Abstract
Purpose
To evaluate the radiation doses delivered during volumetric helical perfusion CT of the thorax, abdomen or pelvis.
Materials and methods
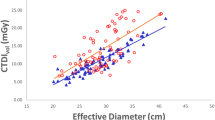
The dose-length product (DLP) and CT dose index (CTDIvol) were recorded and effective dose (E) determined for patients undergoing CT (4D adaptive spiral) for tumour evaluation. Image noise and contrast to noise (CNR) at peak enhancement were also assessed for quality.
Results
Forty two consecutive examinations were included: thorax (16), abdomen (10), pelvis (16). Z-axis coverage ranged from 11.4 to 15.7 cm. Mean DLP was 1288.8 mGy.cm (range: 648 to 2456 mGy.cm). Mean CTDIvol was 96.2 mGy (range: 32.3 to 169.4 mGy). Mean effective dose was 19.6 mSv (range: 12.3 mSv to 36.7 mSv). In comparison mean DLP and effective dose was 885.2 mGy.cm (range: 504 to 1633 mGy.cm) and 13.3 mSV (range: 7.8 to 24.5 mSv) respectively for the standard staging CT thorax, abdomen and pelvis. Mean tumour CNR at peak enhancement was 1.87.
Conclusion
The radiation dose imposed by perfusion CT was on average 1.5 times that of a CT thorax, abdomen and pelvis. The dose is not insubstantial, and must be balanced by the potential clinical utility of additional physiologic data. Further efforts towards dose reduction should be encouraged.

Similar content being viewed by others
References
Mettler FA, Bhargavan M, Faulkner K et al (2009) Medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources—1950–2007. Radiology 253:520–531
Miles KA, Griffiths MR (2003) Perfusion CT: a worthwhile enhancement? Br J Radiol 76:220–231
Miles KA (2003) Perfusion CT for the assessment of tumor vascularity: which protocol? Br J Radiol 76:S36–42
Mnyusiwalla A, Aviv RI, Symons SP (2009) Radiation dose from multidetector row CT imaging for acute stroke. Neuroradiology 51:635–640
Wang J, Wu N, Cham MD, Song Y (2009) Tumor response in patients with advanced non-small cell lung cancer: perfusion CT evaluation of chemotherapy and radiation therapy. AJR Am J Roentgenol 193:1090–1096
Meijerink MR, van Cruijsen H, Hoekman K et al (2007) The use of perfusion CT for the evaluation of therapy combining AZD2171 with gefitinib in cancer patients. Eur Radiol 17:1700–1713
Ng QS, Goh V, Milner J et al (2007) Effect of nitric-oxide synthesis on tumour blood volume and vascular activity: a phase I study. Lancet Oncol 8:111–118
Ng QS, Goh V, Carnell D et al (2007) Tumor antivascular effects of radiotherapy combined with combretastatin a4 phosphate in human non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 67:1375–1380
Koukourakis MI, Mavanis I, Kouklakis G et al (2007) Early antivascular effects of bevacizumab anti-VEGF monoclonal antibody on colorectal carcinomas assessed with functional CT imaging. Am J Clin Oncol 30:315–318
Faria SC, Ng CS, Hess KR et al (2007) CT quantification of effects of thalidomide in patients with metastatic renal cell carcinoma. AJR Am J Roentgenol 189:378–85
Xiong HQ, Herbst R, Faria SC et al (2004) A phase I surrogate endpoint study of SU6668 in patients with solid tumors. Invest New Drugs 22:459–466
Willett CG, Boucher Y, di Tomaso E et al (2004) Direct evidence that the VEGF-specific antibody bevacizumab has antivascular effects in human rectal cancer. Nat Med 10:145–147
Thomas JP, Arzoomanian RZ, Alberti D et al (2003) Phase I pharmacokinetic and pharmacodynamic study of recombinant human endostatin in patients with advanced solid tumors. J Clin Oncol 21:223–231
Huda W, Ogden KM, Khorasani MR (2008) Converting dose-length product into effective dose. Radiology 248:995–1003
Task Group on Control of Radiation Dose in Computed Tomography (2000) Managing patient dose in computed tomography. A report of the International Commission on Radiological Protection. Ann ICRP 30:7–45
Mettler FA, Huda W, Yoshizumi TT, Mahesh M (2008) Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology 248:254–63
Shrimpton PC, Hillier MC, Lewis MA, et al (2003) Doses from computed tomography (CT) examinations in the UK-2003 review. National Radiation Protection Board, UK NRPB-W67
Radiological protection in medicine (1996) ICRP Publication 73. Ann ICRP 26(2)
European Commission (2000) European guidelines on quality criteria for computed tomography. EUR 16262 EN. Office for Official Publications for the European Communities, Luxembourg
Goetti R, Leschka S, Desbiolles L et al (2010) Quantitativecomputed tomography liver perfusion imaging using dynamic spiral scanning with variable pitch: feasibility and initial results in patients with cancer metastases. Invest Radiol 45:419–26
Kalva S, Sahani DV, Hahn PF, Saini S (2006) Using the K-edge to improve contrast conspicuity and to lower radiation dose with a 16-MDCT: a phantom and human study. J Comput Assist Tomgr 30:391–397
Recommendations of the international commission on radiological protection, 60 (1990). ICRP Publication 60. Ann ICRP 21(1–3)
Recommendations of the international commission on radiological protection, 103 (2008). ICRP Publication 103. Ann ICRP 37(2–4)
Wiesmann M, Berg S, Bohner G, Klingebiel R, Schöpf V, Stoeckelhuber BM, Yousry I, Linn J, Missler U (2008) Dose reduction in dynamic Perfusion CT of the brain: effects of the scan frequency on measurements ofcerebal blood flow, cerebeal blood volume and mean transit time. Eur Radiol 18:2967–74
Martin CJ (2007) Effective dose: how it should be applied to medical procedures? Br J Radiol 80:639–647
Medical Services Agency (2010) Im-PACT CT patient dosimetry calculator version 1.01 q. Medical Devices Agency, London, UK
Basic anatomical and physiological data for use in radiological protection: reference values (2002) Annals of the ICRP Publication 89 Annals of the ICRP 32:64
Acknowledgements
We thank Ernst Klotz for his advice and comments, and Siemens Healthcare for their support with perfusion CT software provision.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Conversion factor for Dose Length Produce (DLP) to Effective dose (E)
The rationale for the use of the conversion factors for Dose Length Produce (DLP) to Effective dose (E) for the CTs acquired at 80 kV/100 kV in this study is explained further in this Appendix.
The conversion factor is dependent on the dose to the various specific radiosensitive organs as specified in ICRP 103[23]. The ImPACT calculator (pre-release version 1.01 [26]) calculates these organ doses from both the primary and scattered x-rays using Monte Carlo techniques. The calculator enables beam qualities specific to the acquisition (CT model and kV), and the section of the body irradiated to be entered into the calculation. The ImPACT calculator then multiplies the organ doses by tissue weighting factors as specified by ICRP 103 to give an effective dose.
The calculator is however designed for a conventional CT mode, where the dose in the craniocaudal direction is uniform, and not a ‘shuttle’ mode as in the case of the 4D adaptive spiral mode. Thus the potential non-uniformity of the acquisition dose was investigated initially to ensure that use of the calculator was appropriate. The measured normalized variation of dose with the 4D adaptive spiral (11.4 cm z-axis coverage) is shown in Fig. 2. The measured dose profile shown in Fig. 2 demonstrates a uniform distribution, and this indicates that substantial errors will not be introduced by assuming a uniform dose distribution in our calculations for the 4D adaptive spiral mode.
The 4D adaptive spiral mode uses a primary beam of a relatively short irradiated length (12.4–14.5 cm). The organ doses for each type of scan, chest, abdomen, pelvis will depend on the exact location of the CT primary beam relative to the ICRP radiosensitive organs. As the position of the tumor, and scan location will vary from patient to patient, this variation was investigated for each of the body areas imaged (thorax, abdomen, pelvis).
Appropriate values for CT (Siemens Definition), body area (chest, abdomen, pelvis), kilovoltage (80,100,100 kV), mean CTDI (51.9, 110.5, 131.5 mGy) and irradiated scan lengths, defined as the value of DLP/CTDI (13.8, 14.5, 12.4 cm) were entered into the ImPACT dose calculator. A range of conversion factor values, E/DLP, were found for chest, abdomen and pelvis scans as the position of the centre of the scan was incremented by 1 cm along the body. The results are summarized in Table 5:
In addition to confirm that the use of the imPACT calculator was appropriate, measured organ doses were compared to organ doses calculated by the imPACT software (Fig. 3). To perform this, a number of calibrated thermo luminescent dosemeters (TLDs) were place in an anthromorphic phantom (male ART pelvis) at the following organ sites: colon, bladder and skin. The phantom was scanned using the standard pelvis volumetric helical perfusion CT protocol with the centre of the scan directly over the centre of the bladder. The comparison of calculated and measured organ doses are shown in the Table 6.
The mean measured organ doses for colon and bladder were less than that for the imPACT calculator, by about 20%. This may be due to the exact positioning of the TLDs and the size of the anthromorphic phantom. These measurements indicate that the use of the imPACT calculator for the relevant scan parameters is unlikely to underestimate the organ doses, and hence effective dose and conversion factor E/DLP. The measured skin dose did not correlate to the calculated dose as it is the maximum skin dose, as opposed to the skin dose averaged over all the body as given by the calculator. An average skin dose, 11 mGy, estimated as the ratio of the skin in the primary beam to the skin area of the whole body (ICRP 89 [27]) was less than the dose given on the imPACT calculator, as this simple estimate does not include scattered radiation. The maximum skin dose does however indicate that the skin dose is well below a threshold dose for deterministic effects.
In summary the conversion factors used for the thorax, abdomen and pelvis were the average values 0.019, 0.018 and 0.012 mSv/mGy.cm (range 0.009–0.022) respectively, derived as shown in Table 5. A further uncertainty when determining organ doses and effective dose given by the imPACT dose calculator, is that the results are only valid for a standard mathematical phantom, representing a 70 kg person.
Rights and permissions
About this article
Cite this article
Goh, V., Dattani, M., Farwell, J. et al. Radiation dose from volumetric helical perfusion CT of the thorax, abdomen or pelvis. Eur Radiol 21, 974–981 (2011). https://doi.org/10.1007/s00330-010-1997-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-010-1997-y