Abstract
Aim/purpose
Extreme congenital club foot deformities are common in developing countries, presenting at birth, persisting in children, adolescents and adults; as untreated/under-corrected by conservative and/or surgical means. Scores of confusing names exist in literature for such deformities with no good treatment available; mostly advocating unacceptable arthrodesis. The author researched this grey area for more than 40 years and successfully innovated improved surgical corrections, more acceptable to patients.
Methods
All were given a generic name: “extreme deformities”, with 3 hierarchic grades. each 3D (trimorphic) because of their common aim: a good correction. The author started with anatomical dissections in clubfeet (zero cost), consistently reinforced with solid clinical background. Heterogeneous skin contractures, congenital with/without scars, were discovered as the primary cause with cramped deeper tissues and evolved, evidence based, 3D enlargement of skin chamber by triple expanding incisions: DOrso-LAteral Rotation skin flap (DOLAR- acronym) for grade I, DOLAR + Z-plasty (DOLARZ) for grade II and DOLAR + Z + VY-plasty (DOLARZ-E) for grade III, E means Extended. Patient satisfaction level (excellent, good, fair/poor) had been considered for grading results, rather than scoring systems because each clubfoot is different with countless variables.
Results & conclusions
The author operated 1080 feet during the last 40 years with long term follow up, six months to 30 years, with an average of 12½ years. The results obtained were: excellent/good (96%) and fair/poor (4% including superficial skin necrosis only in 3%, evidence based). Triple surgical skin expansion consistently resulted in longer, flexible, joints sparing, good shaped, better functioning foot; even in adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction & review of literature
Congenital club foot is common, but remains unsolved and the literature quotes up to 95% incidence of residual adduction and inversion, Tarraf & Carroll [9]. There are numerous, diverse, confusing, terms in the literature, e.g. neglected, recurrent, relapsed, residual, resistant, recalcitrant, severe, rigid, syndromic, isolated, with/without surgical scars, from child to adults etc., having commonality in treatment failures. Millions of DALYs are wasted with clubfoot related GBD [17], especially in developing countries. The author has been researching in this grey area for more than 40 years, achieving a breakthrough. A generic name “extreme deformities” has been given to multiple terms describing severe/rigid deformities, having three hierarchic grades each 3D (trimorphic): Gr1 having partially flexible joints mostly children; Gr2 slightly mobile joints, mostly adolescents/adults and Gr3 with little or no mobility, mostly adults; with some overlapping. Incomplete understanding of complex 3D patho-anatomy, primarily of skin and consequently deeper tissues, has been considered responsible for all failures (Table 1).
This research is in three stages/generations, with distinct timeline and completely evidence based. First generation technique in two parts: Part 1 was started around the mid-1970s by studying the patho-anatomy of clubfeet in stillborn foetuses, from skin to deeper tissues with double purpose: Firstly, to clarify reported patho-anatomical controversies; some blaming muscle defects primarily [7, 22], others attributing bones [10, 19] or combined muscles/bones [3, 20, 24] and still others TN subluxation/dislocation [20, 24], but none mentioning skin; secondly, to consolidate opinion about anatomical hurdles causing failures. Fifteen clubfeet were dissected, 16 was the highest number reported till then [19], mostly one or two dissections. Skin contracture in 3D with smaller room was discovered as the primary cause and jammed soft tissues/osteo-articular structures as secondary, which was constantly reinforced with clinical innovations. Without skin expansion, deeper correction is unthinkable. Subcutaneous skin expanders implantation have been reported in clubfoot with limited role in children [18], not in extreme deformities. Part II: A new surgical technique, DOrsoLAteral Rotation skin flap (DOLAR) in Gr1 deformities, expanded skin in 3D, permitting extensive soft tissue release with comfortable realignment of deeper tissues. Anatomical dissections/clinical case series were documented in reputed peer reviewed journals [IJO1981;15-2;129-35 & JFAS(AP)2014;1(2):72-77] and author recieved the best original research award in 1988 from Indian orthopaedic association. Al-Khooly etal 2013 [26] cited with complete reference in their bibliography and successfully used surgical technique of author's 1st Gen i.e. DOrsolateral LAteral Rotation (DOLAR) skin flap (Internat orthop- SICOT 1987) for correction of resistant clubfeet, but maintained initially for 4 weeks with an external fixator instead of plaster cast, with excellent/good results. Others cited this report and used modified fascio-cutaneous flaps and reported with limited role in children only and not in extreme deformities [11,13].
Second generation technique: With increasing awareness, Gr2 extreme deformities in older children/adolescents/adults started presenting for treatment. The focus was again on further 3D skin expansion, incorporating one to three Z-plasties in DOLAR incision depending upon severity, with more extensive deeper dissection. Triple arthrodesis could be avoided in the majority. This was named the DOLARZ technique (DOLAR + Z-plasty). A large series was completed with long term follow up and highly satisfied patients. The author received another National Award from Indian Orthopaedic Association in 2013 and published an article in International journal [Int Orthop 1987;11(3):189-92.PMID:3623754].
Third generation technique: With more awareness, Gr3 deformities in children, adolescents and adults with scars/other complications, started presenting. Therefore, V-Y plasty was added to DOLAR + Z incision (three-in-one expansile incision), besides additional procedures: a small Thiersch graft, a distant relaxing incision and non-skin surgical steps. Hence, this was named DOLARZ-E, E stands for extended.
The literature is full of reports with innumerable conservative/surgical procedures and their modifications. Ponseti’s casting technique with percutaneous TA tenotomy [17], is good if started within the first month, with the right regimen and long term bracing in small children only, but not in extreme deformities. Others having limited role in children are PMR, PSTR and CSTR [23,24,25], CC fusion [8], TMT mobilisation [12], TP, Tib.A transplants [7, 23], Illizarov techniques [6]. Complex problems of residual deformities management in childhood operated clubfeet with deteriorating function in adulthood have been highlighted [4]. In extreme deformities, arthrodesis or talectomy have been recommended [4, 17, 24]. Polydactyly and osseous coalitions [5, 21] can also occur with clubfoot, creating difficulties. The primary aim has been to treat, hitherto neglected “extreme deformities”, achieving a longer/flexible foot without fusion with high acceptability.
Material & methods
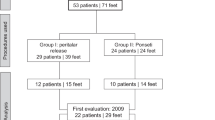
Surgery was performed in varied extreme deformities at all ages, with over 50% older children, adolescents and adults. The earliest age for surgery was about one year (walking age), with the majority of older children (8 years & above), adolescents/adults coming in recent years. Each case was assessed clinically and radiologically by TC angle [2] for TN subluxation/dislocation. Steindler’s plantar release was done in all; modified Evan’s procedure was done mostly after four years, sometimes earlier.
Morbid anatomy & evidence based correction
3D skin contracture
There is abundant evidence: Tight PM & wrinkled DL skin on passive manipulation, surface areas discrepancy on PM and DL aspects; two circles diagram on clubfoot specimen (Fig. 1a), increasing with age, previous surgeries scars, post-trauma increase & occasional unique contracture (corrected by an innovative design, horse shoe shaped MPSTD (Table 1, Fig. 1, case 1 bii-iv,). Correction Gr1: DOLAR skin incision is hockey shaped: semi-circular part over the foot starting near 5th MT base to MM and longitudinal over leg (Fig. 1c, d). A thick fascio-cutaneous flap is raised, meticulously for only 1.5 to 2 cm. All steps of deeper extensive releases: posterior, medial, lateral, SSR, TN reduction and T.M.T mobilisation [12] are executed through this incision. Placement of the first stitch during wound closure is important for maximum PM rotation of skin flap (Fig. 1e). Lateral dog ear is eliminated gradually during wound closure. In Gr2: one or more Z-plasties (DOLARZ) are added in incision on medial side and in Gr3: distal based, V-Y plasties, superficial to deep fascia, are added near ankle region (DOLARZ-E), when wound closure is not possible after excising scar (Fig. 1g, h-j).
a-j: a- A 2 circle diagram on dissection specimen showing medial skin contracture; bi-iv Table 1 case 1 - A Gr 3 unique clubfoot with additional distal plantar skin contracture, corrected by 3 stage surgery: i. DOLAR, ii. plantar VY plasty by an innovative DMPSTD and iii. Minor vy for 2nd toe at one year follow up and iv. at four years follow up; c,d&e- DOLAR incision on DL & medial side with first stitch placement; f- Foot skeleton explaining 5 grades of equinus (FDs); EQ1 to EQ5: EQ1 FD at ankle, EQ2 FD at heel, EQ3 FD at IT & TMT joints (cavus), EQ4 is FD MP & IP joints and EQ5 is oversized talus vis-a-vis ankle joint; g- DOLARZ incision- DOLAR +2 Z plasties; h- An extreme clubfoot with extensive scars; i- Excised extensive scars and DOLARZ-E incision; j- DOLAR + Z + VY plasty, wound closure as well as a K-wire in situ to correct extreme cavus & HV
Muscular contractures
Abductor hallucis, smaller but hypertrophied (Fig. 2c), is slid forward. Gastrosoleus- contracted, hypertrophied, belly extending low, calcaneal TA insertion fan shaped/more medial. Importantly, TP is hypertrophied/contracted. Its nine bony insertions, pulling in 3D towards MM, become crowded, navicular coming closer to ST, pushing talus laterally. Pull of the anterior end of calcaneum medially by TP, complements varying degree of TN dislocation with decreased or zero TC angle (Fig. 2k, l). Adaptative changes in bones with age further increase the deformity. FDP and FHL, short muscles and plantar aponeurosis, are contracted. Correction: Gastrosoleus is corrected by TA Z-plasty, cutting the medial calcaneal half. Dissect/divide all nine insertions of TP (Fig. 2d) facilitating opening all the I.T and TMT spaces of clenched foot. FDP and FHL are divided at Henry’s knot, besides Steindler’s release for FDB & plantar aponeurosis.
a-m: a&b- X-rays lat views (Table 1 case 2) bilateral severe EQ3 (acute cavus); c- Hypertrophied abductor hallucis muscle; d- Intraop showing dissected out nine TP insertions in an adult; e&f- Under-corrected clubfoot with GR; correcting itself by foot Op. g- Hidden equinus after Ponseti’s percutaneous cut TA; h- Divided CPC & opened both subtaloid & ankle joints, inset with corrected hidden equinus; i&j- Dissected specimens normal & deformed feet showing two subtalar articular areas in deformed foot (navicular touching ST) & three areas in normal foot; k&l- A dissected specimen showing TN dislocation with zero TC angle; m- Gr3 residual EV, scar & hallux varus
Ligamentous & capsular contractures
A. CPC of ankle & subtaloid joints: Posterior capsule, PPDL and PTFL, the trio form a contracted/continuous sheet spanning both joints; producing rigid hidden heel equinus, which is improperly understood. Five examples are: a: Rocker bottom foot in serial casting, b: break at weaker point on treating by Ex. Fix. c: GR in under-corrected clubfoot (Fig. 2e), d: decreased TC angle in lateral skiagram and e: after TAL, feet plantigrade on standing, but sitting with knees flexed causes heel raised from ground as hidden equinus (Fig. 2g). In contrast, normally feet are fully plantigrade on sitting on feet. Correction: Besides TA lengthening; complete division of CPC, from medial to lateral and opening both ankle & subtaloid joints will correct hidden equinus too (Fig. 2h/inset).
B. Spring (PCN) ligament- Normally, it is a triangular structure between S.T and navicular supporting talar head underneath at its middle articular area (Fig. 2i). In clubfoot PCN ligament is contracted with navicular touching ST with cavo-varus & TN dislocation (Fig. 2j–l). Correction: complete division from lateral to medial side restores spring ligament space, correcting cavo-varus and TN reduction.
C. ITC ligament (lateral contracture) evidence: Decreased TC angle by rotation of calcaneum & talus in opposite directions due to pull of TP (Fig. 2l). Correction: Divide it in the sinus tarsi from lateral side by a tenotomy knife, blindly, from anterior to posterior, making talus sufficiently manipulable, but not completely, to restore TC angle. This is called subtotal subtalar release (SSR).
D. Other IT, TMT, MP & IP ligamentous contractures evidence: After TP and other releases, crowded bones with cavus-varus, including HV still persist, seen in skiagrams and photographs (Fig. 2a,b,m). Correction: Divide them as required to open up all clenched foot joints.
a-c: Table 1 case 2 ai-vi: photographs Gr3 BL extreme defs in 2½ Y MC with big Callosities & GR; X-rays showing CC, TN disls with acute varus; post-op photographs and foot prints showing excellent correction; Table 1 case 3 bi-vi: photos Gr3 BL defs 7YFC showing extreme equinus > in Rt foot – forefoot at right angle, Intraop DL cuboid wedge removal & (Rotation + Z + VY)- DOLARZ-.E excellent result on standing, shapes of feet with scars & foot prints;Table 1 case 5 ci-v:Photographs 9YMC, Gr3 def Rt, big callos, KFS with webbing neck undescended testis hypoplastic LL, X-rays with CC, TN Disls compared with normal, post-op excellent correction by DOLARZ-E. Excellent correction, standing position and a close up of foot with scars and foot prints
TN. Subluxation/dislocation
Most often present, but not always. Evidence (Fig. 2a,b,l). Correction: After all releases, talar head is pulled medially by curved artery forceps, navicular pushed laterally in front of talar head, TC angle & spring ligament space restored and navicular fixed with K-wire from front with talus. This further increases medial foot length. After TN reduction, severe medial cavus with cock-up great toe (EQ3&4) is corrected by K-wire fixation.
CC hump & callosity
It is present since birth in extreme deformities callosity forms due to weight bearing, increasing with age (Figs. 2j and 3ai&bi). Correction: Modified Evan’s, i.e., D.L. wedge is excised of from cuboid & sometimes other tarsals (joints sparing). Only S.TC is ineffective over four years sometimes even in younger children.
Equinus
Conventionally defined as PF at ankle, has been viewed as a complex deformity in a new perspective, comprising five hierarchic components: i. PF at ankle, ii. At heel (hidden equinus), iii. At IT & TMT joints (cavus), iv At MP & IP joints and v. Rarely over-sized talus vis-à-vis ankle mortis in old/severe deformities (Figs. 1f- EQ. 1-5 and 5di-ii). All level PFs, i.e. EQ. 1-5, need correction for fully plantigrade foot. Correction: the majority can be corrected without triple arthrodesis by triple techniques. Only Gr3 long standing deformities in adults, especially scarred or extensive coalitions will need fusions.
Complications/problems
These are additional congenital defects: coalitions, polydactyly, constriction bands etc. In uncorrected or under-corrected cases: hallux varus, clumsy gait, low/no earning capacity, marital problems (before or after marriage), painful walking (inflamed bursa, callosity), symptomatic GR with posterior subluxation/painful locking, heterogeneous scars, early O.A knee, hip & spine, after effects of severe trauma, HV, plantar horn and stress fracture. All these have been seen by the author. Correction is need based.
Post-operative management
Well padded BK POP cast is given with foot in under-correction to forestall circulatory embarrassment, fully corrected at two/three fortnightly casts. Total immobilisation is for 2 to 3 months.
Assessment Criteria & Grading of results
Assessment criteria: Patient satisfaction level; based on foot length, flexibility, looks and function has been considered for grading results, rather than any scoring system, because “each clubfoot is different” with evidence based countless variables due to severity, rigidity, differing deformity components at birth, varying with age, diverse surgical scars, additional congenital defects, above complicating issues and radiological under-corrections with normal looking operated foot. There are three patient satisfaction grades: excellent, good and fair/ poor. Results: In about 40 years, 1080 surgeries have been performed with adequate follow up in 800 feet, from six months to 30 years, and in 600 ft more than five years with an overall average of 12½ years. There was excellent/good patient satisfaction in 96%, which included insignificant marginal skin necrosis in 3%, not affecting the results (evidence based- BJPS , 1981, Apr;34(2):215-20). There was fair/poor patient satisfaction in 4% with complications of recurrence/overcorrection with or without infection.
Discussion
Heterogeneous 3D skin contractures, have been considered as the most important obstacles in good correction. These may be only congenital (primary) or complicated with scars (secondary). In a smaller container, the contents have to be squeezed in, like a gymnast in small box or a closed contractured fist. Rotation flap, Z & VY-plasties are popular plastic surgery procedures and have been innovatively used as three-in-one skin expanders in clubfoot, enlarging the skin chamber longitudinally, horizontally and vertically. Addition of V-Y plasties in Gen3 technique is also evidence based on plastic surgery reports PMID 7236984 and many more.
These procedures offer numerous advantages: excising mega scars, better deeper release, restoring osteo-articular relationships, closing DL wedge defect, minimising osseous resections for maximum foot length, retaining mobility without arthrodesis. Unusual neglected cases, common in developing countries are also correctible to improve their psycho-socio-economic status, helping in reducing GBD.
Hypertrophied/contracted TP, with its nine tenacious insertions, has been underestimated. They pull the bones towards MM. It is, therefore, imperative to release all attachments along with CPC, spring, TMT, ITC ligaments & modified Evan’s procedure to realign the talus, including HV. A couple of K-wire fixations are needed to maintain correction. Arthrodesis is mostly avoidable with highly meticulous dissection.
Subtotal subtalar release: Multiple steps of extensive soft tissue/osseous release, meant for repositioning of talus vis-à-vis other bones is acronymed as SSR. Leaving some TC attachments (subtotal) in extreme deformities is considered better than Turco’s PSTR (1971) partial (without lateral) release or Simon’s CSTR, complete release (1985). In SSR, talus is adequately manipulable, more than partial, but less than complete and cannot go out of control. A new perspective for equinus, i.e. flexion deformities at five levels, described above, is important for total correction. Rarely, old standing Gr3 deformity in adults with EQ5 in one case, required ITFS division to retrace talus, enabling lesser osseous resections with excellent result (Table 1: case 14, Fig. 5d1,d2).
Unusual complications: AMC defies all corrections [1], a complicated adult AMC with plantar horn, was corrected by these techniques (Table 1: case 12 ci-viii). Another unique case, probably the first one in a literature review, with eight toes, IT & TMT coalitions and many other defects (octopus clubfoot) has been corrected with a highly satisfied patient in spite of 2½” limb shortening (Fig. 4 Table 1: case 8bi-ix) Fig. A case of stress fracture too has been corrected with high patient satisfaction (Table 1:case 9, Fig. 4ci-iv). GR, a compensatory postural mechanism in under-corrected clubfoot with unsightly gait, may have severe knee symptoms and early OA and need correction. Two cases with significant knee symptoms had correction of feet, knees also got corrected (Table 1:case 7, Fig. 2e&f. Traumatic ischaemic rigidity or osseous coalitions with healed scars, are easily corrected by these techniques (Table 1, Fig. 5: cases 14 di,ii/case 15, ei-v). They all need correction, having tremendous physico-psycho-socio-economic problems for family and society.
Table 1a-c: case 6 ai-vi: Gr3 deformity in 16 YM BL, Lt much > Rt with GR adherent highlighted scars. Corrected by DOLARZ & a small PTSG (encircled), excellent result patient standing; Case 8 bi-ix: A unique Gr3 syndromic deformity with 8 eight toes in 18 YF Lt, IT & TMT coalitions, 2½" short & Wasted LL, ankle mobile, WSD, bizarre foot print — named octopus clubfoot (like octopus), Intraop. DOLARZ-E correction (2 insets show excised extra toes & K-wire in GT to correct HV & cavus. Excellent correction, mobile ankle & some TMT joints but 2" short wasted leg & smaller foot, walking with shoe raise at 1YFU. Needs limb lengthening & IT & TMT mobility can also be achieved by undoing coalitions, but patient is highly satisfied even now. Case 9 ci-iv: 24YM GrIII, scars3 Stress # 5th MT in x-ray, unable to walk. Treated by DOLARZ & multiple K-wires fixations. Excellent correction with healing stress # also
Table 1 cases 10,11,12,15&16 a-e: case 10 ai & ii: 23YM Gr3, EQ3, marital problem due to deformity. X-rays preop & postop FU in inset. Excellent correction without any arthrodesis by DOLARZ,1YFU. Case 11 bi-iv: 23YM Gr3, almost 1800 inversion with reversed foot gait & large oblong callosity from LT–LM seen in ellipse as discoloured area, HP leg. X-ray too shows marked inversion. Excellent correction by DOLARZ-E without arthrodesis, at 6 M FU; Case 12 ci-viii: AMC 33YMC, BL DOLAR at 8Y, Rt excellent result, Lt partial due to cong. osseous coalitions, refused 2nd OP that time. Contacted author at 33Y with EQ5, painful PH (encircled), for which GT ray amputated one year back at some other hospital and still unable to walk with deformity & plantar horn. X-ray showed extensive fusion from ankle to all foot bones. Varied DL wedge resections at intertarsal & toe joints with K-wires fixations. Excellent clinical & x-ray correction, nice looking foot & plantigrade foot prints. Patient walking with PTB brace & padded shoes at 1YFU. Case 14 di,ii: BL Gr3 35YM, EQ5, had #s BB both legs & ILNs, defs increased (ischaemic) making walking difficult, compelling painstaking three surgeries each foot with triple arthrodesis. Excellent patient satisfaction at 10 YFU. Case 15 ei-v: Gr3 Rt, complicated by RSA with extensive scars, unstable lateral side skin scar (inset), corrected by DOLARZ-E (rotation + Z+ double VY plasties) & PTSG DL side. Excellent patient satisfaction at 1YFU
Assessment criteria have been based on patient satisfaction level, because “each clubfoot is different” with myriad variables depending upon: deformity components, age, weight bearing, syndromic/ others, previous surgeries, complications, radiological osteo-articular differences (Table1,Case2,CC & TN dislocations). No prevalent assessment criteria can be applicable.
To conclude: I do not find any real weaknesses in this study howover, to discus, it’s weaknesses can be: 1. Longer learning curve, because these techniques are meticulous/time consuming requiring experience; 2. Each clubfoot is different. Just as one size shoes cannot fit all feet, similarly each clubfoot. Each patient requires individual assessment and planning, often requiring ingenuity at the operation table itself; and 3. Foot cannot become normal anatomically, but this is true for other available procedures also.
Its strengths are: 1. Evidence based surgical techniques, consistently reinforced by clinical innovations for more than 40 years; 2. Long term follow up in a large diverse series with high percentage of excellent & good results and no adverse effect on corrections; 3. High patient satisfaction with a longer, flexible without fusion, good looking, better functioning foot and improved socio-economic status; 4. Effective for every type, rarest of the rare clubfoot, at all ages and; 5. The latest innovative addition of V-Y plasty (remaining superficial to deep fascia) in Gen3 technique is completely evidence based with minimal chances of skin necrosis with experience. There are many reports from India and abroad in plastic surgery journals proving good capillaries, arterioles, venules, lymphatics and neural networks deep and superficial to deep fascia with numerous perforators (Ponten B 1981 PMID7326984, Bhattacharya V doi. https://doi.org/10.4103/0970-0358.73424) with cross references. Meticulously performed, the Three-in-One techniques, are completely evidence based achieving the best possible cosmetic and functional corrections with minimal chances of failures.
Abbreviations
- AMC:
-
Arthrogryposis multiplex congenita
- BK:
-
Below knee
- BL:
-
Bilateral
- CPC:
-
Conjoint posterior capsule
- CC:
-
Calcaneo-cuboid
- C:
-
Child
- CSTR:
-
Complete subtalar release
- DL:
-
Dorso-lateral
- Defs:
-
Deformities
- Disls:
-
Dislocations
- DALYs:
-
Disability associated life years
- Ex Fix:
-
External fixator
- EQ1-5:
-
Equinus grades1-5
- Fig.:
-
Figure
- FDL:
-
Flexor digitorum longus
- F:
-
Female
- FHL:
-
Flexor hallucis longus
- FU:
-
Follow up
- Gr1:
-
Grade I
- Gr2:
-
Grade II
- Gr3:
-
Grade III
- GR:
-
Genu recurvatum
- GBD:
-
Global burden of disease
- GEN:
-
Generation
- GT:
-
Great toe
- HV:
-
Hallux varus
- HP:
-
Hypoplastic
- ITFS:
-
Inferior tibiofibular syndesmosis
- ITC:
-
Interosseous talocalcanean
- IT:
-
Intertarsal
- Intraop:
-
Intraoperative
- LT:
-
Little toe
- LM:
-
Lateral malleolus
- M:
-
Male
- MM:
-
Medial malleolus
- M:
-
Months
- MPSTD:
-
Multi-point soft tissue distractor
- OA:
-
Osteoarthritis
- OP:
-
Operation
- PF:
-
Plantar-flexion
- PCN:
-
Plantar calcaneo-navicular
- PPDL:
-
Posterior part deltoid ligament
- PTFL:
-
Posterior talo-fibular ligament
- PMR:
-
Postero-medial release
- PSTR:
-
Partial subtalar release
- Preop:
-
Pre-operative
- PH:
-
Plantar horn
- PTB:
-
Patellar tendon bearing
- SSR:
-
Subtotal subtalar release
- STC:
-
Soft tissue correction
- ST:
-
Sustentaculum tali
- Scars2 :
-
Scars of 2 past surgeries
- 3D:
-
Three dimensional
- TMT:
-
Tarso-metatarsal
- TCN:
-
Talo-calcaneo-navicular
- TA:
-
Tendoachilles
- Tib.A:
-
Tibialis anterior
- TP:
-
Tibialis posterior
- TC:
-
Talo-calcanean
- TN:
-
Talo-navicular
- TAL:
-
Tendoachilles lengthening
- TEV:
-
Talipes equinovarus
- WSD:
-
Wind swipe deformity
- Y:
-
Year
References
Bartlomiej K, Jaroslaw F (2016) Arthrogryposis: an update on clinical aspects, etiology, and treatment strategies. Arch Med Sci 12(1):10–24. https://doi.org/10.5114/aoms.2016.57578
Beatson TR, Pearson JR (1966) A method of assessing correction in clubfoot. J Bone Joint Surg 48-B(1):40–50. http://www.boneandjoint.org.uk/content/jbjsbr/48-B/1/40.full.pdf
Bechtol CO, Mosman HW (1950) Club foot an embryological study of associated muscle abnormalities. J Bone Joint Surg 32-A:827–838
Brodsky JW (2010) The adult sequelae of treated congenital clubfoot. Foot Ankle N Amer 1:287–296. https://doi.org/10.1016/j.fcl.2010.03.002
Eberhardt O, Fernandez FF, Gabriel H, Wirth T, Fuchs-Winkelmann S, Peterlein CD (2014) Clubfoot associated with preaxial polydactyly. J Padtiar Orthop B 23(6):505–511. https://doi.org/10.1097/BPB.0000000000000084
Freedman Jason A, Watts H, Otsuka Norman Y (2006) The Ilizarov method for the treatment of resistant clubfoot: is it an effective solution? J Pediatr Orthop 26(4):432–437. https://doi.org/10.1097/01.bpo.0000226276.70706.0e
Fried A (1959) Recurrent congenital club foot. The role of M. Tibialis posterior in etiology and treatment. J Bone Joint Surg 41-A:243–252
Graham GP, Dent CM (1992) Dillwyn Evans operation for relapsed club foot. Long term results. J Bone Joint Surg (Br) 74-B:445–448
Huang YT, Lei W, Zhao L, Wang J (1999) The treatment of congenital club foot by operation to correct deformity and achieve dynamic muscle balance. J Bone Joint Surg 81-B:858–862
Irani RM, Sherman MS (1963) The pathological anatomy of club foot. J Bone Joint Surg 45-A:45–52
Kamath BJ, Bhardwaj P (2005) Local flap coverage following posteromedial release clubfoot surgery in older children. Int Orthop (Sicot) 29:39–41. https://doi.org/10.1007/s00264-004-0615-5
Kendrick RE, Sharma NK, Hassler W, Herndon CH (1970) Trasometatarsal mobilisation for resistant adduction of fore part of foot. J Bone Joint Surg 52-A:61–70
Lubicky JP, Altiok H (2001) Regional fasciocutaneous flap closure for club foot surgery. J Paediat Orthop 21:50–54
McClure P, Booy D, Katarancic J, Eberson C (2016) Orthopedic manifestations of Mobius syndrome: case series and survey study. Int J Pediatr ID 9736723, 6 pages. https://doi.org/10.1155/2016/973723
McKay DW (1983) New concept of and approach to morbid anatomy (section II) correction of club foot. J Paed Ortho 3:10–21
Penny JN (2005) The neglected clubfoot. Techniques in Orthopaedics; 20(2):153–166. Lippincott, Williams & Wilkins, Philadelphia
Ponseti IV et al (2006) Treatment of the complex idiopathic clubfoot. Clin Orthop Relat Res 451:171–176
Roposch A, Steinwender G, Linhart WE (1999) Implantation of a soft tissue expander before operation in children. J Bone Joint Surg 81-B(3):398–401
Settle GW (1963) The anatomy of congenital talipes equinovarus (sixteen dissected specimens). J Bone Joint Surg 45-A:1341–1354
Simons GW (1985) Complete subtalar release in club feet. J Bone Joint Surg 67-A:1044–1065. https://doi.org/10.1177/107110079201300302
Spero CR, Simon GS, Tornetta P (1994) Clubfeet and tarsal coalition. J Paediatr Orthop 14(3):372–376
Stewart SF (1951) Club foot; its incidence, causes and treatment. An anatomical physiological study. J. Bone Joint Surg 33-A:577–590
Thompson GH, Hoyen HA, Barthel T (2009) Tibialis anterior tendon transfer after clubfoot surgery. Clin Orthop Relat Res 467(5):1306–1313. https://doi.org/10.1007/s11999-009-0757-2
Turco VJ (1979) Resistant congenital club feet. One stage posteromedial release with internal fixation. J Bone Joint Surg 61-A:805–814
Van Gelder JH, Van Ruiten JD, Visser JD, Maathuis PG (2010) Long-term results of the posteromedial release in the treatment of idiopathic clubfoot. J Paediatr Orthop 30(7):700–704. https://doi.org/10.1097/BPO.0b013e3181ec9402
Al-Khooly A, Mohamed M, El-Hawary AE (2013) Treatment of Resistant Clubfoot with Soft TissueRelease and Alkhooly External Fixator," Open Journal of Orthopedics, 3(7):314–320. https://doi.org/10.4236/ojo.2013.37058
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
This article does not contain any studies with human participants or animals performed by the author.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mittal, R.L. Trimorphic extreme clubfoot deformities and their management by triple surgical skin expanders- DOLAR, DOLARZ and DOLARZ-E (evidence based mega-corrections without arthrodesis). International Orthopaedics (SICOT) 42, 1297–1306 (2018). https://doi.org/10.1007/s00264-017-3741-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3741-6