Abstract
Background
In intensive care units (ICUs), antiepileptic drugs (AEDs) are used for manifold indications. This is the first study to assess the prevalence of acute AED use in ICUs and to identify associated clinical variables.
Methods
All patients in seven adult ICUs of a German university hospital in 2016 were retrospectively evaluated. Data were extracted from the computerized critical care information system and manually reviewed. Acute AED treatments were defined as initiated during ICU treatment or ≤ 6 h before ICU admission, excluding benzodiazepines and sedatives.
Results
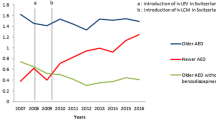
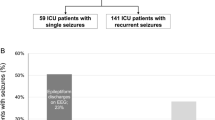
Among 2335 patients evaluated, 8.8% received acutely started AEDs: 5.1% due to epileptic seizures, mostly acute symptomatic, and 3.7% for other indications like pain, post-hypoxic myoclonus, and singultus. Following multivariable analyses, acute AED use was independently associated with intracranial reasons for ICU admission and long durations of ICU stay, but not with increased disease severity scores or mortality. Levetiracetam was the substance most frequently used to treat epileptic seizures (88%) as was pregabalin for other conditions (49%). Among surviving patients, acute AEDs were continued beyond ICU discharge in 86% if seizure-related and in 78% if not seizure-related, even if there was no evident need for long-term AED treatment.
Conclusions
One out of eleven ICU patients receives acute AEDs, in almost half of cases for non-seizure indications. Acute AED use is a marker for intracranial ICU indications and prolonged ICU treatments. Usually, newer-generation AEDs are employed with favourable pharmacokinetic and safety profiles. However, whenever possible, acutely started AED should be discontinued before discharge from ICU.


Similar content being viewed by others
References
Wiffen PJ, Derry S, Moore RA, Aldington D, Cole P, Rice AS, Lunn MP, Hamunen K, Haanpaa M, Kalso EA (2013) Antiepileptic drugs for neuropathic pain and fibromyalgia—an overview of cochrane reviews. Cochrane Database Syst Rev 11:CD010567
Ettinger AB, Argoff CE (2007) Use of antiepileptic drugs for nonepileptic conditions: psychiatric disorders and chronic pain. Neurotherapeutics 4:75–83
Beghi E, D’Alessandro R, Beretta S, Consoli D, Crespi V, Delaj L, Gandolfo C, Greco G, La NA, Manfredi M, Mattana F, Musolino R, Provinciali L, Santangelo M, Specchio LM, Zaccara G (2011) Incidence and predictors of acute symptomatic seizures after stroke. Neurology 77:1785–1793
Ritter AC, Wagner AK, Fabio A, Pugh MJ, Walker WC, Szaflarski JP, Zafonte RD, Brown AW, Hammond FM, Bushnik T, Johnson-Greene D, Shea T, Krellman JW, Rosenthal JA, Dreer LE (2016) Incidence and risk factors of posttraumatic seizures following traumatic brain injury: a traumatic brain injury model systems study. Epilepsia 57:1968–1977
Kim MA, Park KM, Kim SE, Oh MK (2008) Acute symptomatic seizures in CNS infection. Eur J Neurol 15:38–41
Beghi E, Carpio A, Forsgren L, Hesdorffer DC, Malmgren K, Sander JW, Tomson T, Hauser WA (2010) Recommendation for a definition of acute symptomatic seizure. Epilepsia 51:671–675
Karceski S (2014) Acute symptomatic seizures and systemic illness. Continuum (Minneap Minn) 20:614–623
Dahl JB, Nielsen RV, Wetterslev J, Nikolajsen L, Hamunen K, Kontinen VK, Hansen MS, Kjer JJ, Mathiesen O (2014) Post-operative analgesic effects of paracetamol, NSAIDs, glucocorticoids, gabapentinoids and their combinations: a topical review. Acta Anaesthesiol Scand 58:1165–1181
Polito NB, Fellows SE (2017) Pharmacologic interventions for intractable and persistent hiccups: a systematic review. J Emerg Med 53:540–549
Aicua R, Novy I, Solari J, Oddo D, Rossetti M AO (2017) Early Lance-Adams syndrome after cardiac arrest: prevalence, time to return to awareness, and outcome in a large cohort. Resuscitation 115:169–172
Perucca P, Gilliam FG (2012) Adverse effects of antiepileptic drugs. Lancet Neurol 11:792–802
Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13:818–829
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Miranda DR, de RA, Schaufeli W (1996) Simplified therapeutic intervention scoring system: the TISS-28 items—results from a multicenter study. Crit Care Med 24:64–73
Waskom M Seaborn: statistical data visualization. https://seaborn.pydata.org/#. Accessed 09 July 2018
d3noob Sankey diagram from formatted JSON. https://gist.github.com/d3noob/c2637e28b79fb3bfea13. Accessed 31 May 2018
The Federal Health Monitoring System Intensive care in hospitals (beds) and stays (cases and occupancy/billing days). Classification: years, region, facility features. http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=i&p_aid=17242324&nummer=841&p_sprache=E&p_indsp=27980598&p_aid=9260741. Accessed 07 May 2018
Crepeau AZ, Treiman DM (2010) Levetiracetam: a comprehensive review. Expert Rev Neurother 10:159–171
Lang N, Esser W, Evers S, Kellinghaus C, Nguento A, Schlegel U, Gaida B, Gburek-Augustat J, Altenmuller DM, Burghaus L, Hoffmann F, Fiedler B, Bast T, Rehfeld T, Happe S, Seitz RJ, Boor R, Stephani U (2015) Intravenous levetiracetam in clinical practice—results from an independent registry. Seizure 29:109–113
Verrotti A, Prezioso G, Di SF, Franco V, Chiarelli F, Zaccara G (2015) The adverse event profile of levetiracetam: a meta-analysis on children and adults. Seizure 31:49–55
The Federal Health Monitoring System Generic drugs prescribed at the expense of the statutory health insurance (total prescriptions in thousand packages and in percent, total sales in million € and in percent). Classification: years, Germany, active pharmaceutical ingredient. http://www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=33558202&nummer=356&p_sprache=E&p_indsp=-&p_aid=39142848. Accessed 25 June 2018
Kellinghaus C, Stogbauer F (2012) Treatment of status epilepticus in a large community hospital. Epilepsy Behav 23:235–240
Kortland LM, Alfter A, Bahr O, Carl B, Dodel R, Freiman TM, Hubert K, Jahnke K, Knake S, von Reese PF, Runge JP, Senft U, Steinmetz C, Rosenow H, Strzelczyk FA (2016) Costs and cost-driving factors for acute treatment of adults with status epilepticus: a multicenter cohort study from Germany. Epilepsia 57:2056–2066
European Medicines Agency European Public Assessment Report for Lyrica. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000546/human_med_000894.jsp&mid=WC0b01ac058001d124. Accessed 01 June 2018
Mishriky BM, Waldron NH, Habib AS (2015) Impact of pregabalin on acute and persistent postoperative pain: a systematic review and meta-analysis. Br J Anaesth 114:10–31
Zaccara G, Perucca P, Gangemi PF (2012) The adverse event profile of pregabalin across different disorders: a meta-analysis. Eur J Clin Pharmacol 68:903–912
Boldt J, Haisch G (2000) The situation of intensive care in Germany—results of a questionnaire. Intensivmed 37:195–205
Hesdorffer DC, Benn EK, Cascino GD, Hauser WA (2009) Is a first acute symptomatic seizure epilepsy? Mortality and risk for recurrent seizure. Epilepsia 50:1102–1108
Holtkamp M, Beghi E, Benninger F, Kälviäinen R, Rocamora R, Christensen H (2017) European Stroke Organisation guidelines for the management of post-stroke seizures and epilepsy. Eur Stroke J 2:103–115
Acknowledgements
BV was funded by a grant of the von Bodelschwingh Foundation. MH holds the ‘Friedrich-von-Bodelschwingh Endowed Professorship for Clinical and Experimental Epileptology’ at the Department of Neurology, Charité–Universitätsmedizin Berlin. The authors wish to thank Dr Gerald Vorderwülbecke for designing Fig. 2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
BJV, GL, and FvD declare that they have no conflict of interest. MH received speaker’s honoraria and/or consultancy fees from Bial, Desitin, Eisai, LivaNova, Novartis, and UCB.
Ethical standards
The study was approved by the institutional research committee at Charité–Universitätsmedizin Berlin. All procedures were in accordance with the ethical standards laid down in the 1964 Helsinki declaration and its later amendments. For this retrospective study, formal consent was not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vorderwülbecke, B.J., Lichtner, G., von Dincklage, F. et al. Acute antiepileptic drug use in intensive care units. J Neurol 265, 2841–2850 (2018). https://doi.org/10.1007/s00415-018-9069-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-9069-3