Abstract
Background
The diagnosis of myocarditis presenting as isolated acute chest pain with elevated troponins but normal systolic function is challenging with significant drawbacks even for the gold-standard endomyocardial biopsy.
Objective
This study aimed to evaluate the diagnostic role of strain imaging by echocardiography and cardiac MRI in these patients.
Materials and methods
This was a retrospective review of children with cardiac MRI for acute chest pain with elevated troponins compared to normal controls. Echocardiographic fractional shortening, ejection fraction, speckle-tracking-derived peak longitudinal, radial, and circumferential strain were compared to cardiac MRI ejection fraction, T2 imaging, late gadolinium enhancement, speckle-tracking-derived peak longitudinal strain, radial strain, and circumferential strain.
Results
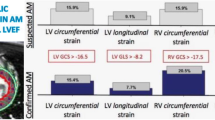
Group 1 included 10 subjects diagnosed with myocarditis, 9 (90%) males with a median age of 15.5 years (range: 14-17 years) compared with 10 age-matched controls in group 2. All subjects in group 1 had late gadolinium enhancement consistent with myocarditis and troponin ranged from 2.5 to >30 ng/ml. Electrocardiogram changes included ST segment elevation in 6 and abnormal Q waves in 1. Qualitative echocardiographic function was normal in both groups and mean fractional shortening was similar (35±6% in group 1 vs. 34±4% in group 2, P=0.70). Left ventricle ejection fraction by cardiac MRI, however, was lower in group 1 (52±9%) compared to group 2 at (59±4%) (P=0.03). Cardiac MRI derived strain was lower in group 1 vs. group 2 for speckle-tracking-derived peak longitudinal strain (-12.8±2.8% vs. -17.1±1.5%, P=0.001), circumferential strain (-12.3±3.8% vs. -15.8±1.2%, P=0.020) and radial strain (13.6±3.7% vs. 17.2±3.2%, P=0.040). Echocardiography derived strain was also lower in group 1 vs. group 2 for speckle-tracking-derived peak longitudinal strain (-15.6±3.9% vs. -20.8±2.2%, P<0.002), circumferential strain (-16±3% vs. -19.8±1.9%, P<0.003) and radial strain (17.3±6.1% vs. 24.8±6.3%, P=0.010).
Conclusion
In previously asymptomatic children, myocarditis can present with symptoms of acute chest pain suspicious for coronary ischemia. Cardiac MRI and echocardiographic strain imaging are noninvasive, radiation-free tests of immense diagnostic utility in these situations. Long-term studies are needed to assess prognostic significance of these findings.



Similar content being viewed by others
References
Selbst SM, Ruddy RM, Clark BJ et al (1988) Pediatric chest pain: a prospective study. Pediatrics 82:319–323
Ohman EM, Armstrong PW, Christenson RH et al (1996) Cardiac troponin T levels for risk stratification in acute myocardial ischemia. GUSTO IIA Investigators. N Engl J Med 335:1333–1341
Mir A, Obafemi A, Young A, Kane C (2011) Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics 128:e1622–e1627
Friedman KG, Kane DA, Rathod RH et al (2011) Management of pediatric chest pain using a standardized assessment and management plan. Pediatrics 128:239–245
Brown JL, Hirsh DA, Mahle WT (2012) Use of troponin as a screen for chest pain in the pediatric emergency department. Pediatr Cardiol 33:337–342
Eisenberg MA, Green-Hopkins I, Alexander ME, Chiang VW (2012) Cardiac troponin T as a screening test for myocarditis in children. Pediatr Emerg Care 28:1173–1178
Bachmaier K, Mair J, Offner F et al (1995) Serum cardiac troponin T and creatine kinase-MB elevations in murine autoimmune myocarditis. Circulation 92:1927–1932
Hirsch R, Landt Y, Porter S et al (1997) Cardiac troponin I in pediatrics: normal values and potential use in the assessment of cardiac injury. J Pediatr 130:872–877
Zhang T, Miao W, Wang S et al (2015) Acute myocarditis mimicking ST-elevation myocardial infarction: A case report and review of the literature. Exp Ther Med 10:459–464
Brighenti M, Donti A, Giulia Gagliardi M et al (2015) Endomyocardial biopsy safety and clinical yield in pediatric myocarditis: An Italian perspective. Catheter Cardiovasc Interv 87:762–767
Zhorne D, Petit CJ, Ing FF et al (2013) A 25-year experience of endomyocardial biopsy safety in infants. Catheter Cardiovasc Interv 82:797–801
Kühl U, Schultheiss HP (2010) Myocarditis in children. Heart Fail Clin 6:483–496
Schumm J, Greulich S, Wagner A et al (2014) Cardiovascular magnetic resonance risk stratification in patients with clinically suspected myocarditis. J Cardiovasc Magn Reson 16:14
Yilmaz A, Ferreira V, Klingel K et al (2013) Role of cardiovascular magnetic resonance imaging (CMR) in the diagnosis of acute and chronic myocarditis. Heart Fail Rev 18:747–760
Caforio AL, Pankuweit S, Arbustini E et al (2013) Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 34:2636–2648, 2648a-2648d
Skouri HN, Dec GW, Friedrich MG, Cooper LT (2006) Noninvasive imaging in myocarditis. J Am Coll Cardiol 48:2085–2093
Childs H, Friedrich MG (2011) Cardiovascular magnetic resonance imaging in myocarditis. Prog Cardiovasc Dis 54:266–275
Etesami M, Gilkeson RC, Rajiah P (2015) Utility of late gadolinium enhancement in pediatric cardiac MRI. Pediatr Radiol 46:1096–1113
Vermes E, Childs H, Faris P, Friedrich MG (2014) Predictive value of CMR criteria for LV functional improvement in patients with acute myocarditis. Eur Heart J Cardiovasc Imaging 15:1140–1144
Løgstrup BB, Nielsen JM, Kim WY, Poulsen SH (2015) Myocardial oedema in acute myocarditis detected by echocardiographic 2D myocardial deformation analysis. Eur Heart J Cardiovasc Imaging 17:1018–1026
Uppu SC, Shah A, Weigand J et al (2015) Two-dimensional speckle-tracking-derived segmental peak systolic longitudinal strain identifies regional myocardial involvement in patients with myocarditis and normal global left ventricular systolic function. Pediatr Cardiol 36:950–959
Weigand J, Nielsen JC, Sengupta PP et al (2016) Feature tracking-derived peak systolic strain compared to late gadolinium enhancement in troponin-positive myocarditis: a case-control study. Pediatr Cardiol 37:696–703
Banka P, Robinson JD, Uppu SC et al (2016) Cardiovascular magnetic resonance techniques and findings in children with myocarditis: a multicenter retrospective study. J Cardiovasc Magn Reson 17:96
André F, Stock FT, Riffel J et al (2016) Incremental value of cardiac deformation analysis in acute myocarditis: a cardiovascular magnetic resonance imaging study. Int J Card Imaging 32:1093–1101
Lopez L, Colan SD, Frommelt PC et al (2010) Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr 23:465–495
Buddhe S, Lewin M, Olson A et al (2016) Comparison of left ventricular function assessment between echocardiography and MRI in Duchenne muscular dystrophy. Pediatr Radiol 46:1399–1408
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Luetkens JA, Homsi R, Sprinkart AM et al (2016) Incremental value of quantitative CMR including parametric mapping for the diagnosis of acute myocarditis. Eur Heart J Cardiovasc Imaging 17:154–161
Cheng S, Larson MG, McCabe EL et al (2013) Reproducibility of speckle-tracking-based strain measures of left ventricular function in a community-based study. J Am Soc Echocardiogr 26:1258–1266.e1252
Di Bella G, Gaeta M, Pingitore A et al (2010) Myocardial deformation in acute myocarditis with normal left ventricular wall motion--a cardiac magnetic resonance and 2-dimensional strain echocardiographic study. Circ J 74:1205–1213
Scatteia A, Baritussio A, Bucciarelli-Ducci C (2017) Strain imaging using cardiac magnetic resonance. Heart Fail Rev 22:465–476
Mavrogeni S, Markousis-Mavrogenis G, Kolovou G (2016) How to approach the great mimic? Improving techniques for the diagnosis of myocarditis. Expert Rev Cardiovasc Ther 14:105–115
Baeßler B, Schaarschmidt F, Dick A et al (2016) Diagnostic implications of magnetic resonance feature tracking derived myocardial strain parameters in acute myocarditis. Eur J Radiol 85:218–227
Kobayashi D, Aggarwal S, Kheiwa A, Shah N (2012) Myopericarditis in children: elevated troponin I level does not predict outcome. Pediatr Cardiol 33:1040–1045
Lee PT, See CK, Chiam PT, Lim ST (2015) Electrocardiographic changes in acute perimyocarditis. Singap Med J 56:e1–e3
Koopman LP, Slorach C, Manlhiot C et al (2011) Assessment of myocardial deformation in children using Digital Imaging and Communications in Medicine (DICOM) data and vendor independent speckle tracking software. J Am Soc Echocardiogr 24:37–44
Wisotzkey BL, Soriano B, Albers E et al (2016) Myocarditis masquerading as acute coronary syndrome: diagnostic role of cardiac MRI. J Cardiovasc Magn Reson 18:174
Acknowledgements
This abstract was presented at the Society for Cardiovascular Magnetic Resonance meeting January 27-30, 2016 in Los Angeles, California [37].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Wisotzkey, B.L., Soriano, B.D., Albers, E.L. et al. Diagnostic role of strain imaging in atypical myocarditis by echocardiography and cardiac MRI. Pediatr Radiol 48, 835–842 (2018). https://doi.org/10.1007/s00247-017-4061-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-4061-0