Abstract
Arterial type of thoracic outlet syndrome belongs to the most unusual mechanisms of stroke in children in the first decade of life. We present a case diagnosed for bilateral and symmetric changes due to retrograde thromboembolic phenomenon. Regarding the age of the patient, the appropriate diagnostics and management are still a matter of debate in pediatric and neurological literature.
Similar content being viewed by others
Introduction
Arterial thoracic outlet syndrome (aTOS) is an extremely rare cause of embolic stroke in children [4]. A symptomatic compression of the subclavian artery (SA) may result from the osteo-musculo-vascular conflict provoked by a supernumerary rib, arising from C7 vertebra [11]. It usually presents with symptoms secondary to SA stenosis and subsequent antegrade embolization, such as loss of peripheral pulse, paresthesias in the hand, claudication, or digits ischemia [15]. Retrograde thromboembolic phenomenon may reveal during overhead abduction of the arm, which favors the occlusion of SA and promotes the occurrence of carotid or vertebrobasilar stroke [2, 6].
Several papers have been published about the symptomatology of retrograde stroke, some of them refer to pediatric population, but none of reported cases presented with symmetric infarctions due to aTOS in the first decade of life.
Case report
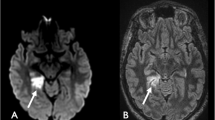
An 8-year-old girl presented with a history of sudden morning numbness of right limbs, headache, and vomiting, followed by tonic-clonic seizures and a loss of consciousness. On admission she was somnolent, moderately dehydrated, with right hemiparesis and right hemihypoesthesia. The warmth of right limbs was decreased but the pulse on peripheral arteries was normal. Magnetic resonance (MR) imaging revealed symmetrical changes in postero-lateral thalami and medial occipital lobes. Smaller areas were noted in the region of splenium of corpus callosum and within deep structures of the left cerebral hemisphere (Fig. 1a–d).
A series of tests towards the diagnosis of metabolic, autoimmune, and rheumatoid diseases, or coagulopathies was performed. None responded positive.
After 7 days, she deteriorated: became non-responsive, on neuro-exam anisocoria R > L, right-sided central facial palsy, bilateral hemiparesis R > L, and positive bilateral Babinski sign were noted. MR scan revealed a new large hyperintense area in the pons and some smaller in the cerebellum (Fig. 1e, f). 3D-TOF angiography showed an embolic mass within the basilar artery (BA) at the level of left AICA and partial occlusion of P2a segments of both posterior cerebral arteries (PCAs) (Fig. 2).
Physical examination revealed a loss of right radial pulse. Doppler-US showed normal flow values in the arteries of right arm and forearm but the complete occlusion of right SA due to an embolic mass at the origin of right vertebral artery (VA). The VA was partially occluded but had a torticuous canal of patency in its initial segment. Chest X-Ray revealed the presence of cervical ribs bilaterally (Fig. 3).
A CT-angiography of subclavian arteries in two typical arm positions was done (Fig. 4). It showed the occlusion of right SA with a developed suprascapular arterial anastomosis supplying the brachial artery. The scans also revealed bony anomalies in the region of superior thoracic aperture: cervical ribs and bifid 1st rib on the right, which fixed the diagnosis of right-sided aTOS, confirmed subsequently in catheter angiography a few days after. Regarding her age, surgeons decided to postpone surgical excision of cervical rib until the end of skeletal growth. She was placed on anticoagulant therapy with low molecular weight heparin combined with warfarin. After a few days, her neurological status improved—she was in good logical contact, responsive, with scattered speech. After rehabilitation sessions, she started to sit and walk without support. She was discharged with right-sided weakness and intention tremor.
Contrast-enhanced CT scans at two arm positions (a, b—anatomical position; c, d—overhead abduction). Right clavicle removed from 3D reconstructions (a, c) for visualization of cervical-1st rib complex. Coronal cuts (b, d) show subclavian arteries (right, SA-R; left, SA-L) passing between the clavicle (empty arrowhead) and first rib (white arrowheads). Occlusion within right SA (white arrows) reaches the right brachial artery (BrA), supplied by right suprascapular artery (SsA). Contrast medium visible on the right within the proximal SA and SsA. Empty arrow shows left cervical rib. Note the distance between the clavicle and 1st rib on both sides
Discussion
Symmetric cerebral infarction is uncommon in pediatric population. Various inflammatory and non-inflammatory vasculopathies (moya-moya, dissecting arteriopathies, infectious arteritis) may result in stroke but they rarely cause bilateral changes [8, 9, 12, 18, 21]. The ischemic area is usually supratentorial, in a carotid distribution, especially when resulting from aTOS provoked by a right cervical rib [10, 11, 15]. Consequently, symmetric changes are considered as typical rather for metabolic or inflammatory diseases of young age, requiring a wide range of diagnostic work-up [14]. The diagnostics is primarily directed towards systemic disorders, such as coagulopathies (responsible for young age stroke in up to 50%, specifically with such risk factors as elevated lipoprotein level, homocysteinemia, factor V Leiden trombophilia, protein C/S deficiency, or antiphospholipid syndrome) or cardiac diseases which are the cause of 10–30% of pediatric stroke [7, 12, 18].
Although demonstrated by other authors, anatomical conditions are seldom considered the first-line factors promoting cerebral infarction in a young. The youngest patient with a stroke due to aTOS described so far was 14 years old and presented with right-sided hemispheric stroke combined with cerebellar infarctions [11]. Our patient also suffered from supratentorial and infratentorial infarctions but of purely vertebrobasilar distribution. This is typical for the retrograde thromboembolic phenomenon, resulting from compression of SA distal to VA origin. This mechanism explains partial occlusion of BA resulting in pons infarction and subsequent thalamic and medial occipital strokes due to obliteration of both PCAs [16].
Cervical ribs are found in less than 1% of general population (more commonly in females) and in 80–90% of cases are asymptomatic [10]. Chronic compression of SA is diagnosed in < 1% of TOS [10, 15]. When symptomatic, the treatment includes a surgical excision of a cervical rib, commonly with the first rib. This method is relatively safe and provides good functional outcome for distal complaints [1, 5, 13].
However, to date, no clear evidence on the success rate of such treatment in aTOS children with stroke has been provided. Reported pediatric series [3, 13, 17, 19, 20] contain only single aTOS cases younger than 10 years. Although surgery seems effective for distal (forearm, hand) complaints, the risks and benefits of vascular reconstruction of the potential SA aneurysm are still a matter of debate. Therefore, regarding the lack of supportive data, it seems that non-operative treatment may be considered an option for preadolescents and surgery offered until the end of skeletal growth, what favors girls after the first menstruation and boys at the age of 14–16.
Conclusions
Symmetric cerebral infarctions are an uncommon presentation of aTOS in the first decade of life. Since retrograde embolic phenomenon may mimic inflammatory or metabolic disease, it should be of importance to exclude this rare cause of stroke. The excision of a supernumerary rib, although effective in adolescents, may be of limited benefit in preadolescent patients what favors non-operative management in case of lack of indications for urgent surgery.
References
Adson AW, Coffey JR (1927) Cervical rib: a method of anterior approach for relief of symptoms by division of the scalenus anticus. Ann Surg 85(6):839–857
al-Hassan HK, Abdul Sattar M, Eklof B (1988) Embolic brain infarction: a rare complication of thoracic outlet syndrome. A report of two cases. J Cardiovasc Surg 29(3):322–325
Arthur LG, Teich S, Hogan M, Caniano DA, Smead W (2008) Pediatric thoracic outlet syndrome: a disorder with serious vascular complications. J Pediatr Surg 43(6):1089–1094. https://doi.org/10.1016/j.jpedsurg.2008.02.038
Australian Childhood Stroke Advisory Committee (2017) Guideline for the diagnosis and acute management of childhood stroke. Available via https://www.mcri.edu.au/sites/default/files/media/stroke_guidelines.pdf. Accessed 6 May 2018
Chang KZ, Likes K, Davis K, Demos J, Freischlag JA (2013) The significance of cervical ribs in thoracic outlet syndrome. J Vasc Surg 57(3):771–775. https://doi.org/10.1016/j.jvs.2012.08.110
Daniels B, Michaud L, Sease F Jr, Cassas KJ, Gray BH (2014) Arterial thoracic outlet syndrome. Curr Sports Med Rep 13(2):75–80. https://doi.org/10.1249/JSR.0000000000000034
Greenham M, Gordon A, Anderson V, Mackay MT (2016) Outcome in childhood stroke. Stroke 47:1159–1164. https://doi.org/10.1161/STROKEAHA.115.011622
Guey S, Tournier-Lasserve E, Herve D, Kossorotoff M (2015) Moyamoya disease and syndromes: from genetics to clinical management. Appl Clin Genet 16(8):49–68. https://doi.org/10.2147/TACG.S42772
Hills NK, Johnston SC, Sidney S, Zielinski BA, Fullerton HJ (2012) Recent trauma and acute infection as risk factors for childhood arterial ischemic stroke. Ann Neurol 72:850–858. https://doi.org/10.1002/ana.23688
Jusufovic M, Sandset EC, Popperud TH, Solberg S, Ringstad G, Kerty E (2012) An unusual case of the syndrome of cervical rib with subclavian artery thrombosis and cerebellar and cerebral infarctions. BMC Neurol 12(48). https://doi.org/10.1186/1471-2377-12-48
Kataria R, Sharma A, Srivastava T, Bagaria H, Sharma A (2012) Cervical rib, a rare cause of recurrent stroke in the young: a case report. Neurologist 18(5):321–323. https://doi.org/10.1097/NRL.0b013e31826754a9
Lyle CA, Bernard TJ, Goldenberg NA (2011) Childhood arterial ischemic stroke: a review of etiologies, antithrombotic treatments, prognostic factors, and priorities for future research. Semin Thromb Hemost 37(7):786–793. https://doi.org/10.1055/s-0031-1297169
Matos JM, Gonzalez L, Kfoury E, Echeverria A, Bechara CF, Lin PH (2018) Outcomes following operative management of thoracic outlet syndrome in the pediatric patients. Vascular 26:410–417. https://doi.org/10.1177/1708538117747628
Mirsky DM, Beslow LA, Amlie-Lefond CA, Krishnan P, Laughlin S, Lee S, Lehman L, Rafay M, Shaw D, Rivkin MJ, Wintermark M (2017) Pathways for neuroimaging of childhood stroke. Pediatr Neurol 69:11–23. https://doi.org/10.1016/j.pediatrneurol.2016.12.004
Palaniandavan, Hafeezullah S, Raghav J, Anuradha N, Selvagambeer (2014) An interesting case of young stroke. WJMS 10(3):275–278. https://doi.org/10.5829/idosi.wjms.2014.10.3.82413
Prior AL, Wilson LA, Gosling RG, Yates AK, Ross Russell RW (1979) Retrograde cerebral embolism. Lancet 2(8151):1044–1047
Rehemutula A, Zhang L, Chen L, Chen D, Gu Y (2015) Managing pediatric thoracic outlet syndrome. Ital J Pediatr 41:22. https://doi.org/10.1186/s13052-015-0128-4
Rosa M, De Lucia S, Rinaldi VE, Le Gal J, Desmarest M, Veropalumbo C, Romanello S, Titomanlio L (2015) Paediatric arterial ischemic stroke: acute management, recent advances and remaining issues. Ital J Pediatr 41:95. https://doi.org/10.1186/s13052-015-0174-y
Teddy PJ, Johnson RD, Cai RR, Wallace D (2012) Surgery for paediatric thoracic outlet syndrome. J Clin Neurosci 19:235–240. https://doi.org/10.1016/j.jocn.2011.05.015
Vu AT, Patel PA, Elhadi H, Schwentker AR, Yakuboff KP (2014) Thoracic outlet syndrome in pediatric population: case series. J Hand Surg Am 39(3):484–487.e2. https://doi.org/10.1016/j.jhsa.2013.11.029
Wintermark M, Hills NK, DeVeber GA, Barkovich AJ, Bernard TJ, Friedman NR, Mackay MT, Kirton A, Zhu G, Leiva-Salinas C, Hou Q, Fullerton HJ (2017) Clinical and imaging characteristics of arteriopathy subtypes in children with arterial ischemic stroke: results of the VIPS study. AJNR Am J Neuroradiol 38(11):2172–2179. https://doi.org/10.3174/ajnr.A5376
Disclaimer
The authors declare that this manuscript has not been published elsewhere and is not under consideration by another journal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical committee approval
The authors declare that that the study complies with the current law in Poland.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Strzelecka, J., Skadorwa, T., Franckiewicz, M. et al. A case of symmetric retrograde thromboembolic cerebral infarction in an 8-year-old child due to arterial thoracic outlet syndrome. Childs Nerv Syst 34, 2503–2507 (2018). https://doi.org/10.1007/s00381-018-3911-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3911-x