Abstract
Introduction
In revision total hip arthroplasty (THA), the cancellous bone is normally completely removed out of the femoral canal during stem extraction. This situation is comparable to primary THA following the shape-closed concept, with some authors advocating to remove the metaphyseal cancellous bone to enhance press-fit stability (“French paradox”). The aim of this study was to investigate the long-term outcome, regarding survival and radiological results, of a cemented straight stem when used for revision THA and to compare these results to the results of the same stem in primary THA.
Materials and methods
178 stem revisions performed between 01/1994 and 08/2008 using the Virtec straight stem were included. The cumulative incidence for re-revision was calculated using a competing risk model. Risk factors for re-revision of the stem were analyzed using an absolute risk regression model. Radiographs analyzed for osteolysis, debonding and subsidence had a minimum follow-up of 10 years.
Results
The cumulative incidence for re-revision due to aseptic loosening of the stem was 5.5% (95% CI, 2.9–10.2%) at 10 years. Aseptic loosening was associated with younger age, larger defect size and larger stem size. After a minimum 10-year follow-up, osteolysis was seen in 39 of 80 revision THA. Compared to the results in primary THA, the survival in revision THA with the same implant was inferior.
Conclusions
Cemented straight stems used for revision THA showed excellent long-term results regarding survivorship and radiological outcome. This stem therefore offers a valuable and cost-effective option in revision THA.
Similar content being viewed by others
Introduction
Revision total hip arthroplasty (THA) is a continuously increasing procedure in orthopedic surgery [1, 2]. Like in primary THA, stability of components can be achieved with or without bone cement. Using uncemented revision implants on the femoral side has become more and more popular. They show excellent long-term results even in patients who have poor femoral bone stock [3]. However, a potential disadvantage of uncemented revision stems is the partial weight bearing allowed in the immediate postoperative period to prevent excessive stem subsidence, especially when using a transfemoral approach [4, 5]. This disadvantage of uncemented stems can be bypassed when using cemented femoral revision stems, where immediate postoperative weight bearing is always possible.
In the literature, long-term results of cemented femoral revision using impaction bone grafting have shown excellent long-term survival [6, 7]. However, this technique is demanding and the periprosthetic fracture rate is reported to be high [8]. Furthermore, it is expensive to keep a bone bank or to buy lyophilized allograft bone chips.
In primary-cemented THA, there are two main basic theoretical design principles for stem fixation: shape-closed/composite beam, and force-closed/loaded taper [9]. For force-closed fixation, an undersized implant is inserted and surrounded by a complete, thick cement mantle while for shape-closed fixation, the largest implant possible is inserted leaving only a thin and/or incomplete cement mantle. The latter technique is also known as “French paradox” [10]. In this concept, the resulting press-fit to the cortical bone enhances the fixation of the stem [11]. Some authors even advocate the removal of cancellous bone using a curette to even further enhance the press-fit stability of the stem [12] with excellent long-term results [13]. This situation is comparable to the situation found in revision THA, where cancellous bone as well as all granulation tissue is normally completely removed out of the femoral canal during stem extraction. Up to now, only sparse knowledge exists on using a shape-closed stem in cemented femoral revision arthroplasty.
The aim of the present study was (1) to investigate the long-term outcome regarding survivorship and radiological results of a cemented straight stem using the shape-closed concept in revision THA and (2) to compare these results to data of the same stem used in primary THA.
Patients and methods
This is an observational, single-center study which is based on prospectively collected data of a consecutive series of patients.
Implants and patients
The Virtec straight stem (Zimmer, Winterthur, Switzerland) is a variant of the Müller straight stem. The stem is double-tapered, has an oval cross section and is made of CoNiCrMo [14]. The design rationale was, analogous to the Kerboull stem [12], to provide better filling of the proximal femur when compared to the original Müller straight stem [14]. Various sizes in standard and lateral versions are available. In the first period of this study, the PF stem (Cedior, Montbéliard, France) with the same shape, however, manufactured out of stainless steel, was used. As results did not differ between the two implants, no differentiation was made for further evaluation (data not shown).
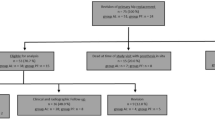
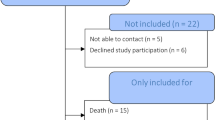
All 172 patients (178 hips) who underwent revision with the PF or Virtec straight stem between 01/1994 and 08/2006 were included. Ethics committee approval was obtained prior to study commencement. The mean age (standard deviation) of the patients at the time of the surgery was 68.4 (9.3) years (range 36–90 years); 126 (71%) cases were male. Indication for revision was aseptic loosening in 137 cases (77%), periprosthetic joint infection (PJI) in 32 cases (18%), malposition of the stem in 6 cases (3.4%), and a broken implant in 3 cases (1.7%). The type of explanted stems are listed and femoral defects prior to replantation classified according to Della Valle and Paprosky [15] shown in Table 1. 116 cases received their primary implantation in our hospital, 62 cases were referred to us from another hospital. A total of 19 cases had at least one previous revision.
A revision of the acetabular component was performed in 82 out of 178 cases. In 61 cases, a cemented Mueller acetabular reinforcement ring was implanted, in 11 cases, a non-cemented SL-cup, and in 10 cases, a Burch-Schneider anti-protrusio cage (all Zimmer, Winterthur, Switzerland).
Surgical technique
Every revision surgery was standardized using a lateral transgluteal approach with the patient in a supine position. After stem removal, the medullary canal was cleaned using drills and chisels to remove all cement remnants; granulation tissue was completely removed using specially designed curettes (Fig. 1). Thereafter, the medullary canal was repeatedly rinsed with a 0.2% polyhexanide solution (Lavasept®, B. Braun, Melsungen, Germany) using a bulb syringe. Subsequently, the largest implant fitting into the medullary canal was implanted, aiming for a primary press-fit fixation in the anterior–posterior (ap) plane (Table 2). Implants were cemented line-to-line with the final broach [16]. All stems where implanted with a second-generation cementing technique (no vacuum mixing, distal plug, retrograde filling) using high-viscosity Palacos R + G (Heraeus, Hanau, Germany) cement [17]. In case of septic loosening, patients were treated according to our established algorithm either with a 1-stage (14 cases) or 2-stage revision (18 cases) [18]. No additional antibiotics were added to the cement in any cases. The postoperative mobilization was the same for all patients with initial full weight bearing as tolerated starting the first postoperative day.
Follow-up
Follow-up examinations were scheduled at 4 months, 1 year, 2 years, and 5 years, and all 5 years thereafter. Patients were rated as lost to follow-up when last contact (outpatient clinic or telephone call) was 5 years overdue. For radiological analysis, the first postoperative radiograph and the most recent radiograph of all unrevised patients with a minimum radiological follow-up of > 10 years or in case of a revision, the last radiograph prior to revision, were analyzed. Standardized AP radiographs were taken centered on the symphysis, showing the entire implant. Findings were stratified according to the Gruen zone system [19]. Osteolysis was defined as any newly developed progressive endosteal bone loss at the cement–bone interface with a diameter > 3 mm and categorized as either scallop- or bead-shaped [20]. Axial subsidence of the stem was measured as an increase of any radiolucency in the proximal cement in Gruen zone 1, created due to distal migration of the shoulder of the prosthesis. It was considered relevant if it was more than 2 mm [21]. Debonding was defined as present, if a radiolucent line at the prosthesis–cement interface, not visible on the first postoperative radiograph, was observed [22]. The stem was rated as being radiologically loose if circumferential radiolucency in all Gruen zones [23] and/or excessive subsidence of more than 10 mm [14] was present. The radiological analysis was carried out by one of the first authors at the end of the study; ambiguous findings were discussed with the senior investigator and agreed upon.
Statistics
A survival analysis with death as a competing risk was performed with various endpoints: (1) aseptic loosening of the stem, (2) worst-case scenario with all cases lost to follow-up judged as aseptic loosening, and (3) re-revision of the stem and/or cup (including exchange of the liner) for any reason. Patients without any re-revision were censored at the date of last contact. For each endpoint, cumulative incidence functions were used. Furthermore, time to aseptic loosening of the stem was analyzed using an absolute risk regression model with death as a competing risk. The included variables were age, sex, preoperative defect, stem offset, and stem size.
A sensitivity analysis was performed using only the first hip in patients with bilateral stem revision. Since it resulted in similar estimates, no joint frailty model was estimated. Data of six patients with bilateral stem revisions were analyzed as independent.
A part of the results from a previously published study using the Virtec straight stem in primary THA (same stem, same bone cement) were compared to the results from the current study [14]. Cumulative incidence for aseptic loosening of the stem was compared according to Gray [24].
Continuous data were presented as mean (standard deviation) with range. Categorical data were presented as frequencies (percentages). The analysis was performed using a significance level of α = 0.05. R statistical package was used for all analyses.
Results
Preoperative femoral defect types were distributed as followed: 47 hips (24.7%) with defect type 1, 58 hips (32.6%) with defect type II, 57 hips with defect type IIIa/b (32%) and no hips with defect type IV (Table 1).
Out of 178 hips there was no revision in 145 cases: a total of 74 patients (77 hips) had died after 9.1 (5.0) years (range 0.0–19.6 years) of causes unrelated to the THA without re-revision. 9 hips were lost to follow-up after 6.1 (4.4) years (range 1.6–14.0 years). The mean clinical follow-up was 9.3 (5.2) years (range 0–20.5 years). 80 hips had a more than 10-year radiographic follow-up (Fig. 3).
A total of 23 stems (12.9%) were re-revised: 15 for aseptic loosening, 2 after a periprosthetic femoral fracture and 6 due to PJI. Out of these six cases with PJI, two occurred after aseptic stem revision, one for persistent infection with coagulase negative staphylococci (CNS), and three had a further PJI with a new germ after previously being revised for PJI. In addition, there was one isolated cup revision during follow-up.
The cumulative incidence for aseptic loosening of the stem at 10 years was 5.5% [95% confidence interval (CI) 2.9–10.2%), whereas the cumulative incidence for death was 30.1% (95% CI 23.6–37.8%, Fig. 2). The cumulative incidence for aseptic loosening of the stem at 10 years assuming all patients which were lost to follow-up had been re-revised for aseptic loosening (worst-case scenario), was 9.9% (95% CI 6.3–15.4%).
The cumulative incidence for re-revision for any reason at 10 years was 9.9% (95% CI 6.3–15.5%).
The absolute risk ratios (ARR) for aseptic loosening of the stem are presented in Table 3. Aseptic loosening is associated with younger age (p = 0.02), larger defect size (p = 0.01/p = 0.07) and larger stem size (p < 0.001).
80 stems were eligible for a detailed radiological long-term analysis (Fig. 3). The average radiological follow-up for all unrevised stems was 12.9 (3.5) years (range 10–20.5 years) and 12.1 (4.2) years (range 0.7–20.5 years) for all hips, including the re-revised cases.
Osteolysis was found in 39 of 80 stems (48.8%, Table 4; Fig. 4). 10 cases (12.5%) showed a circumferential radiolucency in all Gruen zones (of which 8 were re-revised). 13 cases (16.3%) showed a significant subsidence of more than 2 mm, median subsidence of these cases was 6 mm (range 3–10 mm). 5 out of 13 cases with subsidence were re-revised for aseptic loosening.
Debonding was rare and was only seen in two cases. No fracture of the cement mantle was observed.
Results were compared to a part of previously published data obtained using the same implant and bone cement but for primary THA (survival data of 268 patients; 282 hips) [14]. Age at the time of implantation, sex and BMI were comparable in both groups. The only difference between the groups was the stem size implanted. In the revision group, generally larger stems (sizes 11 and 12) were used.
For the primary THA group, the cumulative incidence for aseptic loosening of the stem at 10 years was 1.8% (95% CI 0.8–4.3%). This was significantly lower when compared to revision THA (p = 0.01). No significant difference could be found between the cumulative incidence for death at 10 years for the primary THA group [23.3% (95% CI: 19.1–29.2%)] and for the revision THA group (p = 0.58).
The cumulative incidence for revision for any reason at 10 years for primary THA was 5.0% (95% CI 3.0–8.2%).
Discussion
The current study presents long-term results, in terms of survivorship and radiological outcome, for the cemented Virtec straight stem when used in revision THA. The present findings suggest excellent long-term results in revision THA when using the Virtec straight stem and shape-closed fixation technique.
The cumulative incidence for re-revision due to aseptic loosening after 10 years in our series was 5.5% (95% CI 2.9–10.2%). This falls into the lower range of previously published re-revision rates (8–22%) reported for cemented stem revisions [25,26,27,28,29,30].
The majority of the stems, which were revised, were cemented titanium Müller-type straight stems which have known detrimental effects on survival rates [31, 32]. Becoming aware of this problem, patients were closely followed up at our institution, thus allowing early diagnosis of loosening. This may explain the rather small defect sizes observed, with almost 60% of the patients having defect size I or II.
A high mortality indicates higher comorbidities, which is known as a general risk factor for revision in THA [33]. 74 patients (77 hips) died during the study period in the revision cohort, while only 14 stems were re-revised for aseptic loosening. Therefore, a cumulative incidence method was used to analyze revision rates [34,35,36]. Although the effect may not be clinically significant, the Kaplan–Meier estimates of implant failure are biased and would overestimate the risk of revision [37]. Anyhow it can be noted that the mean age of the patients at the time of the index surgery in the revision group was comparable to the mean age of the patients in the primary cohort. Therefore, the age of the patients in the revision THA group, at the time of the first implantation, was even younger when compared to the primary THA group.
The use of a cemented straight stem in revision THA is an extremely attractive method from an economic point of view [38]. Furthermore, it allows immediate full weight bearing without the risk of stem subsidence [39]. This may be of advantage for elderly, often frail patients, where longer partial weight bearing results in longer functional recovery time or is even impossible.
Risk factors for aseptic loosening of the Virtec stem in this study were young age, large defect size and large stem size. While young age is in accordance with the findings described by Clauss et al. [32] and Hallan et al. [40] for primary THA, the increased risk for revision of large stems is contradictory to results found in the literature. In our revision THA collective, larger stems were used when compared to our collective of primary THA, indicating that cavitary defects were present. In patients with huge cavitary defects, the pressure exerted on the cement mantle during stem insertion might be lower than with a stem which fills the medullary canal completely, resulting in a poorer press-fit in the AP plane. Furthermore, with an undersized implant (i.e., a complete cement mantle), the cement mantle may act differently and might not follow the principle of the “French paradox” [10].
Radiological changes around the stem were more frequent in the revision group compared to the series of primary THA. Osteolysis in any Gruen zone was found in 49% of all cases (39 of 80 stems) with a follow-up of more than 10 years in the revision THA group. However, only ten of these cases showed a circumferential radiolucency in all Gruen zones, eight of which were re-revised. Loosening, when rarely detected, always occurred at the cement–bone interface. This is normally observed in cemented stems with rougher surfaces were initially described by Gardiner et al. [41] Interestingly, the shape of the osteolysis was different in the revision THA group when compared to primary THA group. Osteolysis at the cement–bone interface in primary THA was more bead-shaped; in revision THA, osteolysis was more often like a scalloping radiolucent line without bead-shaped aspects (Figs. 4, 5). This finding may be due to the fact that during stem revision a meticulous debridement of all synovial membranes and remaining cancellous bone was achieved and a sound interdigitation between the cement and smooth inner cortex was not possible. This also explains the absence of debonding in the second interface (cement–stem) after a minimum follow-up of 10 years even with non-polished stems.
In conclusion, cemented straight stems, fixed according to the shape-closed principle, used in revision THA showed excellent long-term results regarding survivorship and radiological outcome. The mechanism of loosening might be different than in primary THA. Cemented straight stems offer a valuable and cost-effective option for revision THA, especially in the ever-growing number of geriatric patients requiring stem revision, where full weightbearing after surgery is favorable for functional recovery.
References
Kurtz S et al (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89(4):780–785
Patel A et al (2015) The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Jt J 97-B(8):1076–1081
Fink B, Urbansky K, Schuster P (2014) Mid term results with the curved modular tapered, fluted titanium Revitan stem in revision hip replacement. Bone Jt J 96-B(7):889–895
Bircher HP et al (2001) The value of the Wagner SL revision prosthesis for bridging large femoral defects. Orthopade 30(5):294–303
Abdel MP et al (2017) Modular fluted tapered stems in aseptic revision total hip arthroplasty. J Bone Jt Surg Am 99(10):873–881
Te Stroet MA et al (2015) Satisfying outcomes scores and survivorship achieved with impaction grafting for revision THA in young patients. Clin Orthop Relat Res 473(12):3867–3875
Schreurs BW et al (2005) Femoral component revision with use of impaction bone-grafting and a cemented polished stem. J Bone Jt Surg Am 87(11):2499–2507
Ornstein E et al (2002) Early complications after one hundred and forty-four consecutive hip revisions with impacted morselized allograft bone and cement. J Bone Jt Surg Am 84-A(8):1323–1328
Scheerlinck T, Casteleyn PP (2006) The design features of cemented femoral hip implants. J Bone Jt Surg Br 88(11):1409–1418
Langlais F et al (2003) The ‘French paradox’. J Bone Jt Surg Br 85(1):17–20
Clauss M et al (2010) The histology around the cemented Muller straight stem: a post-mortem analysis of eight well-fixed stems with a mean follow-up of 12.1 years. J Bone Jt Surg Br 92(11):1515–1521
Postel M et al (1987) Total hip replacement. Springer, Berlin
Kerboull L et al (2004) Long-term results of Charnley-Kerboull hip arthroplasty in patients younger than 50 years. Clin Orthop Relat Res 418:112–118
Clauss M et al (2016) Similar effect of stem geometry on radiological changes with 2 types of cemented straight stem: the Muller stem and the Virtec stem compared in 711 hips. Acta Orthop 87(2):120–125
Della Valle CJ, Paprosky WG (2003) Classification and an algorithmic approach to the reconstruction of femoral deficiency in revision total hip arthroplasty. J Bone Jt Surg Am 85-A(Suppl 4):1–6
El Masri F et al (2010) Is the so-called ‘French paradox’ a reality?: long-term survival and migration of the Charnley-Kerboull stem cemented line-to-line. J Bone Jt Surg Br 92(3):342–348
Kühn K-D (2014) PMMA cements. Springer, Berlin, Heidelberg
Zimmerli W, Trampuz A, Ochsner PE (2004) Prosthetic-joint infections. N Engl J Med 351(16):1645–1654
Gruen TA, McNeice GM, Amstutz HC (1979) Modes of failure of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27
Joshi RP et al (1998) Osteolysis after Charnley primary low-friction arthroplasty. A comparison of two matched paired groups. J Bone Jt Surg Br 80(4):585–590
Raber DA, Czaja S, Morscher EW (2001) Fifteen-year results of the Muller CoCrNiMo straight stem. Arch Orthop Trauma Surg 121(1–2):38–42
Clauss M et al (2009) Fixation and loosening of the cemented Muller straight stem: a long-term clinical and radiological review. J Bone Jt Surg Br 91(9):1158–1163
Harris WH, McCarthy JC Jr, O’Neill DA (1982) Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Jt Surg Am 64(7):1063–1067
Gray RJ (1988) A class of K-Sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16(3):1141–1154
Haydon CM et al (2004) Revision total hip arthroplasty with use of a cemented femoral component. Results at a mean of ten years. J Bone Jt Surg Am 86(6):1179–1185
Iorio R, Healy WL, Presutti AH (2008) A prospective outcomes analysis of femoral component fixation in revision total hip arthroplasty. J Arthroplasty 23(5):662–669
Mulroy WF, Harris WH (1996) Revision total hip arthroplasty with use of so-called second-generation cementing techniques for aseptic loosening of the femoral component. A fifteen-year-average follow-up study. J Bone Jt Surg Am 78(3):325–330
Gramkow J et al (2001) Long-term results after cemented revision of the femoral component in total hip arthroplasty. J Arthroplasty 16(6):777–783
Wang L et al (2013) Medium-term outcomes of cemented prostheses and cementless modular prostheses in revision total hip arthroplasty. Sci Rep 3:2796
Estok DM II, Harris WH (1994) Long-term results of cemented femoral revision surgery using second-generation techniques. An average 11.7-year follow-up evaluation. Clin Orthop Relat Res 299:190–202
Maurer TB et al (2001) Increased loosening of cemented straight stem prostheses made from titanium alloys. An analysis and comparison with prostheses made of cobalt-chromium-nickel alloy. Int Orthop 25(2):77–80
Clauss M et al (2013) Risk factors for aseptic loosening of Muller-type straight stems: a registry-based analysis of 828 consecutive cases with a minimum follow-up of 16 years. Acta Orthop 84(4):353–359
Prokopetz JJ et al (2012) Risk factors for revision of primary total hip arthroplasty: a systematic review. BMC Musculoskelet Disord 13:251
Gooley TA et al (1999) Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 18(6):695–706
Ranstam J et al (2011) Statistical analysis of arthroplasty data. II. Guidelines. Acta Orthop 82(3):258–267
Schwarzer G et al (2001) Statistical analysis of failure times in total joint replacement. J Clin Epidemiol 54(10):997–1003
Gillam MH et al (2010) Competing risks survival analysis applied to data from the Australian Orthopaedic Association National Joint Replacement Registry. Acta Orthop 81(5):548–555
Unnanuntana A et al (2009) Cementless femoral prostheses cost more to implant than cemented femoral prostheses. Clin Orthop Relat Res 467(6):1546–1551
Tangsataporn S et al (2015) Risk factors for subsidence of a modular tapered femoral stem used for revision total hip arthroplasty. J Arthroplasty 30(6):1030–1034
Hallan G et al (2012) Is there still a place for the cemented titanium femoral stem? 10,108 cases from the Norwegian Arthroplasty Register. Acta Orthop 83(1):1–6
Gardiner RC, Hozack WJ (1994) Failure of the cement–bone interface. A consequence of strengthening the cement-prosthesis interface? J Bone Jt Surg Br 76(1):49–52
Acknowledgements
The authors thank Tamara Horn Lang, PhD for proofreading the manuscript.
Funding
Part of this work was supported by Heraeus Medical GmbH, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the local ethics committee. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Pallaver, A., Zwicky, L., Bolliger, L. et al. Long-term results of revision total hip arthroplasty with a cemented femoral component. Arch Orthop Trauma Surg 138, 1609–1616 (2018). https://doi.org/10.1007/s00402-018-3023-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3023-9