Abstract
The effect of biological (pollen) and chemical air pollutants on respiratory hospital admissions for the Szeged region in Southern Hungary is analysed. A 9-year (1999–2007) database includes—besides daily number of respiratory hospital admissions—daily mean concentrations of CO, PM10, NO, NO2, O3 and SO2. Two pollen variables (Ambrosia and total pollen excluding Ambrosia) are also included. The analysis was performed for patients with chronic respiratory complaints (allergic rhinitis or asthma bronchiale) for two age categories (adults and the elderly) of males and females. Factor analysis was performed to clarify the relative importance of the pollutant variables affecting respiratory complaints. Using selected low and high quantiles corresponding to probability distributions of respiratory hospital admissions, averages of two data sets of each air pollutant variable were evaluated. Elements of these data sets were chosen according to whether actual daily patient numbers were below or above their quantile value. A nonparametric regression technique was applied to discriminate between extreme and non-extreme numbers of respiratory admissions using pollen and chemical pollutants as explanatory variables. The strongest correlations between extreme patient numbers and pollutants can be observed during the pollen season of Ambrosia, while the pollen-free period exhibits the weakest relationships. The elderly group with asthma bronchiale is characterised by lower correlations between extreme patient numbers and pollutants compared to adults and allergic rhinitis, respectively. The ratio of the number of correct decisions on the exceedance of a quantile resulted in similar conclusions as those obtained by using multiple correlations.


Similar content being viewed by others
References
Ågren C (2010) Particles killing half a million. Acid News. AirClim. Air Pollution & Climate Secretariat, Sweden 2:1–5 http://www.airclim.org/acidnews/2010/AN2-10.php#1
Albertini R, Ugolotti M, Peveri S, Valenti MT, Usberti I, Ridolo E, Dall’Aglio P (2012) Evolution of ragweed pollen concentrations, sensitization and related allergic clinical symptoms in Parma (northern Italy). Aerobiologia 28:347–354. doi:10.1007/s10453-011-9239-6
Alves CA, Scotto MG, Freitas MC (2010) Air pollution and emergency admissions for cardiorespiratory diseases in Lisbon (Portugal). Quim Nova 33:337–344. doi:10.1590/S0100-40422010000200020
Andersen ZJ, Wahlin P, Raaschou-Nielsen O, Scheike T, Loft S (2007) Ambient particle source apportionment and daily hospital admissions among children and the elderly in Copenhagen. J Expo Sci Environ Epidemiol 17:625–636. doi:10.1038/sj.jes.7500546
Barrett K, de Leeuw F, Fiala J, Larssen S, Sundvor I, Fjellsbø L, Dusinska M, Ostatnická J, Horálek J, Černikovský L, Barmpas F, Moussipoulos N, Vlahocostas C (2008) Health impacts and air pollution – an exploration of factors influencing estimates of air pollution impact upon the health of European citizens. ETC/ACC Tech Pap 13
Bauer BA, Reed CE, Yunginger JW, Wollan PC, Silverstein MD (1997) Incidence and outcomes of asthma in the elderly—a population-based study in Rochester, Minnesota. Chest 111(2):303–310. doi:10.1378/chest.111.2.303
Carracedo-Martínez E, Sánchez C, Taracido M, Saez M, Jato V, Figueiras A (2008) Effect of short-term exposure to air pollution and pollen on medical emergency calls: a case-crossover study in Spain. Allergy 63:347–353. doi:10.1111/j.1398-9995.2007.01574.x
Cecchi L, D’Amato G, Ayres JG, Galán C, Forastiere F, Forsberg B, Gerritsen J, Nunes C, Behrendt H, Akdis C, Dahl R, Annesi-Maesano I (2010) Projections of the effects of climate change on allergic asthma: the contribution of aerobiology. Allergy 65:1073–1081. doi:10.1111/j.1398-9995.2010.02423.x
Chen CH, Xirasagar S, Lin HC (2006) Seasonality in adult asthma admissions, air pollutant levels, and climate: a population-based study. J Asthma 43:287–292. doi:10.1080/02770900600622935
Chiu HF, Cheng MH, Yang CY (2009) Air pollution and hospital admissions for pneumonia in a subtropical city: Taipei, Taiwan. Inhal Toxicol 21:32–37. doi:10.1080/08958370802441198
Chiusolo M, Cadum E, Stafoggia M, Galassi C, Berti G, Faustini A, Bisanti L, Vigotti MA, Dessi MP, Cernigliaro A, Mallone S, Pacelli B, Minerba S, Simonato L, Forastiere F (2011) Short-term effects of nitrogen dioxide on mortality and susceptibility factors in 10 Italian cities: the EpiAir study. Environ Health Perspect 119:1233–1238. doi:10.1289/ehp.1002904
Chung KAF, Zhang JF, Zhong NS (2011) Outdoor air pollution and respiratory health in Asia. Respirology 16:1023–1026. doi:10.1111/j.1440-1843.2011.02034.x
Cohen AJ, Anderson HR, Ostro B, Pandey KD, Krzyzanowski M, Künzli N, Gutschmidt K, Pope A, Romieu I, Samet JM, Smith K (2005) The global burden of disease due to outdoor air pollution. J Toxicol Environ Health A 68:1301–1307. doi:10.1080/15287390590936166
Darrow LA, Klein M, Sarnat JA, Mulholland JA, Strickland MJ, Sarnat SE, Russell AG, Tolbert PE (2011) The use of alternative pollutant metrics in time-series studies of ambient air pollution and respiratory emergency department visits. J Expo Sci Environ Epidemiol 21:10–19. doi:10.1038/jes.2009.49
Davies RJ, Rusznak C, Devalia JL (1998) Why is allergy increasing? Environmental factors. Clin Exp Allergy 28:8–14
Díaz J, Linares C, Tobías A (2007) Short-term effects of pollen species on hospital admissions in the city of Madrid in terms of specific causes and age. Aerobiologia 23:231–238. doi:10.1007/s10453-007-9067-x
Dullaers M, De Bruyne R, Ramadani F, Gould HJ, Gevaert P, Lambrecht BN (2012) The who, where, and when of IgE in allergic airway disease. J Allergy Clin Immunol 129:635–645. doi:10.1016/j.jaci.2011.10.029
Erkara I, Cingi C, Ayranci U, Gurbuz K, Pehlivan S, Tokur S (2009) Skin prick test reactivity in allergic rhinitis patients to airborne pollens. Environ Monit Assess 151:401–412. doi:10.1007/s10661-008-0284-8
Fan J, Yao Q (2005) Nonlinear time series: nonparametric and parametric methods. Springer, New York
Fischer G, Roppert J (1965) Ein Verfahren der Transformationsanalyse faktorenanalytischer Ergebnisse. In: Lineare Strukturen in Mathematik und Statistik unter besonderer Berücksichtigung der Faktoren- und Transformationsanalyse. Arbeiten aus dem Institut für höhere Studien und wissenschaftliche Forschung. Physica, Vienna
Freitas MC, Pacheco AMG, Verburg TG, Wolterbeek HAT (2010) Effect of particulate matter, atmospheric gases, temperature, and humidity on respiratory and circulatory diseases’ trends in Lisbon, Portugal. Environ Monit Assess 162:113–121. doi:10.1007/s10661-009-0780-5
Fusco D, Forastiere F, Michelozzi P, Spadea T, Ostro B, Arca M, Perucci CA (2001) Air pollution and hospital admissions for respiratory conditions in Rome, Italy. Eur Respir J 17:1143–1150. doi:10.1183/09031936.01.00005501
Galán C, Cariňanos P, García-Mozo H, Alcázar P, Domínguez-Vilches E (2001) Model for forecasting Olea europaea L. airborne pollen in South-West Andalusia, Spain. Int J Biometeorol 45:59–63. doi:10.1007/s004840100089
Giovannini M, Sala M, Riva E, Radaelli G (2010) Hospital admissions for respiratory conditions in children and outdoor air pollution in Southwest Milan, Italy. Acta Paediatr 99:1180–1185. doi:10.1111/j.1651-2227.2010.01786.x
Global Strategy for Asthma Management and Prevention (2010) 103 p http://www.ginasthma.org/pdf/GINA_Report_2010.pdf Accessed 6 August 2012
Global Strategy for Asthma Management and Prevention (2011) http://www.ginasthma.org/pdf/GINA_Report_2011.pdf
Gowers AM, Cullinan P, Ayres JG, Anderson HR, Strachan DP, Holgate ST, Mills IC, Maynard RL (2012) Does outdoor air pollution induce new cases of asthma? Biological plausibility and evidence; a review. Respirology 17:887–898. doi:10.1111/j.1440-1843.2012.02195.x
Hajat S, Anderson HR, Atkinson RW, Haines A (2002) Effects of air pollution on general practitioner consultations for upper respiratory diseases in London. Occup Environ Med 59:294–299. doi:10.1136/oem.59.5.294
Hanigan IC, Johnston FH (2007) Respiratory hospital admissions were associated with ambient airborne pollen in Darwin, Australia, 2004–2005. Clin Exp Allergy 37:1556–1565. doi:10.1111/j.1365-2222.2007.02800.x
Hirst JM (1952) An automatic volumetric spore trap. Ann Appl Biol 39:257–265
Jahn W, Vahle H (1968) Die Faktoranalyse und ihre Anwendung. Wirtschaft, Berlin
Járai-Komlódi M (1998) Ragweed in Hungary. In: (Spieksma FThM, ed.) Ragweed in Europe. Satellite Symposium Proceedings of 6th International Congress on Aerobiology. Perugia, Italy. Alk-Abelló, Horsholm, pp 33–38
Jeffery PK, Haahtela T (2006) Allergic rhinitis and asthma: inflammation in a one airway condition. BMC Pulm Med 6(Suppl 1):S5
Johnson ML (ed) (2005) The Cambridge handbook of age and ageing. Cambridge University Press, Cambridge
Jolliffe IT (1993) Principal component analysis: a beginner’s guide—II. Pitfalls, myths and extensions. Weather 48:246–253
Joseph PM (2007) Paradoxical ozone associations could be due to methyl nitrite from combustion of methyl ethers or esters in engine fuels. Environ Int 33:1090–1106. doi:10.1016/j.envint.2007.07.001
Joseph PM, Weiner MG (2002) Visits to physicians after the oxygenation of gasoline in Philadelphia. Arch Environ Health 57:137–154
Käpylä M, Penttinen A (1981) An evaluation of the microscopial counting methods of the tape in Hirst-Burkard pollen and spore trap. Grana 20:131–141. doi:10.1080/00173138109427653
Kassomenos P, Papaloukas C, Petrakis M, Karakitsios S (2008) Assessment and prediction of short term hospital admissions: the case of Athens, Greece. Atmos Environ 42:7078–7086. doi:10.1016/j.atmosenv.2008.06.011
Katsouyanni K, Zmirou D, Spix C (1996) Short-term effects of urban air pollution on health: a European approach using epidemiologic time series data. The APHEA protocol. J Epidemiol Commun H 5:S12–S18. doi:10.1136/jech.50.Suppl_1.S12
Kelly FJ, Fussell JC (2011) Air pollution and airway disease. Clin Exp Allergy 41:1059–1071. doi:10.1111/j.1365-2222.2011.03776.x
Kim BJ, Kwon JW, Seo JH, Kim HB, Lee SY, Park KS, Yu J, Kim HC, Leem JH, Sakong J, Kim SY, Lee CG, Kang DM, Ha M, Hong YC, Kwon HJ, Hong SJ (2011) Association of ozone exposure with asthma, allergic rhinitis, and allergic sensitization. Ann Allerg Asthma Im 107:214–219. doi:10.1016/j.anai.2011.05.025
Kiss L, Béres I (2006) Anthropogenic factors behind the recent population expansion of common ragweed (Ambrosia artemisiifolia L.) in Eastern Europe: is there a correlation with political transitions? J Biogeogr 33:2156–2157. doi:10.1111/j.1365-2699.2006.01633.x
Knight A, Drouin MA, Yang WH, Alexander M, Delcarpio J, Arnott WS (1991) clinical-evaluation of the efficacy and safety of noberastine, a new H1 antagonist, in seasonal allergic rhinitis—a placebo-controlled, dose–response study. J Allergy Clin Immun 88:926–934. doi:10.1016/0091-6749(91)90250-R
Ko FWS, Tam W, Wong TW, Lai CKW, Wong GWK, Leung TF, Ng SSS, Hui DSC (2007) Effects of air pollution on asthma hospitalisation rates in different age groups in Hong Kong. Clin Exp Allergy 37:1312–1319. doi:10.1111/j.1365-2222.2007.02791.x
Koppen G, Bloemen K, Colles A, Nelen V, Desager K, Schoeters G (2011) Exposure to traffic-related air pollutants in the perinatal period of life in relation to respiratory health in infancy. Crit Rev Environ Sci Technol 41:2003–2025. doi:10.1080/10643389.2010.495643
Kupczyk M, Wenzel S (2012) US and European severe asthma cohorts: what can they teach us about severe asthma? J Intern Med 272:121–132. doi:10.1111/j.1365-2796.2012.02558.x
Liu PWG (2009) Simulation of the daily average PM10 concentrations at Ta-Liao with Box-Jenkins time series models and multivariate analysis. Atmos Environ 43:2104–2113. doi:10.1016/j.atmosenv.2009.01.055
Magas OK, Gunter JT, Regens JL (2007) Ambient air pollution and daily pediatric hospitalizations for asthma. Environ Sci Pollut R 14:19–23. doi:10.1065/espr2006.08.333
Makra L, Juhász M, Béczi R, Borsos E (2005) The history and impacts of airborne Ambrosia (Asteraceae) pollen in Hungary. Grana 44:57–64. doi:10.1080/00173130510010558
Makra L, Matyasovszky I, Bálint B (2012) Association of allergic asthma emergency room visits with the main biological and chemical air pollutants. Sci Total Environ 432:288–296. doi:10.1016/j.scitotenv.2012.05.088
Martinez FD (2007) Genes, environments, development and asthma: a reappraisal. Eur Respir J 29:179–184. doi:10.1183/09031936.00087906
Miguel AG, Taylor PE, House J, Glovsky MM, Flagan RC (2006) Meteorological influences on respirable fragment release from Chinese elm pollen. Aerosol Sci Technol 40:690–696. doi:10.1080/02786820600798869
Miller RL, Ho SM (2008) Environmental epigenetics and asthma current concepts and call for studies. Am J Respir Crit Care Med 177:567–573. doi:10.1164/rccm.200710-1511PP
Namdeo A, Tiwary A, Farrow E (2011) Estimation of age-related vulnerability to air pollution: assessment of respiratory health at local scale. Environ Int 37:829–837. doi:10.1016/j.envint.2011.02.002
Nascimento LFC, Pereira LAA, Braga ALF, Modolo MCC, Carvalho JA (2006) Effects of air pollution on children’s health in a city in Southeastern Brazil. Rev Saude Publ 40:77–82
Nuvolone D, della Maggiore R, Maio S, Fresco R, Baldacci S, Carrozzi L, Pistelli F, Viegi G (2011) Geographical information system and environmental epidemiology: a cross-sectional spatial analysis of the effects of traffic-related air pollution on population respiratory health. Environ Health 10: Article No. 12 doi:10.1186/1476-069X-10-12
Orazzo F, Nespoli L, Ito K, Tassinari D, Giardina D, Funis M, Cecchi A, Trapani C, Forgeschi G, Vignini M, Nosetti L, Pigna S, Zanobetti A (2009) Air pollution, aeroallergens, and emergency room visits for acute respiratory diseases and gastroenteric disorders among young children in six Italian cities. Environ Health Perspect 117:1780–1785. doi:10.1289/ehp.0900599
Peternel R, Culig J, Hrga I, Hercog P (2006) Airborne ragweed (Ambrosia artemisiifolia L.) pollen concentrations in Croatia, 2002–2004. Aerobiologia 22:161–168. doi:10.1007/s10453-006-9028-9
Rogers CA, Wayne PM, Macklin EA, Muilenberg ML, Wagner CJ, Epstein PR, Bazzaz FA (2006) Interaction of the onset of spring and elevated atmospheric CO2 on ragweed (Ambrosia artemisiifolia L.) pollen production. Environ Health Perspect 114:865–869. doi:10.1289/ehp.8549
Sacks JD, Stanek LW, Luben TJ, Johns DO, Buckley BJ, Brown JS, Ross M (2011) Particulate matter-induced health effects: who is susceptible? Environ Health Perspect 119:446–454. doi:10.1289/ehp.1002255
Tramuto F, Cusimano R, Cerame G, Vultaggio M, Calamusa G, Maida CM, Vitale F (2011) Urban air pollution and emergency room admissions for respiratory symptoms: a case-crossover study in Palermo, Italy. Environ Health 10: Article No. 31 doi:10.1186/1476-069X-10-31
World Health Organization (1992) Acute effects on health of smog episodes. WHO Regional Publications, European Series, 43 WHO Regional Office for Europe, Geneva
World Health Organization (1999) Manual of the international statistical classification of diseases, injuries, and causes of death, 10th revision. World Health Organization, Geneva
Zhang F, Wang W, Lv J, Krafft T, Xu J (2011) Time-series studies on air pollution and daily outpatient visits for allergic rhinitis in Beijing, China. Sci Total Environ 409:2486–2492. doi:10.1016/j.scitotenv.2011.04.007
Ziello C, Sparks TH, Estrella N, Belmonte J, Bergmann KC, Bucher E, Brighetti MA, Damialis A, Detandt M, Galan C, Gehrig R, Grewling L, Bustillo AMG, Hallsdottir M, Kockhans-Bieda MC, De Linares C, Myszkowska D, Paldy A, Sanchez A, Smith M, Thibaudon M, Travaglini A, Uruska A, Valencia-Barrera RM, Vokou D, Wachter R, de Weger LA, Menzel A (2012) Changes to airborne pollen counts across Europe. Plos One 7: Article No. e34076 doi:10.1371/journal.pone.0034076
Zimmerman DW (1997) A note on interpretation of the paired-samples t test. J Educ Behav Stat 22:349–360. doi:10.3102/10769986022003349
Ziska LH, Caulfield FA (2000) Rising CO2 and pollen production of common ragweed (Ambrosia artemisiifolia), a known allergy-inducing species: implications for public health. Aust J Plant Physiol 27:893–898
Ziska LH, George K, Frenz DA (2007) Establishment and persistence of common ragweed (Ambrosia artemisiifolia) in disturbed soil as a function of an urban-rural macro-environment. Glob Change Biol 13:266–274. doi:10.1111/1365-2486.2006.01264.x
Acknowledgements
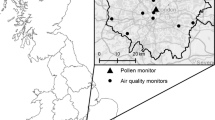
The authors would like to thank Gábor Motika (Environmental Conservancy Inspectorate, Szeged, Hungary) for providing chemical air pollutant data of Szeged, Miklós Juhász (University of Szeged) for providing pollen data of Szeged and Zoltán Sümeghy (University of Szeged) for the digital mapping in Fig. 1. The authors gratefully acknowledge the anonymous reviewers for their constructive comments, advice and suggestions. The European Union and the European Social Fund provided financial support for the project under the grant agreement no. TAMOP 4.2.1/B-09/1/KMR-2010-0003, TAMOP-4.2.1/B-09/1/KONV-2010-0005 and TAMOP-4.2.2/B-10/1-2010-0012.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Makra, L., Matyasovszky, I., Bálint, B. et al. Association of allergic rhinitis or asthma with pollen and chemical pollutants in Szeged, Hungary, 1999–2007. Int J Biometeorol 58, 753–768 (2014). https://doi.org/10.1007/s00484-013-0656-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-013-0656-9