J Bone Miner Res 15:1537–1544
Bergmann P, Body JJ, Boonen S et al (2009) Evidence-based guidelines for the use of biochemical markers of bone turnover in the selection and monitoring of bisphosphonate treatment in osteoporosis: a consensus document of the Belgian Bone Club. Int J Clin Pract 63:19–26
Potter BK, Kirk KL, Shah SA et al (2006) Loss of coronal correction following instrumentation removal in adolescent idiopathic scoliosis. Spine 31:67–72
Farshad M, Sdzuy C, Min K (2013) Late implant removal after posterior correction of AIS with pedicle screw instrumentation—a matched case control study with 10-year follow-up. Spine Deform 1:68–71
Funding
No funds were received in support of this work, and no relevant financial activities outside the submitted work exist.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kei Watanabe, Masayuki Ohashi, Toru Hirano, Keiichi Katsumi, Hirokazu Shoji, Tatsuki Mizouchi, Kazuhiro Hasegawa, Naoto Endo, and Hideaki E. Takahashi declare that they have no conflict of interest.
Ethical approval
The study was approved by the ethics committee of the Niigata University Graduate School of Medical and Dental Sciences. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
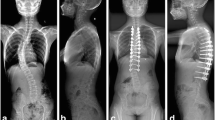
a Radiograph of a 20-year-old girl (group R) with Lenke type 2 adolescent idiopathic scoliosis before surgery. b Radiograph 3 years after posterior spinal fusion using Harrington instrumentation from T4 to L1. c Radiograph 33 years after implant removal, demonstrating acceptable correction. d HU values of CT at the UIV−1, apex, LIV+1, and LIV−1 levels showing 101.7, 27.7, 61.8, and 128.8 HU, respectively. HU, Hounsfield units; CT, computed tomography; UIV−1, one level below the uppermost instrumented vertebra; LIV+1, one level above the lowermost instrumented vertebra; LIV−1, one level below the lowermost instrumented vertebra
a Radiograph of an 18-year-old girl (group NR) with Lenke type 1 adolescent idiopathic scoliosis before surgery. b Radiograph 2 years after posterior spinal fusion using Cotrel–Dubousset instrumentation from T5 to L2. c Radiograph 21 years after initial surgery, demonstrating acceptable correction. d HU values of CT at the UIV−1, apex, LIV+1, and LIV−1 levels showing 169.9, 176.0, 185.5, and 218.1 HU, respectively. HU, Hounsfield units; CT, computed tomography; UIV−1, one level below the uppermost instrumented vertebra; LIV+1, one level above the lowermost instrumented vertebra; LIV−1, one level below the lowermost instrumented vertebra
Rights and permissions
About this article
Cite this article
Watanabe, K., Ohashi, M., Hirano, T. et al. Can posterior implant removal prevent device-related vertebral osteopenia after posterior fusion in adolescent idiopathic scoliosis? A mean 29-year follow-up study. Eur Spine J 28, 1314–1321 (2019). https://doi.org/10.1007/s00586-019-05921-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-05921-6