Abstract
Purpose
Obesity is the main feature of a complex illness known as metabolic syndrome. Anti-obesogenic therapies are often associated with side effects and represent a high cost in conventional pharmacological approaches. New strategies based on natural remedies are under continuous investigation. Leopoldia comosa (L.) Parl. (L. comosa) is a spontaneous plant with diuretic, anti-inflammatory and antioxidant properties. Recently, a hypoglycemic activity mediated by inhibition of carbohydrate digestion has been identified. The aim of this study was to evaluate the effects of a diet supplemented with L. comosa extracts on a rat model of diet-induced obesity.
Methods
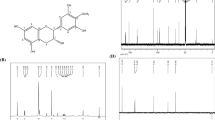
Leopoldia comosa bulb extracts were obtained using a dynamic extractor. Phytochemical properties and in vitro determination of the antioxidant activity and of the inhibitory effects on lipase and pancreatic amylase were performed. Rats were fed (12 weeks) a standard diet, or a high-fat diet (HFD), or an HFD plus L. comosa (20 or 60 mg/die) extracts. The metabolic and anthropometric parameters were recorded.
Results
Results indicated that L. comosa inhibited lipase and pancreatic amylase activities. In vivo data showed that the supplementation with both doses of L. comosa extracts counteracted the HFD-dependent effects. It reduced body weight, abdominal obesity and dyslipidemia, and improved glucose tolerance with a reduction of lipidic tissue hypertrophy and liver steatosis, as compared to HFD-fed rat. In liver, L. comosa reduced protein expression levels of PEPCK and G6Pase.
Conclusion
We suggest that L. comosa extracts prevent obesity-dependent metabolic disorders. This paves the way for their therapeutic application as a natural anti-obesity drug.









Similar content being viewed by others
References
González-Muniesa P, Mártinez-González MA, Hu FB, Després JP, Matsuzawa Y, Loos RJF, Moreno LA, Bray GA, Martinez JA (2017) Obesity. Nat Rev Dis Primers 3:17034. https://doi.org/10.1038/nrdp.2017.34
Kopelman PG (2000) Obesity as a medical problem. Nature 404:635–643. https://doi.org/10.1038/35007508
Mopuri R, Islam MS (2017) Medicinal plants and phytochemicals with anti-obesogenic potentials: a review. Biomed Pharmacother 89:1442–1452. https://doi.org/10.1016/j.biopha.2017.02.108
Sniderman A, Cainflone K (1995) Metabolic disruptions in the adipocyte–hepatocyte fatty acid axis as causes of HyperapoB. Int J Obesity 19:S27–S33
Alpert MA (2001) Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. Am J Med Sci 321(4):225–236. https://doi.org/10.1097/00000441-200104000-00003
de la Iglesia R, Loria-Kohen V, Zulet MA, Martinez JA, Reglero G, Ramirez de Molina A (2016) Dietary strategies implicated in the prevention and treatment of metabolic syndrome. Int J Mol Sci. https://doi.org/10.3390/ijms17111877
de Freitas Junior LM, de Almeida EB Jr (2017) Medicinal plants for the treatment of obesity: ethnopharmacological approach and chemical and biological studies. Am J Transl Res 9(5):2050–2064
Borgonovo G, Caimi S, Morini G, Scaglioni L, Bassoli A (2008) Taste-active compounds in a traditional Italian food: Lampascioni. Chem Biodivers 5(6):1184–1194. https://doi.org/10.1002/cbdv.200890095
Pieroni A, Janiak V, Dürr CM, Lüdeke S, Trachsel E, Heinrich M (2002) In vitro antioxidant activity of non-cultivated vegetables of ethnic Albanians in southern Italy. Phytother Res 16(5):467–473. https://doi.org/10.1002/ptr.1243
Pieroni A, Nebel S, Quave C, Münz H, Heinrich M (2002) Ethnopharmacology of liakra: traditional weedy vegetables of the Arbëreshë of the Vulture area in southern Italy. J Ethnopharmacol 81(2):165–185. https://doi.org/10.1016/S0378-8741(02)00052-1
Motti R, Antignani V, Idolo M (2009) Traditional plant use in the Phlegraean Fields Regional Park (Campania, southern Italy). Hum Ecol 37:775–782. https://doi.org/10.1007/s10745-009-9254-1
Loizzo MR, Tundis R, Menichini F, Pugliese A, Bonesi M, Solimene U, Menichini F (2010) Chelating, antioxidant and hypoglycaemic potential of Muscari comosum (L.) Mill. (L.) Mill. bulb extracts. Int J Food Sci Nutr 61(8):780–791. https://doi.org/10.3109/09637486.2010
Casacchia T, Sofo A, Casaburi I, Marrelli M, Conforti F, Statti GA (2017) Antioxidant, enzyme-inhibitory and antitumor activity of the wild dietary plant Muscari comosum (L.). Mill Int J Plant Biol 8:6895. https://doi.org/10.4081/pb.2017.6895
Adinolfi M, Barone G, Belardini M, Lanzetta R, Laonigro G, Parilli M (1984) Homoisoflavanones from Muscari comosum (L.) Mill. Bulbs Phytochem 24:2423–2426. https://doi.org/10.1016/S0031-9422(00)83055-1
Adinolfi M, Barone G, Belardin M, Lanzetta R, Laonigro G, Mangoni L, Parilli M (1985) Three 3-benzyl-4-chromanones from Muscari comosum (L.) Mill. Phytochemistry 24:624–626. https://doi.org/10.1016/S0031-9422(00)84989-4
Adinolfi M, Barone G, Corsaro MM, Lanzetta R, Mangoni L (1987) Glycosides from Muscari comosum (L.) Mill. 7. Structure of three novel muscarosides. Can J Chem 65:2317–2326. https://doi.org/10.1139/v87-387
Adinolfi M, Barone G, Corsaro MM, Mangoni L, Lanzetta R, Parrilli M (1988) Absolute configuration of homoisoflavanones from Muscari species. Tetrahedron 44:4981–4988. https://doi.org/10.1016/S0040-4020(01)86202-5
Marrelli M, Cristaldi B, Menichini F, Conforti F (2015) Inhibitory effects of wild dietary plants on lipid peroxidation and on the proliferation of human cancer cells. Food Chem Toxicol 86:16–24. https://doi.org/10.1016/j.fct.2015.09.011
Marrelli M, Conforti F, Toniolo C, Nicoletti M, Statti G, Menichini F (2014) Hypericum perforatum: influences of the habitat on chemical composition, photo-induced cytotoxicity, and antirad-ical activity. Pharm Biol 52(7):909–918. https://doi.org/10.3109/13880209.2013.872675
Conforti F, Perri V, Menichini F, Marrelli M, Uzunov D, Statti GA, Menichini F (2012) Wild Mediterranean dietary plants as inhibitors of pancreatic lipase. Phytother Res 26(4):600–604. https://doi.org/10.1002/ptr.3603
Kwon YI, Apostolidis E, Kim YC, Shetty K (2007) Health benefits of traditional corn, beans and pumpkin: in vitro studies for hyperglycemia and hypertension management. J Med Food 10:266–275. https://doi.org/10.1089/jmf.2006.234
Ferraz RR, Tiselius HG, Heiberg IP (2004) Fat malabsorption induced by gastrointestinal lipase inhibitor leads to an increase in urinary oxalate excretion. Kidney Int 66:676–682. https://doi.org/10.1111/j.1523-1755.2004.00790.x
Kim JH, Kim OK, Yoon HG, Park J, You Y, Kim K, Lee YH, Choi KC, Lee J, Jun W (2016) Anti-obesity effect of extract from fermented Curcuma longa L. through regulation of adipogenesis and lipolysis pathway in high-fat diet-induced obese rats. Food Nutr Res 60:30428. https://doi.org/10.3402/fnr.v60.30428
Okamura T, Pei XY, Miyoshi I, Shimizu Y, Takanashi-Yanobu R, Mototani Y, Kanai T, Satoh J, Kimura N, Kasai N (2013) Phenotypic characterization of LEA rat: a new rat model of non obese type 2 diabetes. J Diabetes Res. 2013:986462. https://doi.org/10.1155/2013/986462
Panchal SK, Poudyal H, Brown L (2012) Quercetin ameliorates cardiovascular, hepatic, and metabolic changes in diet-induced metabolic syndrome in rats. J Nutr 142(6):1026–1032. https://doi.org/10.3945/jn.111.157263
Garofalo F, Imbrogno S, Tota B, Amelio D (2012) Morpho-functional characterization of the goldfish (Carassius auratus L.) heart. Comp Biochem Physiol A Mol Integr Physiol 163(2):215–222. https://doi.org/10.1016/j.cbpa.2012.05.206
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419. https://doi.org/10.1007/BF00280883
Cacho J, Sevillano J, de Castro J, Herrera E, Ramos MP (2008) Validation of simple indexes to assess insulin sensitivity during pregnancy in Wistar and Sprague-Dawley rats. Am J Physiol Endocrinol Metab 295(5):E1269–E1276. https://doi.org/10.1152/ajpendo.90207.2008
Mulholland DA, Schwikkard SL, Crouch NR (2013) The chemistry and biological activity of the Hyacinthaceae. Nat Prod Rep 30(9):1165–1210. https://doi.org/10.1039/c3np70008a
Vera Regitz-Zagrosek V, Lehmkuhl E, Mahmoodzadeh S (2007) Gender aspects of the role of the MetS as a risk factor for cardiovascular disease. Gend Med 4:162–167. https://doi.org/10.1016/S1550-8579(07)80056-8
Tolpin DA, Collard CD, Lee VV, Elayda MA, Pan W (2009) Obesity is associated with increased morbidity after coronary artery bypass graft surgery in patients with renal insufficiency. J Thorac Cardiovasc Surg 138:873–879. https://doi.org/10.1016/j.jtcvs.2009.02.019
Etkin NL (1996) Medicinal cuisines: diet and ethnopharmacology. Int J Pharmacognosy 34:313–326. https://doi.org/10.1076/phbi.34.5.313.13246
Marrelli M, Loizzo MR, Nicoletti M, Menechini F, Conforti F (2014) In vitro investigation of the potential health benefits of wild Mediterranean dietary plants as anti-obesity agents with α-amylase and pancreatic lipase inhibitory activities. J Sci Food Agric 94(11):2217–2224. https://doi.org/10.1002/jsfa.6544
Pare D, Hilou A, Ouedraogo N, Guenne S (2016) Ethnobotanical study of medicinal plants used as anti-obesity remedies in the nomad and hunter communities of Burkina Faso. Medicines 3:9. https://doi.org/10.3390/medicines3020009
Seyedan A, Alshawsh MA, Alshagga MA, Koosha S, Mohamed Z (2015) Medicinal plants and their inhibitory activities against pancreatic lipase: a review. Evid Based Complement Altern Med. 2015:973143. https://doi.org/10.1155/2015/973143
Eichler HG, Korn A, Gasic S, Prison W, Businger J (1984) The effect of new specific α-amylase inhibitor on post-prandial glucose and insulin excursions in normal subjects and Type 2 (non-insulin dependent) diabetic patients. Diabetologia 26(4):278–281. https://doi.org/10.1007/BF00283650
Tarling CA, Woods K, Zhang R, Brastianos HC, Brayer GD, Andersen RJ, Withers SG (2008) The search for novel human pancreatic α-amylase inhibitors: high-throughput screening of terrestrial and marine natural product extracts. Chem Bio Chem 9:433–438. https://doi.org/10.1002/cbic.200700470
Han TS, van Leer EM, Seidell JC, Lean ME (1995) Waist circumference action levels in the identification of cardiovascular risk factors: prevalence study in a random sample. BMJ 311(7017):1401–1405. https://doi.org/10.1136/bmj.311.7017.1401
Sharabi K, Tavares CD, Rines AK, Puigserver P (2015) Molecular pathophysiology of hepatic glucose production. Mol Aspects Med 46:21–33. https://doi.org/10.1016/j.mam.2015.09.003
Barthel A, Schmoll D (2003) Novel concepts in insulin regulation of hepatic gluconeogenesis. Am J Physiol Endocrinol Metab 285(4):E685–E692. https://doi.org/10.1152/ajpendo.00253.2003
de Divitiis O, Fazio S, Petitto M, Maddalena G, Contaldo F, Mancini M (1981) Obesity and cardiac function. Circulation 64(3):477–482. https://doi.org/10.1161/01.CIR.64.3.477
Lauer MS, Anderson KM, Kannel WB, Levy D (1991) The impact of obesity on left ventricular mass and geometry. The Framingham Heart Study. JAMA 266(2):231–236. https://doi.org/10.1001/jama.1991.03470020057032
McMurray F, Patten DA, Harper ME (2016) Reactive oxygen species and oxidative stress in obesity-recent findings and empirical approaches. Obesity 24(11):2301–2310. https://doi.org/10.1002/oby.21654
Huang H, Mai W, Liu D, Hao Y, Tao J, Dong Y (2008) The oxidation ratio of LDL: a predictor for coronary artery disease. Dis Markers 24(6):341–349. https://doi.org/10.1155/2008/371314
Funding
This research was supported by “Dottorato di Ricerca in Medicina Traslazionale” (C.T.), “Dottorato di Ricerca in Scienze della Vita” (S.F., R.C., G.M.C., D.A., R.M., T.A) and MIUR of Italy (ex 60%).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Casacchia, T., Scavello, F., Rocca, C. et al. Leopoldia comosa prevents metabolic disorders in rats with high-fat diet-induced obesity. Eur J Nutr 58, 965–979 (2019). https://doi.org/10.1007/s00394-018-1609-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1609-1