Abstract
Purpose
To assess the accuracy, criteria, and clinical significance of diffusion-weighted imaging (DWI) signal intensity and apparent diffusion coefficient (ADC) quantification for diagnosing acute appendicitis.
Methods
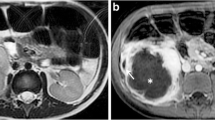
Fifty-one patients with right lower abdominal pain [uncomplicated appendicitis (n = 25), complicated appendicitis (n = 10), and non-appendicitis (n = 16)] who underwent MR examination were enrolled in this retrospective study. Two radiologists independently measured appendiceal diameter and wall thickness. They assessed whether a wall defect, an abscess, extraluminal air, or an appendicolith was present on axial T2WI; evaluated intensity on DWI using a 5-point scale; and determined the ADC values of the appendix and peri-appendiceal tissue. Statistical analysis was performed to assess imaging findings for the diagnosis of appendicitis and complicated appendicitis. Cut-off values were determined using receiver operating characteristic analysis.
Results
For diagnosing acute appendicitis, the accuracy improved from 78.4% using only T2WI to 86.3% using combined T2WI and DWI for reader 1 and from 82.4 to 86.3% for reader 2. For the appendix, the cut-off ADC values that diagnosed appendicitis were 1.41 × 10−3 and 1.26 × 10−3 mm2/s with accuracies of 78.4% and 76.5%, respectively. For the peri-appendiceal tissue, these values of 1.03 × 10−3 and 0.91 × 10−3 mm2/s differentiated between uncomplicated and complicated appendicitis with an accuracy of 97.1%.
Conclusions
Combined DWI and T2WI provided high accuracy for diagnosing appendicitis. The inflamed appendix had lower ADC value than the normal appendix. The peri-appendiceal tissue presenting low ADC value was a notable finding of complicated appendicitis.
Similar content being viewed by others
References
Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT (2015) Acute appendicitis: Modern understanding of pathogenesis, diagnosis, and management. Lancet 386(10000):1278–1287.
Mayumi T, Yoshida M, Tazuma S, Furukawa A, Nishii O, Shigematsu K, et al (2016) The Practice Guidelines for Primary Care of Acute Abdomen 2015. Jpn J Radiol 34(1):80–115.
Garcia EM, Camacho MA, Karolyi DR, Kim DH, Cash BD, Chang KJ, et al (2018) ACR Appropriateness Criteria® Right Lower Quadrant Pain-Suspected Appendicitis. J Am Coll Radiol 15(11S):S373–S387.
Leelakanok N, Phelps AS, Zapala MA, Kato K, Ohliger M, Li Y, et al (2017) Assessing 3D T2 FSE sequence for identification of the normal appendix: working toward a single-sequence MR appendicitis protocol. Emerg Radiol 24(6):653–660.
Noda Y, Goshima S, Kojima T, Kawaguchi S, Kawada H, Kawai N, et al (2017) Improved diagnosis of common bile duct stone with single-shot balanced turbo field-echo sequence in MRCP. Abdom Radiol 42(4):1183–1188.
Iraha Y, Okada M, Iraha R, Azama K, Yamashiro T, Tsubakimoto M, et al (2017) CT and MR Imaging of Gynecologic Emergencies. RadioGraphics 37(5):1569–1586.
Nitta N, Takahashi M, Furukawa A, Murata K, Mori M, Fukushima M (2005) MR imaging of the normal appendix and acute appendicitis. J Magn Reson Imaging 21(2):156–165.
Kinner S, Pickhardt PJ, Riedesel EL, Gill KG, Robbins JB, Kitchin DR, et al (2017) Diagnostic accuracy of MRI versus CT for the evaluation of acute appendicitis in children and young adults. Am J Roentgenol 209(4):911–919.
Repplinger MD, Pickhardt PJ, Robbins JB, Kitchin DR, Ziemlewicz TJ, Hetzel SJ, et al (2018) Prospective Comparison of the Diagnostic Accuracy of MR Imaging versus CT for Acute Appendicitis. Radiology 288(2):467–475.
Eng KA, Abadeh A, Ligocki C, Lee YK, Moineddin R, Adams-Webber T, et al (2018) Acute Appendicitis: A Meta-Analysis of the Diagnostic Accuracy of US, CT, and MRI as Second-Line Imaging Tests after an Initial US. Radiology 288(3):712–727.
Martin JF, Mathison DJ, Mullan PC, Otero HJ (2018) Secondary imaging for suspected appendicitis after equivocal ultrasound: time to disposition of MRI compared to CT. Emerg Radiol 25(2):161–168.
Singh A, Danrad R, Hahn PF, Blake MA, Mueller PR Novelline RR (2007) MR imaging of the acute abdomen and pelvis: Acute appendicitis and beyond. Radiographics 27(5):1419–1431.
Petkovska I, Martin DR, Covington MF, Urbina S, Duke E, Daye ZJ, et al (2016) Accuracy of Unenhanced MR Imaging in the Detection of Acute Appendicitis: Single-Institution Clinical Performance Review. Radiology 279(2):451–60.
Byott S, Harris I (2016) Rapid acquisition axial and coronal T2 HASTE MR in the evaluation of acute abdominal pain. Eur J Radiol 85(1):286–290.
Ditkofsky NG, Singh A, Avery L, Novelline RA (2014) The role of emergency MRI in the setting of acute abdominal pain. Emerg Radiol 21(6):615–624.
Patel D, Fingard J, Winters S, Low G (2017) Clinical use of MRI for the evaluation of acute appendicitis during pregnancy. Abdom Radiol 42(7):1857–1863.
Oto A, Srinivasan PN, Ernst RD, Koroglu M, Cesani F, Nishino T, et al (2006) Revisiting MRI for appendix location during pregnancy. Am J Roentgenol 186(3):883–887.
Pedrosa I, Levine D, Eyvazzadeh A (2006) MR Imaging Evaluation of Acute Appendicitis in Pregnancy. Radiology 238(3):891–899.
Inci E, Kilickesmez O, Hocaoglu E, Aydin S, Bayramoglu S, Cimilli T (2011) Utility of diffusion-weighted imaging in the diagnosis of acute appendicitis. Eur Radiol 21(4):768–775.
Bayraktutan Ü, Oral A, Kantarci M, Demir M, Ogul H, Yalcin A, et al (2014) Diagnostic performance of diffusion-weighted MR imaging in detecting acute appendicitis in children: Comparison with conventional MRI and surgical findings. J Magn Reson Imaging 39(6):1518–1524.
Leeuwenburgh MM, Wiarda BM, Bipat S, Nio CY, Bollen TL, Kardux JJ, et al (2012) Acute appendicitis on abdominal MR images: Training Readers to Improve Diagnostic Accuracy. Radiology 264(2):455–463.
Avcu S, Çetin FA, Arslan H, Kemik Ö, Dülger AC (2013) The value of diffusion-weighted imaging and apparent diffusion coefficient quantification in the diagnosis of perforated and nonperforated appendicitis. Diagnostic Interv Radiol 19(2):106–110.
Martin JF, Mathison DJ, Mullan PC, Otero HJ (2018) Secondary imaging for suspected appendicitis after equivocal ultrasound: time to disposition of MRI compared to CT. Emerg Radiol 25(2):161–168.
Terasawa T, Blackmore CC, Bent S, Kohlwes RJ (2004) Systematic review : computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med 141(7):537–46
Horrow MM, White DS, Horrow JC (2003) Differentiation of Perforated from Nonperforated Appendicitis at CT. Radiology 227(1):46–51.
Foley TA, Iv FE, Nathan MA, Hough DM, Schiller HJ, Hoskin TL (2005) Differentiation of nonperforated from perforated appendicitis: accuracy of CT diagnosis and relationship of CT findings to length of hospital stay. Radiology 235(1):89–96.
Tsuboi M, Takase K, Kaneda I, Ishibashi T, Yamada T, Kitami M, et al (2008) Perforated and nonperforated appendicitis: defect in enhancing appendiceal wall--depiction with multi-detector row CT. Radiology 246(1):142–147.
Kinner S, Pickhardt PJ, Riedesel EL, Gill KG, Robbins JB, Kitchin DR, et al (2017) Diagnostic Accuracy of MRI Versus CT for the Evaluation of Acute Appendicitis in Children and Young Adults. Am J Roentgenol 209(4):911–919.
Pedrosa I, Levine D, Eyvazzadeh AD, Siewert B, Ngo L Rofsky NM (2006) MRI evaluation of acute appendicitis in pregnancy. Radiology 238(3):891–899.
Birchard KR, Brown MA, Hyslop WB, Firat Z, Semelka RC (2005) MRI of acute abdominal and pelvic pain in pregnant patients. Am J Roentgenol 184(2):452–458.
Choe J, Wortman JR, Michaels A, Sarma A, Fulwadhva UP, Sodickson AD (2019) Beyond appendicitis: ultrasound findings of acute bowel pathology. Emerg Radiol 26(3):307–317.
Oto A, Kayhan A, Williams JTB, Fan X, Yun L, Arkani S, et al (2011) Active Crohn’s disease in the small bowel: Evaluation by diffusion weighted imaging and quantitative dynamic contrast enhanced MR imaging. J Magn Reson Imaging 33(3):615–624.
Kiryu S, Dodanuki K, Takao H, Watanabe M, Inoue Y, Takazoe M, et al (2009) Free-breathing diffusion-weighted imaging for the assessment of inflammatory activity in crohn’s disease. J Magn Reson Imaging 29(4):880–886.
Wang A, Shanbhogue AK, Dunst D, Hajdu CH, Rosenkrantz AB (2016) Utility of diffusion-weighted MRI for differentiating acute from chronic cholecystitis. J Magn Reson Imaging 44(1):89–97.
Inoue A (2018) Lower abdominal pain outside of the obstetrics and gynecology. Clinical Imagiology 34(4):449–460.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Inoue, A., Furukawa, A., Nitta, N. et al. Accuracy, criteria, and clinical significance of visual assessment on diffusion-weighted imaging and apparent diffusion coefficient quantification for diagnosing acute appendicitis. Abdom Radiol 44, 3235–3245 (2019). https://doi.org/10.1007/s00261-019-02180-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02180-3