Abstract
Purpose
Studies of the association between maternal nutrition and birth outcomes have investigated differing nutrients, maternal socioeconomic conditions, and timing within the reproductive cycle; and have produced inconsistent results. We evaluated the association of preconceptional maternal dietary intake with birth outcomes among low socioeconomic status ethnic minority women in a high-income country.
Methods
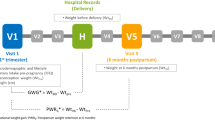
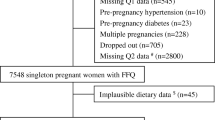
In this prospective cohort study, habitual preconceptional dietary intake was assessed among pregnant Bedouin Arab women in Israel (n = 384), using a short culturally specific, targeted food frequency questionnaire. Multiple nutrients (protein, lysine, calcium, iron, zinc, folate, omega-3 fatty acids) were evaluated simultaneously via a diet quality score derived from principal component analysis. Multivariable logistic regression was used to test associations between the diet quality score and a composite adverse birth outcomes variable, including preterm birth, low birth weight and small for gestational age.
Results
Sixty-nine women (18%) had adverse birth outcomes. Women with low preconceptional diet quality scores had low intakes of nutrient-rich plant foods, bioavailable micronutrients, and complete proteins. In multivariable analysis, a woman at the 10th percentile of the diet quality score had a 2.97 higher odds (95% CI 1.28–6.86) of an adverse birth outcome than a woman at the 90th percentile.
Conclusion
Low diet quality during the preconceptional period was associated with adverse birth outcomes among low socioeconomic status minority women in a high-income country. The results have implications for the development of appropriate intervention strategies to prevent adverse birth outcomes, and the promotion of adequate nutrition throughout the child-bearing years.



Similar content being viewed by others
References
Abu-Saad K, Fraser D (2010) Maternal nutrition and birth outcomes. Epidemiol Rev 32:5–25
King JC (2016) A summary of pathways or mechanisms linking preconception maternal nutrition with birth outcomes. J Nutr 146:437S–S444
Wu G, Bazer FW, Cudd TA et al (2004) Maternal nutrition and fetal development. J Nutr 134:2169–2172
Emond JA, Karagas MR, Baker ER et al (2018) Better diet quality during pregnancy is associated with a reduced likelihood of an infant born small for gestational age: an analysis of the prospective New Hampshire Birth Cohort Study. J Nutr 148:22–30
Grieger JA, Clifton VL (2014) A review of the impact of dietary intakes in human pregnancy on infant birthweight. Nutrients 7:153–178
Haider BA, Bhutta ZA (2017) Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev (4):Art. No.: CD004905. 10.1002/14651858.CD004905.pub5
Fall CH, Yajnik CS, Rao S et al (1756S) Micronutrients and fetal growth. J Nutr 133:1747S–1756S
Villar J, Merialdi M, Gulmezoglu AM et al (1625S) Nutritional interventions during pregnancy for the prevention or treatment of maternal morbidity and preterm delivery: an overview of randomized controlled trials. J Nutr 133:1606S–1625S
Carmichael SL, Yang W, Shaw GM, National Birth Defects Prevention Study (2013) Maternal dietary nutrient intake and risk of preterm delivery. Am J Perinatol 30:579–88
Grieger JA, Grzeskowiak LE, Clifton VL (2014) Preconception dietary patterns in human pregnancies are associated with preterm delivery. J Nutr 144:1075–1080
Stephenson J, Heslehurst N, Hall J et al (2018) Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet 391:1830–1841
Langley-Evans AJ, Langley-Evans SC (2003) Relationship between maternal nutrient intakes in early and late pregnancy and infants’ weight and proportions at birth: prospective cohort study. J R Soc Promot Health 123:210–216
Mathews F, Yudkin P, Neil A (1999) Influence of maternal nutrition on outcome of pregnancy: prospective cohort study. BMJ 319:339–343
de Graaf JP, Steegers EA, Bonsel GJ (2013) Inequalities in perinatal and maternal health. Curr Opin Obstet Gynecol 25:98–108
Willis E, McManus P, Magallanes N et al (2014) Conquering racial disparities in perinatal outcomes. Clin Perinatol 41:847–875
Rubin L, Belmaker I, Somekh E (2017) Maternal and child health in Israel: building lives. Lancet 389:2514–2530
Groen JJ, Balough M, Levy M et al (1964) Nutrition of the Bedouins in the Negev desert. Am J Clin Nutr 14:37–46
Abu-Saad K, Shai I, Kaufman-Shriqui V et al (2009) Bread type intake is associated with lifestyle and diet quality transition among Bedouin Arab adults. Br J Nut 102:1513–1522
Central Bureau of Statistics (2016) Local authorities, in ascending order of the socio-economic index 2015: index value, rank and cluster, and changes compared to 2013. https://old.cbs.gov.il/publications19/1765_socio_economic_2015/pdf/t02.pdf. Accessed 5 Oct 2019
Central Bureau of Statistics (2015) Statistical Abstract of Israel No. 66. Central Bureau of Statistics, Table 3.11, Jerusalem
Haas EJ, Bilenko N, Shoham-Vardi I (2014) Infant mortality in Bedouin Arabs in the Negev. Int Public Health J 6:9–16
Abu-Saad K, Shahar DR, Fraser D et al (2012) Adequacy of usual dietary intake and nutritional status among pregnant women in the context of nutrition transition: the DEPOSIT Study. Br J Nutr 108:1874–1883
Abu-Ghanem S, Sheiner E, Sherf M et al (2012) Lack of prenatal care in a traditional community: trends and perinatal outcomes. Arch Gynecol Obstet 285:1237–1242
Gottlieb N, Belmaker I, Bilenko N et al (2010) Bedouin-Arab women’s access to antenatal care at the interface of physical and structural barriers: a pilot study. Glob Public Health 2:1–14
Abu-Saad K, Shahar DR, Abu-Shareb H et al (2009) Assessing individual dietary intake from common-plate meals: a new tool for an enduring practice. Pub Health Nutr 12:2464–2472
US Department of Agriculture (1995) Continuing survey of food intakes by individuals (CSFII) 1994. USDA, Washington, DC
Abu-Saad K, Shai I, Vardi H et al (2011) Rapid assessment tools for ranking pregnant minority women into multi-nutrient exposure groups. Public Health Nutr 14:379–387
Abu-Saad K, Shahar DR, Vardi H et al (2010) Importance of ethnic foods as predictors of and contributors to nutrient intake levels in a minority population. Eur J Clin Nutr 64:S88–S94
Shai I, Vardi H, Shahar DR et al (2003) Adaptation of international nutrition databases and data-entry system tools to a specific population. Public Health Nutr 6:401–406
Khokhar S, Gilbert PA, Moyle CWA et al (2009) Harmonized procedures for producing new data on the nutritional composition of ethnic foods. Food Chem 113:816–824
Goldenberg RL, Culhane JF (2007) Low birth weight in the United States. Am J Clin Nutr 85:584S–590S
Dollberg S, Haklai Z, Mimouni FB et al (2005) Birth weight standards in the live-born population in Israel. IMAJ 7:311–314
Kessner DM, Singer J, Kalk CE et al (1973) Infant death: an analysis by maternal risk and health care. In: Contrasts in health status, vol 1. Institute of Medicine, Washington, DC
Ministry of Health (2001) Regulations for care of the pregnant woman. Regulation No. 1/2001. Ministry of Health, Jerusalem (in Hebrew)
Cunningham FG, Leveno KL, Bloom SL et al (2007) Prenatal care. Williams obstetrics, 22nd edn. McGraw, New York, pp 201–230
Institute of Medicine, National Research Council (2009) Weight gain during pregnancy: reexamining the guidelines. The National Academies Press, Washington, DC
Carroll RJ, Ruppert D, Stefanski LA et al (2006) Measurement error in nonlinear models—a modern perspective, 2nd edn. Chapman & Hall, Boca Raton
Simopoulos AP (2000) Human requirement for n-3 polyunsaturated fatty acids. Poult Sci 79:961–970
Kibret KT, Chojenta C, Gresham E et al (2018) Maternal dietary patterns and risk of adverse pregnancy (hypertensive disorders of pregnancy and gestational diabetes mellitus) and birth (preterm birth and low birth weight) outcomes: a systematic review and meta-analysis. Public Health Nutr. https://doi.org/10.1017/S1368980018002616
Thompson JM, Wall C, Becroft DM et al (2010) Maternal dietary patterns in pregnancy and the association with small-for-gestational-age infants. Br J Nutr 103:1665–1673
Gresham E, Collins CE, Mishra GD et al (2016) Diet quality before or during pregnancy and the relationship with pregnancy and birth outcomes: the Australian Longitudinal Study on Women's Health. Public Health Nutr 19:2975–2983
Ramakrishnan U, Grant F, Goldenberg T et al (2012) Effect of women's nutrition before and during early pregnancy on maternal and infant outcomes: a systematic review. Paediatr Perinat Epidemiol 26(Suppl 1):285–301
Novikov I, Fund N, Freedman LS (2010) A modified approach to estimating sample size for simple logistic regression with one continuous covariate. Stat Med 29:97–107
National Cancer Institute. Dietary Assessment Primer: Learn more about energy adjustment. https://dietassessmentprimer.cancer.gov/learn/adjustment.html. Accessed 24 Dec 2019.
Willett WC (2013) Nutritional epidemiology, 3rd edn. Oxford University Press, Oxford, pp 275–276
Payne M, Stephens T, Lim K et al (2018) Lysine requirements of healthy pregnant women are higher during late stages of gestation compared to early gestation. J Nutr 148:94–99
Fleming TP, Watkins AJ, Sun C et al (2015) Do little embryos make big decisions? How maternal dietary protein restriction can permanently change an embryo's potential, affecting adult health. Reprod Fertil Dev 27:684–692
Young VR, Pellett PL (1994) Plant proteins in relation to human protein and amino acid nutrition. Am J Clin Nutr 59:203S–212S
de Gavelle E, Huneau JF, Bianchi CM et al (2017) Protein adequacy is primarily a matter of protein quantity, not quality: modeling an increase in plant: animal protein ratio in French adults. Nutrients 9(12):E1333
van Rompay MI, McKeown NM, Castaneda-Sceppa C et al (2012) Acculturation and sociocultural influences on dietary intake and health status among Puerto Rican adults in Massachusetts. J Acad Nutr Diet 112:64–74
Oken E, Kleinman KP, Olsen SF et al (2004) Associations of seafood and elongated n-3 fatty acid intake with fetal growth and length of gestation: results from a US pregnancy cohort. Am J Epidemiol 160:774–783
Sparks PJ (2009) Do biological, sociodemographic, and behavioral characteristics explain racial/ethnic disparities in preterm births? Soc Sci Med 68:1667–1675
Hussain T, Abbas S, Khan MA et al (2004) Lysine fortification of wheat flour improves selected indices of the nutritional status of predominantly cereal-eating families in Pakistan. Food Nutr Bull 25:114–122
Ramakrishnan U, Nguyen PH, Gonzalez-Casanova I et al (1445S) Neither preconceptional weekly multiple micronutrient nor iron-folic acid supplements affect birth size and gestational age compared with a folic acid supplement alone in rural Vietnamese women: a randomized controlled trial. J Nutr 146:1445S–S2152
Hamersma S, Hou Y, Kim Y et al (2018) Business cycles, Medicaid generosity and birth outcomes. Popul Res Policy Rev 37:729
Puthussery S (2016) Perinatal outcomes among migrant mothers in the United Kingdom: is it a matter of biology, behaviour, policy, social determinants or access to health care? Best Pract Res Clin Obstet Gynaecol 32:39–49
Braveman P, Gottlieb L (2014) The social determinants of health: it's time to consider the causes of the causes. Public Health Rep 129(Suppl 2):19–31
National Cancer Institute. Short Dietary Assessment Instruments. National Cancer Institute, Division of Cancer Control & Population Studies, Epidemiology and Genomics Research Program. https://epi.grants.cancer.gov/diet/screeners/. Accessed 24 Dec 2019.
Thompson FE, Subar AF, Smith AF, Midthune D, Radimer KL, Kahle LL, Kipnis V (2002) Fruit and vegetable assessment: performance of 2 new short instruments and a food frequency questionnaire. J Am Diet Assoc 102:1764–1772
Colón-Ramos U, Thompson FE, Yaroch AL, Moser RP, McNeel TS, Dodd KW, Atienza AA, Sugerman SB, Nebeling L (2009) Differences in fruit and vegetable intake among Hispanic subgroups in California: results from the 2005 California Health Interview Survey. J Am Diet Assoc 109:1878–1885
Schröder H, Fitó M, Estruch R et al (2011) A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J Nutr 141:1140–1145
McClure R, Villani A (2019) Greater adherence to a Mediterranean Diet is associated with better gait speed in older adults with type 2 diabetes mellitus. Clin Nutr ESPEN 32:33–39
Hillier SE, Olander EK (2017) Women's dietary changes before and during pregnancy: a systematic review. Midwifery 49:19–31
Cucó G, Fernández-Ballart J, Sala J et al (2006) Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. Eur J Clin Nutr 60:364–371
Hure A, Young A, Smith R, Collins C (2009) Diet and pregnancy status in Australian women. Public Health Nutr 12:853–861
Pinto E, Barros H, dos Santos SI (2009) Dietary intake and nutritional adequacy prior to conception and during pregnancy: a follow-up study in the north of Portugal. Public Health Nutr 12:922–931
Endeweld M, Fruman A, Gottlieb D (2008) Poverty and social gaps in 2007: annual report. National Insurance Institute, Jerusalem. https://www.btl.gov.il/English%20Homepage/Publications/Poverty_Report/Documents/oni2007-E.pdf. Accessed 3 Sept 2019
Endeweld M, Gottlieb D, Heller O et al (2017) Poverty and social gaps: 2016 annual report. National Insurance Institute, Jerusalem. https://www.btl.gov.il/English%20Homepage/Publications/Poverty_Report/Documents/oni2016-e.pdf. Accessed 3 Sept 2019
Berger-Polsky A, Daoud N, Sergienko R et al (2019) Polygamy and birth outcomes among Bedouin women of the Negev: the contribution of social determinants and pregnancy complications. Health Care Women Int. https://doi.org/10.1080/07399332.2019.1639708
Acknowledgements
We would like to thank the women who participated in the DEPOSIT cohort, the study staff of the S. Daniel Abraham Center for Health and Nutrition at Ben-Gurion University of the Negev, and the staff of the Maternal and Child Health and High Risk Pregnancy clinics. We would also like to thank Dr. Ilya Novikov for conducting the power analysis. This work was supported by a grant from the Israel National Institute for Health Policy and Health Services Research [Grant Number: 2003/136/A]. The funding agency had no role in the design, conduct or analysis of the study; or in the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
KA-S and DF conceived of and procured the funding for study, and KA-S was responsible for the project administration. KA-S, DF and LSF planned and conducted the analysis, with input from VK-S and IB, KA-S prepared the initial manuscript draft. All authors critically reviewed the manuscript for important intellectual content; and gave final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Abu-Saad, K., Kaufman-Shriqui, V., Freedman, L.S. et al. Preconceptional diet quality is associated with birth outcomes among low socioeconomic status minority women in a high-income country. Eur J Nutr 60, 65–77 (2021). https://doi.org/10.1007/s00394-020-02221-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-020-02221-4