Abstract
Background
Ultrasound is an accurate tool for diagnosing acute appendicitis. Conservative treatment for uncomplicated acute appendicitis is feasible and safe in children. However, no sonographic follow-up results from children with nonoperatively managed acute appendicitis have been reported.
Objective
To describe the sonographic appearance of the appendix at follow-up ultrasound and to attempt to identify signs predictive of recurrent acute appendicitis.
Materials and methods
Children diagnosed with uncomplicated acute appendicitis and treated conservatively in our hospital from 2014 to 2019, and who presented for follow-up ultrasound at 3, 6 and 9 months, were included in our study. Clinical, laboratory and ultrasound data were recorded.
Results
By the end of follow-up, 29 (14.2%) of 204 children in the cohort had developed recurrent acute appendicitis and 175 had recovered uneventfully. On follow-up ultrasound, appendiceal diameter measured > 6 mm in 56/204 (27.5%) cases at 3 months and in 9/26 (34.5%) at 6 months. After 3 months, 102/204 (50%) children had normal appendiceal diameter on ultrasound. Appendiceal diameter > 6 mm was associated with intraluminal fluid or sludge in the appendiceal lumen at 3- and 6-month follow-up (P < 0.001, P = 0.002, respectively). Comparing cases with and without recurrence, at 3-month follow-up, appendiceal diameter > 6 mm was found in 17/29 (58.6%) cases vs. 39/175 (22.3%), respectively (P < 0.001). Appendiceal diameter returned to normal in 12/19 (63.2%) cases in the nonrecurrent acute appendicitis group compared with 2/7 (28.6%) in the recurrent acute appendicitis group (P = 0.05) at the 6-month follow-up. Intraluminal fluid or sludge was detected more frequently in the recurrent acute appendicitis versus the nonrecurrent acute appendicitis group at 3- (P < 0.001) and 6-month (P = 0.001) follow-up.
Conclusion
Progressive normalization of appendiceal diameter was noted on follow-up ultrasound. The prevalence of both appendiceal diameter > 6 mm and intraluminal fluid or sludge were found to be increased in children who later developed recurrent acute appendicitis. Ultrasound appears to be a useful tool for follow-up in children with conservatively treated uncomplicated acute appendicitis and possibly might help predict recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Appendicitis is the most common surgical emergency in children. Overall, acute appendicitis is diagnosed in 1–8% of children presenting to the emergency department with acute abdominal pain [1,2,3,4]. For years, appendectomy has been the treatment of choice. Several studies have evaluated conservative treatment with antibiotics as the first approach for uncomplicated acute appendicitis in children. The findings demonstrated that this treatment modality is safe and feasible for most children, obviating the need for surgery [5,6,7,8,9,10,11,12,13,14,15].
Additional benefits of conservative treatment include a potential decrease in complications and decreased costs [8, 16]. Moreover, parents prefer conservative management for their children due to the fear of surgical risks [8]. Additionally, increased preference for conservative management for acute appendicitis was reported during the COVID-19 pandemic [17, 18].
Ultrasound plays a central role in the diagnostic work-up of children with suspected appendicitis. A stepwise imaging approach that begins with ultrasound and proceeds to computed tomography (CT) or magnetic resonance imaging (MRI) in select cases is considered the best practice [19]. Two meta-analyses of imaging for pediatric appendicitis reported that ultrasound had a sensitivity of 83% and 89% and a specificity of 94% and 97%, respectively [20, 21]. Sensitivity as high as 97% and specificity of 95% were reported from ultrasound studies performed by pediatric radiologists [22, 23].
Information about the usefulness of imaging for follow-up of patients treated nonoperatively for uncomplicated acute appendicitis is limited. We found only one study reporting the use of ultrasound to follow up adults treated conservatively for uncomplicated acute appendicitis. The number of patients analyzed in that study was small (19) and the follow-up period was only 30 days [24].
To the best of our knowledge, ultrasound has not yet been evaluated for the follow-up of children with acute appendicitis managed nonoperatively and sonographic findings after conservative treatment have not been reported. Furthermore, no consistent, reliable ultrasonographic signs have been described to predict recurrent acute appendicitis.
The aims of this study were to evaluate the outcomes of children with an established diagnosis of uncomplicated acute appendicitis treated nonoperatively with antibiotics, to describe the sonographic appearance of the appendix on follow-up ultrasound, to identify ultrasound signs predictive of recurrent acute appendicitis and to assess the reliability of ultrasound as a tool for follow-up of these patients.
Materials and methods
This cohort study was conducted at a tertiary-care medical center. It included children who met the following criteria: admitted to the Pediatric Surgery Department from January 2014 through December 2019, diagnosed with uncomplicated acute appendicitis, received conservative antibiotic treatment and underwent follow-up ultrasound. The clinical records and ultrasound data of these children at presentation and during follow-up were evaluated. Radiologists (R.S., with 17 years’ experience; R.M., a radiology resident, and M.W., with 30 years’ experience) assessed and recorded the following sonographic features: ultrasound-measured appendiceal diameter (classified as > 6 mm or ≤ 6 mm), appendiceal wall thickening (> 3 mm or < 3 mm), presence or absence of intraluminal fluid or sludge, increased echogenicity of periappendiceal fat, periappendiceal free fluid and enlarged mesenteric lymph nodes. The final diagnosis of uncomplicated acute appendicitis was made by a pediatric surgeon (Z.S.) with 28 years of experience based on the clinical, laboratory and ultrasonographic findings. The inclusion criteria for diagnosing a child with uncomplicated acute appendicitis were duration of symptoms < 36 h, Samuel score ≥ 7 and an ultrasound appendiceal diameter 6–10 mm. Samuel score [25] is calculated as the sum of: (1) cough/percussion/hopping tenderness in the right lower quadrant of the abdomen, (2) anorexia, (3) pyrexia, (4) nausea/emesis, (5) tenderness over the right iliac fossa, (6) leukocytosis, (7) polymorphonuclear neutrophilia and (8) migration of pain. Each of these variables were assigned a score of 1, except for physical signs (1 and 5), which were scored 2 to obtain a total of 10 (Online Supplementary Material 1) [25]. Exclusion criteria for conservative management were suspicion of perforated appendicitis, detection of an appendicolith by ultrasound, two previous rounds of conservative antibiotic treatment for acute appendicitis, parental request to operate, appendiceal diameter > 10 mm and symptoms lasting > 48 h before admission. The inclusion and exclusion criteria for conservative antibiotic treatment were based on our experience and are similar to those used in other studies [12, 13, 15]. Parents were informed of the potential advantages and disadvantages of operative and conservative management. Parents consented to include their children in the nonoperative group. Data including clinical signs and laboratory and ultrasound results were collected from all patients who underwent conservative antibiotic treatment. All participants visited the outpatient clinic 4–6 weeks after discharge, with additional follow-up visits every 3 months during the first year after conservative antibiotic treatment and then once annually. The 3-month follow-up included medical history and examination by a pediatric surgeon (Z.S.) as well as ultrasonography. Verbal informed consent was obtained from the parents for follow-up ultrasound. The follow-up studies were performed by an experienced pediatric radiologist (R.S.) from the Department of Imaging or under her direct supervision. The ultrasound studies for the initial diagnosis of uncomplicated acute appendicitis and recurrent acute appendicitis were performed emergently by department radiologists. We reviewed these studies and collected clinical, laboratory and sonographic data.
A Philips Affiniti 70 G machine (Philips Healthcare, Andover, MA) and a GE Logic S8 machine (GE Healthcare, Milwaukee, WI) were used.
The appearance of the appendix was considered normal when it was identified, its diameter was ≤ 6 mm, the thickness of the wall was < 3 mm, air was identified in the appendiceal lumen, no stranding of periappendiceal fat was detected, and minimal or no fluid was in the abdominal cavity. In all cases in which the follow-up ultrasound study was normal or the appendix was not identified, the children underwent further clinical follow-up only. In all cases in which the transverse diameter of the appendix was > 6 mm, surgical evaluation was performed to exclude acute appendicitis. If acute appendicitis was ruled out, another follow-up ultrasound was ordered at 6 months, and depending on the results, further ultrasound studies were performed every 3 months until the appendix appeared normal in size on ultrasound or an episode of acute appendicitis recurred. The end of the follow-up was established as Dec. 31, 2020, with a minimum 1-year clinical follow-up period for patients diagnosed with uncomplicated acute appendicitis in December 2019 and 6 years for patients diagnosed in January 2014.
For patients who did not attend follow-up visits, their parents were interviewed by telephone. To identify patients who underwent appendectomy elsewhere during the follow-up period, we searched the national electronic database that includes all children who are hospitalized for any reason. When data extracted from the computerized notes were considered insufficient, supplemental telephone interviews were conducted. Clinical follow-up was planned according to the ultrasound findings.
Failure of conservative antibiotic treatment was defined as a need for secondary antibiotic treatment or surgical intervention during follow-up. Recurrent acute appendicitis was diagnosed by pediatric surgeons based on clinical, laboratory and ultrasonographic findings. In cases with recurrence, the inclusion and exclusion criteria for conservative antibiotic treatment were similar to those used at the initial diagnosis of uncomplicated acute appendicitis. The parents` preference for surgery versus conservative antibiotic treatment was discussed, and the final decision was made accordingly. Time to recurrence was defined as the period from the date of first follow-up (3 months following uncomplicated acute appendicitis) to the date of recurrence.
Statistical analysis
Data were analyzed with R Version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria). Nominal variables are presented as numbers and percentages; continuous variables are presented as mean ± standard deviation (SD) when normally distributed or as median and interquartile range (IQR) when not normally distributed (Shapiro–Wilk test). Differences between the patient groups with and without recurrent acute appendicitis were analyzed with the chi-square test for categorical variables, Student’s t-test for parametric variables and the Mann-Whitney U test and Welch t-test for nonparametric variables. To assess multivariate models, we conducted logistic regressions to predict recurrent acute appendicitis by the main demographic, laboratory and sonographic variables. These regressions produced odds ratios and 95% confidence intervals [CI]. P-values < 0.05 were considered significant.
Results
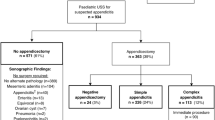
Among the 835 children treated conservatively for uncomplicated acute appendicitis in our hospital, 204 underwent follow-up ultrasound at 3 months and were included in the cohort analysis (Fig. 1). The remaining 631 children were excluded from the study due to failed conservative antibiotic treatment and subsequent appendectomy during hospitalization for the initial episode of uncomplicated acute appendicitis, recurrent acute appendicitis before the scheduled 3-month follow-up ultrasound, parental choice to decline follow-up ultrasound or withdrawal after initial consent (did not present for follow-up ultrasound despite scheduled appointment). Our cohort consisted of 63 girls (30.9%) and 141 (69.1%) boys ranging in age from 3 to17 years (median: 10 years, IQR [8,13]). No significant differences were found between the 631 children excluded and the 204 included in the cohort (Online Supplementary Material 2). Clinical follow-up periods ranged from 1 to 6 years. Figure 1 is a flow diagram of the study.
All children who presented for follow-up ultrasound were asymptomatic, none had focal tenderness at ultrasound or surgical examination and none underwent laboratory investigations at the time of scheduled ultrasonographic studies.
Five of 204 children had a CT scan of the abdomen and pelvis: 4 to confirm the initial uncomplicated acute appendicitis diagnosis and 1 the diagnosis of recurrent acute appendicitis. CT scans were performed at the request of the pediatric surgeons to confirm the ultrasound findings. All CT results were concordant with ultrasound.
The data of the 29 patients who developed recurrent acute appendicitis (at the initial diagnosis, during follow-up or at the time of recurrent acute appendicitis) are presented in Online Supplementary Materials 3 and 4.
Appearance of the appendix on follow-up ultrasound
Data related to the appearance of the appendix at follow-up ultrasound are presented in Table 1. At the 3-month follow-up ultrasound, the appendiceal diameter appeared > 6 mm in 56/204 children (27.5%), was not detected in 46/204 (22.5%) and seemed normal (≤ 6 mm) in 102/204 (50%). An enlarged appendiceal diameter appears to be explained in 17/56 (30.3%) cases by an increase in wall thickness (> 3 mm), in 31/56 (55.4%) by intraluminal fluid or sludge and in 8/56 (14.3%) by both the increase in wall thickness and intraluminal fluid or sludge were found to be in the appendiceal lumen. Intraluminal fluid or sludge was detected more frequently in children with an increased appendiceal diameter than in children with a normal appendiceal diameter (P < 0.001). Of the 56 children with an appendiceal diameter > 6 mm at the 3-month follow-up and scheduled for 6-month follow-up ultrasound, 26 (46.4%) presented for this investigation (6 months from the date of conservative antibiotic treatment); 9 (16.1%) patients had recurrent acute appendicitis before the scheduled 6-month ultrasound (Online Supplementary Material 3) and the remaining 21 (37.5%) patients declined to present for this ultrasound and received clinical follow-up only.
At the 6-month follow-up ultrasound, the appendiceal diameter appeared > 6 mm in 9/26 (34.5%) children, was not detected in 3/26 (11.5%) and appeared normal in size (≤ 6 mm) in 14/26 (54%). The enlarged appendiceal diameter appeared to be due to an increase in wall thickness in three cases, intraluminal fluid or sludge was present in three and increased wall thickness and intraluminal fluid or sludge was in the lumen of the appendix in three. Intraluminal fluid or sludge was detected more frequently in children with an appendiceal diameter > 6 mm (6/9, 66.6%) than in children with an appendiceal diameter ≤ 6 mm (1/14, 7.1%) at 6-month follow-up ultrasound (P = 0.002). The information related to the ultrasound appearance of the appendiceal diameter at the 3- and 6-month follow-ups is summarized in Fig. 2. Overall, after 6 months, 116 (56.8%) children had a normal (≤ 6 mm) appendiceal diameter on ultrasound (102 on the 3-month scan and 14 on the 6-month) and only 9 (4.4%) had an appendiceal diameter > 6 mm documented by ultrasound.
Three of the nine children with an appendiceal diameter > 6 mm at the 6-month follow-up presented for the 9-month ultrasound examination; four children had recurrent acute appendicitis before the scheduled examination (Online Supplementary Material 3) and the remaining two declined to present and were followed clinically. Among the three children who presented for the 9-month ultrasound, the appendiceal diameter was > 6 mm in one and normal in two. The child with the enlarged diameter had recurrent acute appendicitis 10 months from the date of conservative antibiotic treatment (1 month after the 9-month follow-up).
As shown in Fig. 3, the median ultrasound-measured appendiceal diameter at baseline (at the initial diagnosis of uncomplicated acute appendicitis) was 8 mm [IQR 7–9], 5.8 mm [IQR 5.0–6.8] at the 3-month follow-up and 5.9 mm [IQR 5.0–6.5] at the 6-month follow-up. The median appendiceal diameter in the 29 patients with recurrent acute appendicitis was 9 mm [8, 10]. The ultrasound-measured appendiceal diameter in patients were significantly smaller at the 3- and 6-month follow-up visits than at baseline (P < 0.001). In contrast, the appendiceal diameter in patients with recurrent acute appendicitis (measured at the time of recurrent acute appendicitis) was significantly larger than the baseline values (P = 0.012).
Comparison of the demographic and US findings
By the end of the study (Dec. 31, 2020), 29 children (14.2%) had recurrent appendicitis (recurrent acute appendicitis group) and 175 (85.8%) had an uneventful follow-up (nonrecurrent acute appendicitis group). Most of the recurrences (21/29) were seen during the first year, with 5/29 and 3/29 recurrences occurring in the 2nd year and beyond, respectively. The recurrence rate over the first year was 10.3% (21/204), while the rate over the first two years was 12.7% (26/204), with a recurrence rate of 14.2% over the entire study period.
Comparison of the demographic findings
No significant differences in age or sex were found between the recurrent acute appendicitis group (n = 29) and the nonrecurrent acute appendicitis group (n = 175). Children from the recurrent acute appendicitis group had a median age of 11 years (IQR [9, 13)], compared with 10 years (IQR [8, 13]) for the nonrecurrent acute appendicitis group (P = 0.58). The percentages of males in the recurrent acute appendicitis and nonrecurrent acute appendicitis groups were similar (72.4% vs. 68.6%, respectively; P = 0.84). An analysis of different age groups with recurrent acute appendicitis versus those without recurrent acute appendicitis also revealed nonsignificant differences (Online Supplementary Material 5).
Comparison of the US parameters during follow-up
Data related to ultrasound parameters at the 3-month follow-up are presented in Table 2. The median appendiceal diameter (Fig. 4) was significantly larger in the recurrent acute appendicitis group (7 mm, IQR [5.9, 7.5]) than in the nonrecurrent acute appendicitis group (5.5 mm, IQR [5.0, 7.5]; P = 0.003).
An appendiceal diameter > 6 mm was recorded in 17/29 (58.6%) cases in which acute appendicitis recurred and in 39/175 (22.3%) of the cases without recurrent acute appendicitis (P < 0.001). The appendiceal diameter was detected as < 6 mm in 6/29 (20.7%) patients in the recurrent acute appendicitis group and in 96/175 (54.9%) in the nonrecurrent acute appendicitis group (P < 0.001). When patients with an undetected appendix were included with those with an appendiceal diameter < 6 mm on ultrasound, statistical significance was preserved (P < 0.001).
Fluid in the abdomen at the 3-month follow-up ultrasound was more common in children who developed recurrent acute appendicitis than in those who did not (P = 0.052, Fisher exact test P = 0.040). Wall thickness > 3 mm, fat infiltration and lymph node enlargement were not associated with increased risk of recurrent acute appendicitis.
Intraluminal fluid or sludge was recorded in 17/23 (73.9%) cases with a detectable appendix and recurrent acute appendicitis and in 32/135 cases (23.7%) with an identifiable appendix and without recurrent acute appendicitis (P < 0.001).
As shown in Fig. 5, at the 3-month follow-up ultrasound, intraluminal fluid or sludge associated with an appendiceal diameter > 6 mm was seen more frequently in children with recurrent acute appendicitis (16/17) than in children without recurrent acute appendicitis (23/39) (P = 0.008). Additionally, as shown in Fig. 5, fluid in the abdomen in association with an enlarged appendiceal diameter appears to be detected more frequently in the recurrent acute appendicitis than in the nonrecurrent acute appendicitis group (P = 0.078, Fisher exact test P = 0.046).
Data related to the ultrasound parameters at the 6-month follow-up are presented in Table 3.
Among the 26 children who underwent 6-month follow-up, 7 developed recurrent acute appendicitis and 19 remained asymptomatic. The appendiceal diameter returned to normal (≤ 6 mm) in 12/19 (63.2%) cases in the nonrecurrent acute appendicitis group compared to 2/7 (28.6%) in the recurrent acute appendicitis group (P = 0.05). The appendix could not be identified in 3/19 (15.8%) cases from the nonrecurrent acute appendicitis group and the diameter remained > 6 mm in 5/7 cases from the recurrent acute appendicitis group (71.4%) vs. 4/19 (21.1%) from the nonrecurrent acute appendicitis group (P = 0.05). When we repeated the analysis adding patients with an undetected appendix to the group with a normal-appearing appendix, the difference approached statistical significance (P = 0.054).
At the 6-month follow-up, intraluminal fluid or sludge was recorded in 5/7 (71.4%) cases with a detectable appendix and recurrent acute appendicitis and in 2/16 (12.5%) cases with an identifiable appendix and without recurrent acute appendicitis (P < 0.001).
At 9 months, the appendiceal diameter was 8 mm in the child who eventually developed recurrent acute appendicitis and contained intraluminal fluid or sludge. In contrast, it was < 6 mm by that time in the two children who remained asymptomatic.
Association of the US parameters at 3-month follow-up and the treatment for recurrent acute appendicitis
Recurrent acute appendicitis was treated surgically in 23 cases and nonoperatively in 6. The data related to the appendiceal diameter at the 3-month follow-up ultrasound and the type of treatment for recurrent acute appendicitis are presented in Table 4.
The data related to intraluminal fluid or sludge at the 3-month follow-up ultrasound and the type of treatment for recurrent acute appendicitis are presented in Table 5.
The need for surgical treatment was more common in children with an appendiceal diameter > 6 mm at the 3-month follow-up ultrasound than in children with a normal size or unidentified appendix. Additionally, the need for surgery was more common among children with intraluminal fluid or sludge in the appendiceal lumen at 3-month follow-up ultrasound than in children without this finding.
Comparison of the US parameters at the initial diagnosis of uncomplicated acute appendicitis
Data related to the ultrasound findings at the initial diagnosis of uncomplicated acute appendicitis in children who developed recurrent acute appendicitis versus those who did not are presented in Table 6.. No significant association was found between the appendiceal diameter at initial diagnosis and the risk of recurrence. Intraluminal fluid or sludge was detected at the initial uncomplicated acute appendicitis diagnosis in 17/29 (58.6%) children who developed recurrent acute appendicitis compared with 44/175 (25.1%) who did not (P = 0.002). None of the other ultrasound parameters used at the initial diagnosis of uncomplicated acute appendicitis (free fluid in the peritoneal cavity, fat infiltration, lymph node enlargement, thickening of the appendiceal wall) was associated with increased risk of recurrent acute appendicitis.
Predictive multivariate models
The results of the logistic multivariate regressions predicting recurrent acute appendicitis based on the main demographic, laboratory and sonographic variables at diagnosis and 3-month follow-up visits are presented in Table 7. The regression model for 6-month follow-up consisted of very few observations; therefore, no coefficients were produced.
Results show that, after adjusting other variables, at both the diagnosis (odds ratio [OR = 4.030, 95% [CI] [1.663, 9.765]) and 3-month follow-up visits (OR = 13.56, 95% CI [4.069, 45.248]), intraluminal fluid or sludge predicted recurrent acute appendicitis.
Discussion
Most studies dealing with conservative antibiotic treatment for uncomplicated acute appendicitis have focused on the success of treatment [5, 14, 15, 26]. Others have tried to predict recurrence using clinical, laboratory and US data at initial diagnosis [12, 13, 27, 28]. To the best of our knowledge, there are no reports providing information about the usefulness of imaging for follow-up of children treated conservatively for uncomplicated acute appendicitis. Our study addressed this issue and assessed the appearance of the appendix on follow-up ultrasound after conservative antibiotic treatment for uncomplicated acute appendicitis in children.
By the end of the follow-up period, 29 (14.2%) children had developed recurrent acute appendicitis and 175 had recovered uneventfully. The 14.2% recurrence rate reported by our group corroborates previous reports in the literature, such as the 14% adjusted incidence rate for recurrent appendicitis calculated by Georgiou et al. [7].
The ultrasound-measured appendiceal diameters of our patients were significantly smaller at the 3- and 6-month follow-up visits than at baseline (P < 0.001). In contrast, the appendiceal diameter of patients with recurrent acute appendicitis (measured at the time of recurrent acute appendicitis) were significantly larger than the baseline values (P = 0.012). This information can be valuable for understanding the expected dynamics of appendiceal diameter measurements during the management and follow-up of children treated conservatively for uncomplicated acute appendicitis.
We observed that the appendiceal diameters were already ≤ 6 mm in 50% of cases at the 3-month follow-up. The recovery rate continued to increase progressively during follow-up in accordance with the clinical evaluations. We consider these findings a useful adjunct for choosing conservative antibiotic treatment successfully and for further clinical decision-making.
At the 3-month follow-up ultrasound, in 27.5% of cases, the appendiceal diameter remained increased in size despite the absence of symptoms. Our results also showed that detection of an appendiceal diameter > 6 mm and intraluminal fluid or sludge at follow-up ultrasounds were more frequently associated with recurrent acute appendicitis.
This information can also be helpful for surgeons and other medical personnel involved in the management and follow-up of children with uncomplicated acute appendicitis treated nonoperatively. In the absence of symptoms, an appendiceal diameter > 6 mm on 3-month follow-up ultrasound does not appear to be an indication for immediate treatment or diagnostic work-up, as the appendix was normal size (< 6 mm) in 54% of the children who had an additional ultrasound at 6 months. For some children, an increased appendiceal diameter at the 3-month follow-up probably indicates that they need additional time for the appendix to heal and for the inflammatory changes to recede, but for others, it can be an indicator of increased recurrence risk. We recommend that an enlarged appendiceal diameter on follow-up ultrasounds, months after an episode of uncomplicated acute appendicitis, must be interpreted with caution and in correlation with the clinical and laboratory findings.
At the 6-month follow-up, an appendiceal diameter > 6 mm continued to be present more frequently among children who developed recurrent acute appendicitis (71.4%) than among those who did not (21.1%). Therefore, it is possible to consider that a persistently enlarged appendiceal diameter at 6 months should increase the suspicion of potential recurrent acute appendicitis.
On follow-up ultrasound, intraluminal fluid or sludge was more frequently detected in children with increased as opposed to normal size appendiceal diameter (P < 0.001). The intraluminal fluid or sludge and the association between an increased appendiceal diameter and intraluminal fluid or sludge were also detected more frequently in children with recurrent acute appendicitis than in children without (P < 0.001, P = 0.008, respectively). Intraluminal material appears to explain the persistence of an increased appendiceal diameter in most cases and to be a useful additional tool for predicting recurrent acute appendicitis. Intraluminal fluid or sludge detected at the initial diagnosis of uncomplicated acute appendicitis also appears to be associated with recurrent acute appendicitis (P = 0.002). Furthermore, intraluminal fluid or sludge appears to predict recurrent acute appendicitis in multivariate analysis.
Moteki and Horikoshi [29] reported that intraluminal appendiceal fluid could be a new diagnostic criterion for acute appendicitis. Other authors [13, 28] concluded that intraluminal fluid can help predict recurrent acute appendicitis after successful nonoperative management of uncomplicated acute appendicitis in pediatric patients and our results support their findings. A possible explanation for persistent intraluminal content could be that the obstruction of the appendiceal lumen related to the initial episode of acute appendicitis resolves only partially in some children and it is likely these children have an increased risk for recurrent acute appendicitis.
No significant correlation was found between the appendiceal diameter at the initial diagnosis and the risk of recurrence. This agrees with results reported by some authors [13] but not with others [28].
Most children with recurrent acute appendicitis (23/29) were treated surgically and the diagnosis was confirmed histologically in all. None of the children with recurrent acute appendicitis presented with perforated appendicitis and all had an uncomplicated course, suggesting that initial nonoperative treatment is safe in the medium- to long-term, as reported in the literature [9]. The detection of an enlarged appendiceal diameter on follow-up ultrasound appears to be associated with surgical recurrent acute appendicitis, but this finding must be interpreted with caution, as the choice for the surgical approach was often influenced by the parents’ preference.
The results of this study influenced our practice. We introduced a protocol for ultrasound follow-up of children treated for uncomplicated acute appendicitis in our hospital, which includes ultrasound of the appendix every 3 months with the end points of either normalization of sonographic appearance or development of recurrent acute appendicitis. In cases with increased appendiceal diameter, intraluminal fluid or sludge, or the association of both these parameters, closer clinical follow-up is recommended, as we consider the risk of recurrent acute appendicitis to be increased.
The current study was limited by the relatively small number of patients. Among the 835 children treated conservatively for uncomplicated acute appendicitis in our hospital, 204 underwent 3-month follow-up ultrasound, 26 presented for 6-month follow-up and only 3 received 9-month follow-up. In addition, the sample size and selection were not standardized, as only a small subset of the children presented for follow-up ultrasound. Therefore, the population analyzed may not accurately reflect the entire population of children treated nonoperatively for uncomplicated acute appendicitis in our hospital. However, with the aim of decreasing this bias, we compared the children who presented for sonographic follow-up with the children who received only clinical follow-up and did not find any significant differences (Online Supplementary Material 2). Larger studies with more precisely defined follow-up criteria are needed to confirm our findings.
This was a single-center study conducted at a hospital with a radiology team able to perform follow-up ultrasound. It is possible that our results would not be applicable in a setting with different characteristics and different US availability.
Conclusion
By the end of the follow-up period, 29 (14.2%) children had developed recurrent acute appendicitis and 175 had recovered uneventfully. A trend toward progressive normalization of the appendiceal diameter over time was noted at follow-up ultrasounds. The prevalence of appendiceal diameter enlargement and intraluminal fluid or sludge were increased in children who later developed recurrent acute appendicitis. Ultrasound appears to be a useful tool for the follow-up of children with conservatively treated uncomplicated acute appendicitis and may help predict recurrence.
References
Rentea RM, St Peter SD (2017) Pediatric appendicitis. Surg Clin North Am 97:93–112
St Peter SD, Sharp SW, Holcomb GW et al (2008) An evidence-based definition for perforated appendicitis derived from a prospective randomized trial. J Pediatr Surg 43:2242–2245
Reynolds SL, Jaffe DM (1992) Diagnosing abdominal pain in a pediatric emergency department. Pediatr Emerg Care 8:126–128
Scholer SJ, Pituch K, Orr DP et al (1996) Clinical outcomes of children with acute abdominal pain. Pediatrics 98:680–685
Huang L, Yin Y, Yang L et al (2017) Comparison of antibiotic therapy and appendectomy for acute uncomplicated appendicitis in children: a meta-analysis. JAMA Pediatr 171:426–434
Tanaka Y, Uchida H, Kawashima H et al (2015) Long-term outcomes of operative versus nonoperative treatment for uncomplicated appendicitis. J Pediatr Surg 50:1893–1897
Georgiou R, Eaton S, Stanton MP et al (2017) Efficacy and safety of nonoperative treatment for acute appendicitis: a meta-analysis. Pediatrics 139:e20163003
Minneci PC, Mahida JB, Lodwick DL et al (2016) Effectiveness of patient choice in nonoperative vs surgical management of pediatric uncomplicated acute appendicitis. JAMA Surg 151:408–415
Maita S, Andersson B, Svensson JF et al (2020) Nonoperative treatment for nonperforated appendicitis in children: a systematic review and meta-analysis. Pediatr Surg Int 36:261–269
Gorter RR, The SML, Gorter-Stam MAW et al (2017) Systematic review of nonoperative versus operative treatment of uncomplicated appendicitis. J Pediatr Surg 52:1219–1227
Hartwich J, Luks FI, Watson-Smith D et al (2016) Nonoperative treatment of acute appendicitis in children: a feasibility study. J Pediatr Surg 51:111–116
Steiner Z, Buklan G, Stackievicz R et al (2015) A role for conservative antibiotic treatment in early appendicitis in children. J Pediatr Surg 50:1566–1568
Steiner Z, Buklan G, Stackievicz R et al (2017) Conservative treatment in uncomplicated acute appendicitis: reassessment of practice safety. Eur J Pediatr 176:521–527
Steiner Z, Buklan G, Gutermacher M et al (2018) Conservative antibiotic treatment for acute uncomplicated appendicitis is feasible. Pediatr Surg Int 34:283–288
Minneci PC, Hade EM, Lawrence A et al (2020) Association of nonoperative management using antibiotic therapy vs laparoscopic appendectomy with treatment success and disability days in children with uncomplicated appendicitis. JAMA 324:581–593
Hansson J, Körner U, Ludwigs K et al (2012) Antibiotics as first-line therapy for acute appendicitis: evidence for a change in clinical practice. World J Surg 36:2028–2036
Antakia R, Xanthis A, Georgiades F et al (2021) Acute appendicitis management during the COVID-19 pandemic: a prospective cohort study from a large UK center. Int J Surg 86:32–37
Mowbray NG, Hurt L, Powell-Chandler A et al (2021) Where have all the appendicectomies gone? Ann R Coll Surg Engl 103:250–254
Swenson DW, Ayyala RS, Sams C et al (2018) Practical imaging strategies for acute appendicitis in children. AJR Am J Roentgenol 211:901–909
Doria AS, Moineddin R, Kellenberger CJ et al (2006) US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology 241:83–94
Zhang H, Liao M, Chen J et al (2017) Ultrasound, computed tomography or magnetic resonance imaging - which is preferred for acute appendicitis in children? A meta-analysis. Pediatr Radiol 47:186–196
Cundy TP, Gent R, Frauenfelder C et al (2016) Benchmarking the value of ultrasound for acute appendicitis in children. J Pediatr Surg 51:1939–1943
Bachur RG, Callahan MJ, Monuteaux MC et al (2015) Integration of ultrasound findings and a clinical score in the diagnostic evaluation of pediatric appendicitis. J Pediatr 166:1134–1139
Eriksson S, Tisell A, Granström L (1995) Ultrasonographic findings after conservative treatment of acute appendicitis and open appendicectomy. Acta Radiol 36:173–177
Samuel M (2002) Pediatric appendicitis score. J Pediatr Surg 37:877–881
Patkova B, Svenningsson A, Almström M et al (2020) Nonoperative treatment versus appendectomy for acute nonperforated appendicitis in children: five-year follow up of a randomized controlled pilot trial. Ann Surg 271:1030–1035
Tsai HM, Shan YS, Lin PW et al (2006) Clinical analysis of the predictive factors for recurrent appendicitis after initial nonoperative treatment of perforated appendicitis. Am J Surg 192:311–316
Koike Y, Uchida K, Matsushita K et al (2014) Intraluminal appendiceal fluid is a predictive factor for recurrent appendicitis after initial successful non-operative management of uncomplicated appendicitis in pediatric patients. J Pediatr Surg 49:1116–1121
Moteki T, Horikoshi H (2007) New CT criterion for acute appendicitis: maximum depth of intraluminal appendiceal fluid. AJR Am J Roentgenol 188:1313–1319
Acknowledgements
We thank Faye Schreiber for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stackievicz, R., Milner, R., Werner, M. et al. Follow-up ultrasonographic findings among children treated conservatively for uncomplicated acute appendicitis. Pediatr Radiol 53, 223–234 (2023). https://doi.org/10.1007/s00247-022-05497-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-022-05497-2