Abstract
Introduction
The differentiation between stiff-knee and low-grade periprosthetic joint infection (PJI) is the current diagnostic challenge in total knee (TKA) revision arthroplasty. The aim of this study was to investigate the additional value of dry biopsies, compared to wet biopsies, in patients presenting with knee stiffness following primary TKA.
Materials and methods
Single center, prospective observational study. Consecutive patients with joint stiffness of unknown origin following primary TKA were enrolled. Patient assessment followed the diagnostic standard algorithm. During diagnostic arthroscopy, synovial fluid (synovial WBC, PMN%) and five dry biopsies (dry) were collected. Then fluid was infused and another five microbiology (wet) and five histological biopsies gathered, all from identical locations. The primary outcome parameter was the difference between the pathogens in wet and dry biopsies.
Results
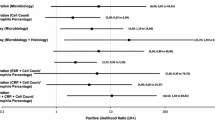
71 patients (61% females, 67 ± 10 years) were eligible. Preoperative blood serology mean CRP (0.7 ± 1.5 mg/dl; p = 0.852), WBC (6.6 ± 1.7 G/l; p = 0.056), and synovial fluid mean WBC (1639 ± 2111; p = 0.602), PMN% (38 ± 28; p = 0.738) did not differ between patients with negative, positive wet or dry biopsies. The histology was in 11% positive (p = 0.058). In 32% at least one pathogen was detected, 48% from wet, 44% from dry biopsies. An inhomogeneous distribution was found. Cutibacterium acnes (100%) was solely found in wet, Micrococcus luteus (75%), Staphylococcus capitis (67%), and Micrococcus lylae (100%) were predominantly found in dry biopsies. Additional dry biopsies increased the pathogen detection rate by 49%.
Conclusion
The addition of dry biopsies to the current standard diagnostic algorithm for PJI increased the pathogen detection rate by 49%.

Similar content being viewed by others
References
Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, Shohat N (2018) The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplast 33(5):1309.e2–1314.e2. https://doi.org/10.1016/j.arth.2018.02.078
Djahani O, Rainer S, Pietsch M, Hofmann S (2013) Systematic analysis of painful total knee prosthesis, a diagnostic algorithm. Arch Bone Jt Surg 1(2):48–52. https://doi.org/10.1136/gutjnl-2017-315384
Park CN, White PB, Meftah M, Ranawat AS, Ranawat CS (2016) Diagnostic algorithm for residual pain after total knee arthroplasty. Orthopedics 39(2):e246–e252. https://doi.org/10.3928/01477447-20160119-06
Esposito CI (2017) CORR Insights®: periprosthetic joint infection is the main cause of failure for modern knee arthroplasty: an analysis of 11,134 knees. Clin Orthop Relat Res 475(9):2202–2204. https://doi.org/10.1007/s11999-017-5436-0
Koh IJ, Cho W-S, Choi NY, Kim TK, Group KKR (2014) Causes, risk factors, and trends in failures after TKA in Korea over the past 5 years: a multicenter study. Clin Orthop Relat Res 472(1):316–326. https://doi.org/10.1007/s11999-013-3252-8
Kanwar S, Al-Mansoori AA, Chand MR, Villa JM, Suarez JC, Patel PD (2018) What is the optimal criteria to use for detecting periprosthetic joint infections before total joint arthroplasty? J Arthroplast. https://doi.org/10.1016/j.arth.2018.02.072
Grau L, Gunder MA, Schneiderbauer M (2017) Difficult-to-detect low-grade infections responsible for poor outcomes in total knee arthroplasty. Am J Orthop (Belle Mead NJ) 46(3):E148–E153
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG (2011) New definition for periprosthetic joint infection: from the workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469(11):2992–2994. https://doi.org/10.1007/s11999-011-2102-9
Parvizi J, Gehrke T, Chen AF (2013) Proceedings of the international consensus on periprosthetic joint infection. Bone Jt J 95-B(11):1450–1452. https://doi.org/10.1302/0301-620X.95B11.33135
Cats-Baril W, Gehrke T, Huff K, Kendoff D, Maltenfort M, Parvizi J (2013) International consensus on periprosthetic joint infection: description of the consensus process. Clin Orthop Relat Res 471(12):4065–4075. https://doi.org/10.1007/s11999-013-3329-4
Della Valle C, Parvizi J, Bauer TW, DiCesare PE, Evans RP, Segreti J, Spangehl M, Watters WC, Keith M, Turkelson CM, Wies JL, Sluka P, Hitchcock K, Surgeons AAoO (2011) American Academy of Orthopaedic Surgeons clinical practice guideline on: the diagnosis of periprosthetic joint infections of the hip and knee. J Bone Jt Surg Am 93(14):1355–1357. https://doi.org/10.2106/JBJS.9314ebo
Parvizi J, Jacovides C, Antoci V, Ghanem E (2011) Diagnosis of periprosthetic joint infection: the utility of a simple yet unappreciated enzyme. J Bone Jt Surg Am 93(24):2242–2248. https://doi.org/10.2106/JBJS.J.01413
Massin P, Delory T, Lhotellier L, Pasquier G, Roche O, Cazenave A, Estellat C, Jenny JY (2016) Infection recurrence factors in one- and two-stage total knee prosthesis exchanges. Knee Surg Sports Traumatol Arthrosc 24(10):3131–3139. https://doi.org/10.1007/s00167-015-3884-1
George DA, Haddad FS (2017) One-stage exchange arthroplasty: a surgical technique update. J Arthroplast 32(9S):S59–S62. https://doi.org/10.1016/j.arth.2017.02.025
Cury RdPL, Cinagawa EHT, Camargo OPA, Honda EK, Klautau GB, Salles MJC (2015) Treatment of infection after total knee arthroplasty. Acta Ortop Bras 23(5):239–243. https://doi.org/10.1590/1413-785220152305138774
Nagra NS, Hamilton TW, Ganatra S, Murray DW, Pandit H (2016) One-stage versus two-stage exchange arthroplasty for infected total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 24(10):3106–3114. https://doi.org/10.1007/s00167-015-3780-8
Trampuz A, Zimmerli W (2005) Prosthetic joint infections: update in diagnosis and treatment. Swiss Med Wkly 135(17–18):243–251
Pandey R, Berendt AR, Athanasou NA (2000) Histological and microbiological findings in non-infected and infected revision arthroplasty tissues. The OSIRIS Collaborative Study Group. Oxford skeletal infection research and intervention service. Arch Orthop Trauma Surg 120(10):570–574
Dramis A, Aldlyami E, Grimer RJ, Dunlop DJ, O’Connell N, Elliott T (2009) What is the significance of a positive Propionibacterium acnes culture around a joint replacement? Int Orthop 33(3):829–833. https://doi.org/10.1007/s00264-008-0534-y
Balato G, Franceschini V, Ascione T, Lamberti A, Balboni F, Baldini A (2018) Diagnostic accuracy of synovial fluid, blood markers, and microbiological testing in chronic knee prosthetic infections. Arch Orthop Trauma Surg 138(2):165–171. https://doi.org/10.1007/s00402-017-2832-6
Baré J, MacDonald SJ, Bourne RB (2006) Preoperative evaluations in revision total knee arthroplasty. Clin Orthop Relat Res 446:40–44. https://doi.org/10.1097/01.blo.0000218727.14097.d5
Rothenberg AC, Wilson AE, Hayes JP, O’Malley MJ, Klatt BA (2017) Sonication of arthroplasty implants improves accuracy of periprosthetic joint infection cultures. Clin Orthop Relat Res 475(7):1827–1836. https://doi.org/10.1007/s11999-017-5315-8
Melendez DP, Greenwood-Quaintance KE, Berbari EF, Osmon DR, Mandrekar JN, Hanssen AD, Patel R (2016) Evaluation of a genus- and group-specific rapid PCR assay panel on synovial fluid for diagnosis of prosthetic knee infection. J Clin Microbiol 54(1):120–126. https://doi.org/10.1128/JCM.02302-15
de Saint Vincent B, Migaud H, Senneville E, Loiez C, Pasquier G, Girard J, Putman S (2018) Diagnostic accuracy of the alpha defensin lateral flow device (Synovasure™) for periprosthetic infections in microbiologically complex situations: a study of 42 cases in a French referral centre. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2018.01.018
Trampuz A, Piper KE, Jacobson MJ, Hanssen AD, Unni KK, Osmon DR, Mandrekar JN, Cockerill FR, Steckelberg JM, Greenleaf JF, Patel R (2007) Sonication of removed hip and knee prostheses for diagnosis of infection. N Engl J Med 357(7):654–663. https://doi.org/10.1056/NEJMoa061588
Volpe L, Indelli PF, Latella L, Poli P, Yakupoglu J, Marcucci M (2014) Periprosthetic joint infections: a clinical practice algorithm. Joints 2(4):169–174
McDowell M, Park A, Gerlinger TL (2016) The painful total knee arthroplasty. Orthop Clin N Am 47(2):317–326. https://doi.org/10.1016/j.ocl.2015.09.008
Fink B, Schäfer P, Frommelt L (2012) Logistic requirements and biopsy of periprosthetic infections: what should be taken into consideration?. Der Orthopäde 41(1):15–19. https://doi.org/10.1007/s00132-011-1836-0
Fuerst M, Fink B, Rüther W (2005) The value of preoperative knee aspiration and arthroscopic biopsy in revision total knee arthroplasty. Z Orthop Ihre Grenzgeb 143(1):36–41. https://doi.org/10.1055/s-2004-836252
Kalson NS, Borthwick LA, Mann DA, Deehan DJ, Lewis P, Mann C, Mont MA, Morgan-Jones R, Oussedik S, Williams FM, Toms A, Argenson JN, Bellemans J, Bhave A, Furnes O, Gollwitzer H, Haddad FS, Hofmann S, Krenn V (2016) International consensus on the definition and classification of fibrosis of the knee joint. Bone Jt J 98-B(11):1479–1488. https://doi.org/10.1302/0301-620X.98B10.37957
Mont MA, Waldman BJ, Hungerford DS (2000) Evaluation of preoperative cultures before second-stage reimplantation of a total knee prosthesis complicated by infection. A comparison-group study. J Bone Jt Surg Am 82-A(11):1552–1557
Burnett RSJ, Kelly MA, Hanssen AD, Barrack RL (2007) Technique and timing of two-stage exchange for infection in TKA. Clin Orthop Relat Res 464:164–178. https://doi.org/10.1097/BLO.0b013e318157eb1e
Math KR, Zaidi SF, Petchprapa C, Harwin SF (2006) Imaging of total knee arthroplasty. Semin Musculoskelet Radiol 10(1):47–63. https://doi.org/10.1055/s-2006-934216
Claaßen L, Ettinger S, Pastor M-F, Budde S, Windhagen H, Floerkemeier T (2016) The value of arthroscopic neosynovium biopsies to diagnose periprosthetic knee joint low-grade infection. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-016-2574-x
Fink B, Makowiak C, Fuerst M, Berger I, Schäfer P, Frommelt L (2008) The value of synovial biopsy, joint aspiration and C-reactive protein in the diagnosis of late peri-prosthetic infection of total knee replacements. J Bone Jt Surg Br 90(7):874–878. https://doi.org/10.1302/0301-620X.90B7.20417
Trampuz A, Hanssen AD, Osmon DR, Mandrekar J, Steckelberg JM, Patel R (2004) Synovial fluid leukocyte count and differential for the diagnosis of prosthetic knee infection. Am J Med 117(8):556–562. https://doi.org/10.1016/j.amjmed.2004.06.022
Chalmers PN, Walton D, Sporer SM, Levine BR (2015) Evaluation of the role for synovial aspiration in the diagnosis of aseptic loosening after total knee arthroplasty. J Bone Jt Surg Am 97(19):1597–1603. https://doi.org/10.2106/JBJS.N.01249
Della Valle CJ, Sporer SM, Jacobs JJ, Berger RA, Rosenberg AG, Paprosky WG (2007) Preoperative testing for sepsis before revision total knee arthroplasty. J Arthroplast 22(6 Suppl 2):90–93. https://doi.org/10.1016/j.arth.2007.04.013
Ghanem E, Antoci V Jr, Pulido L, Joshi A, Hozack W, Parvizi J (2009) The use of receiver operating characteristics analysis in determining erythrocyte sedimentation rate and C-reactive protein levels in diagnosing periprosthetic infection prior to revision total hip arthroplasty. Int J Infect Dis 13(6):e444–e449. https://doi.org/10.1016/j.ijid.2009.02.017
Ghanem E, Parvizi J, Burnett RSJ, Sharkey PF, Keshavarzi N, Aggarwal A, Barrack RL (2008) Cell count and differential of aspirated fluid in the diagnosis of infection at the site of total knee arthroplasty. J Bone Jt Surg Am 90(8):1637–1643. https://doi.org/10.2106/JBJS.G.00470
McArthur BA, Abdel MP, Taunton MJ, Osmon DR, Hanssen AD (2015) Seronegative infections in hip and knee arthroplasty: periprosthetic infections with normal erythrocyte sedimentation rate and C-reactive protein level. Bone Jt J 97-B(7):939–944. https://doi.org/10.1302/0301-620X.97B7.35500
Allum R (2002) Complications of arthroscopy of the knee. J Bone Jt Surg Br 84(7):937–945
Aggarwal VK, Bakhshi H, Ecker NU, Parvizi J, Gehrke T, Kendoff D (2014) Organism profile in periprosthetic joint infection: pathogens differ at two arthroplasty infection referral centers in Europe and in the United States. J Knee 27(5):399–406. https://doi.org/10.1055/s-0033-1364102
Holleyman RJ, Baker P, Charlett A, Gould K, Deehan DJ (2016) Microorganisms responsible for periprosthetic knee infections in England and Wales. Knee Surg Sports Traumatol Arthrosc 24(10):3080–3087. https://doi.org/10.1007/s00167-015-3539-2
Corvec S, Portillo ME, Pasticci BM, Borens O, Trampuz A (2012) Epidemiology and new developments in the diagnosis of prosthetic joint infection. Int J Artif Org 35(10):923–934. https://doi.org/10.5301/ijao.5000168
Malhas AM, Lawton R, Reidy M, Nathwani D, Clift BA (2015) Causative organisms in revision total hip and knee arthroplasty for infection: Increasing multi-antibiotic resistance in coagulase-negative Staphylococcus and the implications for antibiotic prophylaxis. Surgeon 13(5):250–255. https://doi.org/10.1016/j.surge.2014.04.002
Martinez-Pastor JC (2013) Acute infection in total knee arthroplasty: diagnosis and treatment. Open Orthop J 7(1):197–204. https://doi.org/10.2174/1874325001307010197
Ahmad SS, Shaker A, Saffarini M, Chen AF, Hirschmann MT, Kohl S (2016) Accuracy of diagnostic tests for prosthetic joint infection: a systematic review. Knee Surg Sports Traumatol Arthrosc 24(10):3064–3074. https://doi.org/10.1007/s00167-016-4230-y
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baumbach, S.F., Prall, W.C., Scharpf, A.M. et al. Significant increase of pathogen detection rate by dry arthroscopic biopsies at suspected low-grade infection following total knee arthroplasty: a prospective observational study. Arch Orthop Trauma Surg 138, 1583–1590 (2018). https://doi.org/10.1007/s00402-018-3032-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3032-8