Abstract
Objectives
Using preoperative PET/CT, we evaluated the prognostic value of preoperative [18F]FDG uptake ratio between various metastatic lesions and primary tumour in patients with advanced serous epithelial ovarian cancer (EOC).
Methods
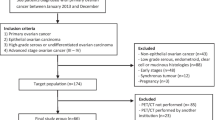
We retrospectively reviewed patients with International Federation of Gynecology and Obstetrics (FIGO) stage III, IV serous EOC who underwent preoperative [18F]FDG PET/CT scans. Clinico-pathological variables and PET/CT parameters such as maximum standardized uptake value of the ovarian cancer (SUVovary), pelvic or para-aortic LN (SUVLN), peritoneal (SUVperit) and distant extra-peritoneal (SUVdist) metastatic lesions, and the metastatic lesion-to-ovarian cancer standardized uptake value ratio were assessed.
Results
Clinico-pathological data were retrospectively reviewed for 97 eligible patients. The median progression-free survival (PFS) was 18 months (range, 6–90 months) and 59 (60.8 %) patients experienced recurrence. In multivariate regression analysis, older age (p = 0.035, hazard ratio (HR) 1.032, 95 % CI 1.002–1.062), and high SUVperit/SUVovary (p = 0.046, HR 1.755, 95 % CI 1.011–3.047) were independent risk factors of recurrence. Patient group categorized by SUVperit/SUVovary showed significant difference in PFS (Log-Rank test, p = 0.001).
Conclusions
In patients with advanced serous EOC, preoperative SUVperit/SUVovary measured by [18F]FDG PET/CT provides significant incremental performance for prediction of recurrence.
Key points
• PET/CT data from advanced serous epithelial ovarian cancer patients were analysed.
• Prognostic value of SUV ratio between metastatic and primary tumour was investigated.
• SUV perit /SUV ovary provides incremental performance for prediction of recurrence.


Similar content being viewed by others
Abbreviations
- EOC:
-
Epithelial ovarian cancer
- FIGO:
-
International Federation of Gynaecology and Obstetrics
- 18F[FDG]:
-
18F-fluorodeoxyglucose
- PET:
-
Positron emission tomography
- CT:
-
Computed tomography
- SUV:
-
Standardized uptake value
- LN:
-
Lymph node
- perit:
-
Peritoneal metastatic lesion
- dist:
-
Distant extra-peritoneal metastatic lesion
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- OS:
-
Overall survival
References
Heintz AP, Odicino F, Maisonneuve P, et al. (2006) Carcinoma of the ovary. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet 95 Suppl 1:S161-192.
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ (2009) Cancer statistics, 2009. CA Cancer J Clin 59:225–249
Angioli R, Capriglione S, Aloisi A et al (2014) Can HE4 predict platinum response during first-line chemotherapy in ovarian cancer? Tumour Biol 35:7009–7015
Harter P, Muallem ZM, Buhrmann C et al (2011) Impact of a structured quality management program on surgical outcome in primary advanced ovarian cancer. Gynecol Oncol 121:615–619
Chang SJ, Bristow RE (2012) Evolution of surgical treatment paradigms for advanced-stage ovarian cancer: redefining 'optimal' residual disease. Gynecol Oncol 125:483–492
Braicu EI, Fotopoulou C, Van Gorp T et al (2013) Preoperative HE4 expression in plasma predicts surgical outcome in primary ovarian cancer patients: results from the OVCAD study. Gynecol Oncol 128:245–251
Chi DS, Bristow RE, Armstrong DK, Karlan BY (2011) Is the easier way ever the better way? J Clin Oncol 29:4073–4075
Winter WE 3rd, Maxwell GL, Tian C et al (2007) Prognostic factors for stage III epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol 25:3621–3627
Winter WE 3rd, Maxwell GL, Tian C et al (2008) Tumor residual after surgical cytoreduction in prediction of clinical outcome in stage IV epithelial ovarian cancer: a Gynecologic Oncology Group Study. J Clin Oncol 26:83–89
Makar AP, Baekelandt M, Trope CG, Kristensen GB (1995) The prognostic significance of residual disease, FIGO substage, tumor histology, and grade in patients with FIGO stage III ovarian cancer. Gynecol Oncol 56:175–180
Brun JL, Feyler A, Chene G, Saurel J, Brun G, Hocke C (2000) Long-term results and prognostic factors in patients with epithelial ovarian cancer. Gynecol Oncol 78:21–27
Bachmann C, Bachmann S, Fehm T et al (2012) Nodal status--its impact on prognosis in advanced ovarian cancer. J Cancer Res Clin Oncol 138:261–267
Kobel M, Reuss A, du Bois A et al (2010) The biological and clinical value of p53 expression in pelvic high-grade serous carcinomas. J Pathol 222:191–198
Chung HH, Lee M, Kim HS, et al. (2017) Prognostic implication of the metastatic lesion-to-ovarian cancer standardised uptake value ratio in advanced serous epithelial ovarian cancer. Eur Radiol 27(11):4510–4515
Mutch DG, Prat J (2014) 2014 FIGO staging for ovarian, fallopian tube and peritoneal cancer. Gynecol Oncol 133:401–404
Lee JW, Cho A, Lee JH et al (2014) The role of metabolic tumor volume and total lesion glycolysis on (1)(8)F-FDG PET/CT in the prognosis of epithelial ovarian cancer. Eur J Nucl Med Mol Imaging 41:1898–1906
Chung HH, Kwon HW, Kang KW et al (2012) Prognostic value of preoperative metabolic tumor volume and total lesion glycolysis in patients with epithelial ovarian cancer. Ann Surg Oncol 19:1966–1972
Pfister D, Porres D, Heidenreich A et al (2016) Detection of recurrent prostate cancer lesions before salvage lymphadenectomy is more accurate with (68)Ga-PSMA-HBED-CC than with (18)F-Fluoroethylcholine PET/CT. Eur J Nucl Med Mol Imaging 43:1410–1417
Vaidyanathan G, McDougald D, Choi J et al (2016) Preclinical Evaluation of 18F-Labeled Anti-HER2 Nanobody Conjugates for Imaging HER2 Receptor Expression by Immuno-PET. J Nucl Med 57:967–973
Einhorn N, Nilsson B, Sjovall K (1985) Factors influencing survival in carcinoma of the ovary. Study from a well-defined Swedish population. Cancer 55:2019–2025
Farias-Eisner R, Teng F, Oliveira M et al (1994) The influence of tumor grade, distribution, and extent of carcinomatosis in minimal residual stage III epithelial ovarian cancer after optimal primary cytoreductive surgery. Gynecol Oncol 55:108–110
Hacker NF, Berek JS, Lagasse LD, Nieberg RK, Elashoff RM (1983) Primary cytoreductive surgery for epithelial ovarian cancer. Obstet Gynecol 61:413–420
Hoskins WJ, Bundy BN, Thigpen JT, Omura GA (1992) The influence of cytoreductive surgery on recurrence-free interval and survival in small-volume stage III epithelial ovarian cancer: a Gynecologic Oncology Group study. Gynecol Oncol 47:159–166
Berek JS (2009) Lymph node-positive stage IIIC ovarian cancer: a separate entity? Int J Gynecol Cancer 19(Suppl 2):S18–S20
Hofman MS, Hicks RJ (2016) How We Read Oncologic FDG PET/CT. Cancer Imaging 16:35
Cairns RA, Harris IS, Mak TW (2011) Regulation of cancer cell metabolism. Nat Rev Cancer 11:85–95
Chi DS, Abu-Rustum NR, Sonoda Y et al (2004) The benefit of video-assisted thoracoscopic surgery before planned abdominal exploration in patients with suspected advanced ovarian cancer and moderate to large pleural effusions. Gynecol Oncol 94:307–311
Cohen-Mouly S, Badia A, Bats AS et al (2009) Role of video-assisted thoracoscopy in patients with ovarian cancer and pleural effusion. Int J Gynecol Cancer 19:1662–1665
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number : HI14C1072).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Gi Jeong Cheon.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Ethical approval
Institutional Review Board approval was obtained.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Study subjects or cohorts overlap
Data from 73 patients in a previous study were included in the current analysis [14]. This study is different from previous one in that it performed lesion-specific analysis.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Chung, H.H., Kim, JW., Park, NH. et al. Prognostic importance of peritoneal lesion-to-primary tumour standardized uptake value ratio in advanced serous epithelial ovarian cancer. Eur Radiol 28, 2107–2114 (2018). https://doi.org/10.1007/s00330-017-5194-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5194-0