Abstract
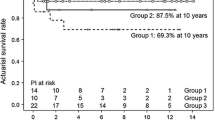
For neonates with right atrial isomerism (RAI), functional single ventricle (f-SV), and obstructive total anomalous pulmonary venous connection (TAPVC), primary TAPVC repair (TAPVCR) has a poor outcome. At our hospital, the survival rate at 1 year of such neonates undergoing primary TAPVCR between 1999 and 2010 (TAPVCR group) was 30% (3/10). Most deceased cases suffered from capillary leak syndrome and unstable pulmonary resistance after the surgeries. We sought to determine whether less invasive primary draining vein stenting (DVS) improved the outcome of these neonates. We investigated outcomes in consecutive nine such neonates (median gestational age 38 weeks, birth weight 2.8 kg, females 4) who underwent primary DVS with 6-mm-diameter Palmaz® Genesis® stents at our hospital between 2007 and 2017 (DVS group). Eight patients underwent subsequent surgeries to adjust the pulmonary flow after decreased pulmonary resistance. The survival rate at 1 year after the first interventions in the DVS group improved to 77% (7/9), although there was a difference between the interventional eras of the two groups. Of the seven patients who underwent multiple stent redilations with a larger balloon or additional stenting in other sites until the next stage of surgery at a median age of 8 months, four received a bidirectional Glenn (BDG) shunt and TAPVCR and three underwent TAPVCR, with two of those cases reaching BDG. Less invasive primary DVS improved the outcome of neonates with RAI, f-SV, and obstructive TAPVC, with many reaching BDG. Patient selection to advance toward Fontan is thought to further improve the outcome.



Similar content being viewed by others
Change history
19 June 2019
The authors have retracted this article [1] because, contrary to the statement in the article, this research did not obtain ethics approval from the National Cerebral and Cardiovascular Center Institutional Review Board prior to submission of the manuscript to Pediatric Cardiology. All authors agree to this retraction.
19 June 2019
The authors have retracted this article [1] because, contrary to the statement in the article, this research did not obtain ethics approval from the National Cerebral and Cardiovascular Center Institutional Review Board prior to submission of the manuscript to Pediatric Cardiology. All authors agree to this retraction.
19 June 2019
The authors have retracted this article [1] because, contrary to the statement in the article, this research did not obtain ethics approval from the National Cerebral and Cardiovascular Center Institutional Review Board prior to submission of the manuscript to Pediatric Cardiology. All authors agree to this retraction.
References
Anagnostopoulos PV, Pearl JM, Octave C, Cohen M, Gruessner A, Wintering E, Teodori MF (2009) Improved current era outcomes in patients with heterotaxy syndromes. Eur J Cardiothorac Surg 35:871–877
Ota N, Fujimoto Y, Murata M, Tosaka Y, Ide Y, Tachi M, Ito H, Sugimoto A, Sakamoto K (2012) Improving outcomes of the surgical management of right atrial isomerism. Ann Thorac Surg 93:832–838
Serraf A, Bensari N, Houyel L, Capderou A, Roussin R, Lebret E, Ly M, Belli E (2010) Surgical management of congenital heart defects associated with heterotaxy syndrome. Eur J Cardiothorac Surg 38:721–727
Khan MS, Bryant R 3rd, Kim SH, Hill KD, Jacobs JP, Jacobs ML, Pasquali SK, Morales DL (2015) Contemporary outcomes of surgical repair of total anomalous pulmonary venous connection in patients with heterotaxy syndrome. Ann Thorac Surg 99:2134–2139
Yun TJ, Al-Radi OO, Adatia I, Caldarone CA, Coles JG, Williams WG, Smallhorn J, Van Arsdell GS (2006) Contemporary management of right atrial isomerism: effect of evolving therapeutic strategies. J Thorac Cardiovasc Surg 131:1108–1113
Hoashi T, Kagisaki K, Oda T, Kitano M, Kurosaki K, Shiraishi I, Yagihara T, Ichikawa H (2013) Long-term results of treatments for functional single ventricle associated with extracardiac type total anomalous pulmonary venous connection. Eur J Cardiothorac Surg 43:965–970
Cheung YF, Cheng VY, Chau AK, Chiu CS, Yung TC, Leung MP (2002) Outcome of infants with right atrial isomerism: is prognosis better with normal pulmonary venous drainage? Heart 87:146–152
Foerster SR, Gauvreau K, McElhinney DB, Geva T (2008) Importance of totally anomalous pulmonary venous connection and postoperative pulmonary vein stenosis in outcomes of heterotaxy syndrome. Pediatr Cardiol 29:536–544
St Louis JD, McCracken CE, Turk EM, Hancock HS, Menk JS, Harvey BA, Vinocur JM, Oster ME, Moller JH, Spector LG, Kochilas LK (2018) Long-term transplant-free survival after repair of total anomalous pulmonary venous connection. Ann Thorac Surg 105:186–192
Lodge AJ, Rychik J, Nicolson SC, Ittenbach RF, Spray TL, Gaynor JW (2004) Improving outcomes in functional single ventricle and total anomalous pulmonary venous connection. Ann Thorac Surg 78:1688–1695
Morales DL, Braud BE, Booth JH, Graves DE, Heinle JS, McKenzie ED, Fraser CD Jr (2006) Heterotaxy patients with total anomalous pulmonary venous return: improving surgical results. Ann Thorac Surg 82:1621–1627
Jacobs JP, Pasquali SK, Morales DL, Jacobs ML, Mavroudis C, Chai PJ, Tchervenkov CI, Lacour-Gayet FG, Walters H 3rd, Quintessenza JA (2011) Heterotaxy: lessons learned about patterns of practice and outcomes from the congenital heart surgery database of the society of thoracic surgeons. World J Pediatr Congenit Heart Surg 2:278–286
Nakata T, Fujimoto Y, Hirose K, Osaki M, Tosaka Y, Ide Y, Tachi M, Sakamoto K (2009) Functional single ventricle with extracardiac total anomalous pulmonary venous connection. Eur J Cardiothorac Surg 36:49–56
Kitano M, Yazaki S, Kagisaki K, Kurosaki K (2009) Primary palliative stenting against obstructive mixed-type total anomalous pulmonary venous connection associated with right atrial isomerism. J Interv Cardiol 22:404–409
Wong DT, Yoo SJ, Lee KJ (2008) Implantation of drug-eluting stents for relief of obstructed infra-cardiac totally anomalous pulmonary venous connection in isomerism of the right atrial appendages. Cardiol Young 18:628–630
Jhang WK, Chang YJ, Park CS, Oh YM, Kim YH, Yun TJ (2008) Hybrid palliation for right atrial isomerism associated with obstructive total anomalous pulmonary venous drainage. Interact Cardiovasc Thorac Surg 7:282–284
Kobayashi D, Forbes TJ, Aggarwal S (2013) Palliative stent placement in vertical vein in a 1.4 kg infant with obstructed supracardiac total anomalous pulmonary venous connection. Catheter Cardiovasc Interv 82:574–580
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
The ethical standards of the institutional research committee granted permission to access and analyze the data with a waiver of informed consent because this is a retrospective analysis of the collected data.
Additional information
The authors have retracted this article because, contrary to the statement in the article, this research did not obtain ethics approval from the National Cerebral and Cardiovascular Center Institutional Review Board prior to submission of the manuscript to Pediatric Cardiology. All authors agree to this retraction.
About this article
Cite this article
Kitano, M., Hoashi, T., Kakuta, T. et al. RETRACTED ARTICLE: Primary Draining Vein Stenting for Obstructive Total Anomalous Pulmonary Venous Connection in Neonates with Right Atrial Isomerism and Functional Single Ventricle Improves Outcome. Pediatr Cardiol 39, 1355–1365 (2018). https://doi.org/10.1007/s00246-018-1902-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-018-1902-z