Abstract
Purpose
To quantitate gadolinium deposits in gliomas and adjacent normal brain specimens, and to evaluate their association with tumor contrast enhancement and the type of gadolinium-based contrast agent (GBCA) used.
Methods
A total of 69 patients with primary glioma who underwent contrast-enhanced magnetic resonance imaging (MRI) prior to surgery were included in this retrospective study. Gadolinium was measured from histologically viable tumor, normal brain, and necrosis within the sample, when available, using inductively coupled plasma mass spectrometry (ICP-MS). Tumor contrast enhancement was categorized as none, minimal, or noticeable. Differences in gadolinium deposits by contrast enhancement and GBCA type were assessed.
Results
Seven patients received linear GBCA and 62 macrocyclic, respectively. At the time of surgery, gadolinium deposits were detected in 39 out of 69 (57%) tumor samples, 8 out of 13 (62%) normal brain, and 12 out of 14 (86%) necrotic specimens. Gadolinium was detected in both enhancing and non-enhancing tumors, but was greatest in gliomas with noticeable enhancement (p = 0.02). Administration of linear agents gadodiamide and gadopentetate dimeglumine resulted in significantly higher tumor gadolinium relative to macrocyclic gadoterate meglumine (p < 0.01 and p < 0.05, respectively). Normal brain and necrosis also showed higher gadolinium after exposure to linear gadodiamide (both p < 0.05). In multivariate regression, GBCA type (linear/macrocyclic) was the most powerful predictor of tumor gadolinium retention (p < 0.001).
Conclusion
Gadolinium can be detected in both enhancing and non-enhancing gliomas, neighboring normal brain, and necrosis. Gadolinium retention is higher after exposure to linear GBCAs compared with the macrocyclic gadoterate meglumine.
Similar content being viewed by others
Introduction
Gadolinium is a heavy metal employed by the standard contrast agents used for MRI due to its paramagnetic nature. Free gadolinium ion (Gd3+), however, is highly toxic. To decrease its toxicity and increase elimination from the body, Gd3+ is bound to organic chelating agents. Chelators used in gadolinium-based contrast agents (GBCAs) can be classified as either linear or macrocyclic, of which the latter are superior in stability (especially the kinetic stability) [1]. In contrast, linear GBCAs have shown in vitro to release substantial amounts of free Gd3+ and are regarded as more unstable [2].
Deposition of gadolinium in the liver, kidney, and bone of mice and rats after exposure to linear GBCAs was reported already in the 1990s [3]. Nevertheless, both linear and macrocyclic GBCAs have been used in routine clinical practice for almost 30 years with no other serious adverse effects described than nephrogenic systemic fibrosis in patients with severe renal insufficiency [4].
In 2014, however, Kanda et al. demonstrated increased signal intensities in the dentate nucleus (DN) and globus pallidus (GP), attributed to deposition of gadolinium, on the T1-weighted (T1W) brain MR images of patients who had received multiple doses of linear GBCA and with normal renal function [5]. This association was supported by several other investigators [6,7,8], whereas administration of macrocyclic GBCAs, even at high doses, was not found to be related to increased signal intensity [9,10,11]. Finally, gadolinium deposition in the human brain after exposure to both linear and macrocyclic GBCAs was confirmed in autopsy specimens raising concern about the toxicity of the potential free gadolinium in the brain [12,13,14].
Several pathological conditions of the brain parenchyma such as tumor, infection, autoimmune disease, and ischemia may alter the integrity of the blood–brain barrier (BBB) resulting in contrast enhancement. Whereas gadolinium accumulation is predictable in diseased brain with disrupted BBB and contrast enhancement, gadolinium retention in brain abnormalities without evident BBB disruption or in adjacent normal brain has not previously been studied. Furthermore, despite the routine use of contrast MRI in brain tumor diagnostics, only one previous study has attempted to quantify gadolinium retention in brain tumors. Xia et al. visually detected gadolinium deposits in five out of 28 tumor samples using scanning electron microscopy/energy-dispersive X-ray spectroscopy (SEM/EDS) [15]. However, only linear GBCAs were used in this study and tumor contrast enhancement was not reported.
The purpose of this study was to quantitate gadolinium accumulation in viable tumor tissue and the neighboring normal-appearing brain in both enhancing and non-enhancing gliomas. Also, the aim was to study the association of gadolinium retention with the type and number of GBCA doses administered, tumor subtype, contrast enhancement, and patient renal function.
Materials and methods
This study was approved by the Ethics Committee of Auria Biobank (TYKS-SAPA, Turku University Hospital, Turku, Finland) and the Hospital District of Southwest Finland. All tissue samples were obtained from Auria Biobank, and in accordance with the Finnish Biobank Act (688/2012), a separate informed consent from individual patients was waived.
Patient selection
Adult patients with newly diagnosed supratentorial glioma (brainstem gliomas excluded) surgically resected or biopsied at Turku University Hospital from January 2005 through December 2013 were retrospectively included. A total of 184 glioma patients were identified out of which 115 were excluded due to insufficient tissue material and/or unavailable pre-operative MR scan. Finally, 69 patients were included. Clinical data was collected from electronic patient records. Plasma creatinine level obtained nearest to the MR scan was used, and glomerular filtration rate (GFR) was calculated using the CKD-EPI equation with creatinine, age, gender, and race taken into consideration.
GBCA administration and tumor contrast enhancement on T1W MRI
Pre-operative MR scans were performed in Turku University Hospital, affiliated hospitals, or private clinics, in case of which all related scans were transferred to University Hospital PACS. Information on the GBCA used was retrieved from the Radiology Information System at University Hospital, PACS, or personal communication with the chief radiologists in affiliated hospitals and private clinics. Only GBCA exposures with evidence of the tumor on brain MRI were included in analyses.
Pre-operative MR images were analyzed by a radiologist with 7 years of experience (A.K.). Tumor contrast enhancement on T1WI was visually categorized into three separate groups: (1) no evidence of contrast enhancement, (2) minimal contrast enhancement defined as one or two small foci of enhancement while the gross majority of the solid tumor was non-enhancing, and (3) distinct/noticeable contrast enhancement.
Tissue samples
Formalin-fixed paraffin-embedded glioma samples were used to determine gadolinium concentration in three distinctive areas: (1) histologically viable tumor, (2) normal-appearing brain tissue when present in the sample, and (3) necrosis. A neuropathologist (M.G.) made annotations with a diameter of 1.5 mm to the most representative areas in the scanned hematoxylin and eosin slides using Pannoramic Viewer software (3DHistech, Budapest, Hungary). Corresponding tissue cores from paraffin-embedded samples were then automatically obtained using a dedicated automatic microarrayer (TMA Grand Master, 3DHistech, Budapest, Hungary). Depending on the sample thickness, one to four cores per area were used for analyses. Tissue cores were deparaffinized with xylene and washed in serial dilutions of ethanol which was finally vaporized at room temperature. Deparaffinized tissue samples were weighted and used for gadolinium measurements using ICP-MS.
Gadolinium measurements using ICP-MS
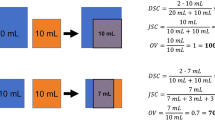
First, 57 samples (42 tumor, 8 normal brain, 7 necrosis) were microwave digested in a mixture of 2.5 ml nitric acid and 0.5 ml hydrogen peroxide and a Teflon vessel was washed out with 50 ml deionized water resulting in relatively low concentrations (average weight of tumor samples 3.3 mg). Therefore, the remaining 40 samples (27 tumor, 6 normal brain, 7 necrosis) were digested by heating the mixture of tissue, 0.5 ml nitric acid, and 0.1 ml hydrogen peroxide up to 100 °C in a glass bottle and washed out with 5 ml deionized water.
Samples were analyzed by ICP-MS (PerkinElmer Sciex Elan 6100 DRC Plus, Waltham, MA, USA) using the following parameters: sweeps/reading = 10, readings/replicate = 1, number of replicates = 7, scan mode = peak hopping, MCA channels = 1, dwell time = 100.0 ms, and integration time = 1000 ms. In addition to gadolinium (mass = 157.924), also rhodium (mass = 102.905) was analyzed and used as an internal standard. Multi-standard 101 was used as a calibration standard for gadolinium (conc. 1, 2.5, 5.0, 10, 25, 50 ppb). The limit of detection was set at 33% relative standard deviation (RSD) to reckon the low gadolinium concentration in the first set of analyses [16]. Measurements with an RSD above 33% were regarded as gadolinium concentration of zero.
The radiologist, neuropathologist, and laboratory personnel were all blinded to the type of GBCA administered at the time of MRI evaluation, tissue analysis, and ICP-MS measurements, respectively.
Glioma classification
The molecular profile of the glioma samples including IDH1 and IDH2 mutation (immunohistochemistry and DNA sequencing), 1p19q codeletion (fluorescent in situ hybridization), and ATRX and p53 mutation (immunohistochemistry) were analyzed, and with all the molecular data available, gliomas were re-assessed by a neuropathologist (M.G.) and diagnosed according to the new WHO 2016 classification.
Statistics
Gadolinium concentration is reported as medians, minimum–maximum range, 25th percentile (P25th), and 75th percentile (P75th) due to the non-normal distribution of the data. Differences on gadolinium concentration by diagnosis, tumor contrast enhancement, and number of GBCA doses administered were assessed with Kruskal–Wallis test. The Mann–Whitney U test was used for pairwise comparisons using the Bonferroni correction when appropriate. Correlations between gadolinium in the tumor and MRI–operation interval, GFR, and gadolinium in normal brain and necrosis were assessed by using the Spearman rank correlation coefficient. A linear multivariate regression analysis was performed to evaluate the significance of contrast enhancement, GBCA type, and GBCA–operation interval to predict gadolinium content. Two-tailed p values < 0.05 were regarded as significant. All statistical analyses were conducted using the IBM SPSS Statistics version 23.0 for Mac (IBM Corp., Armonk, NY, USA).
Results
Baseline patient, tumor, and MRI characteristics
Primary glioma samples from 69 patients were included (28 glioblastomas, 27 diffuse astrocytomas, and 14 oligodendrogliomas; Table 1). Viable tumor tissue was obtained from all 69 samples, normal brain from 14 samples, and necrosis from 14 glioblastomas. One normal brain sample was excluded since the patient had received three doses of gadopentetate dimeglumine 11 years earlier (without evidence of brain tumor on MRI). This may affect gadolinium deposition in the normal brain and would influence the analyses since at the time of glioma diagnosis the patient received gadoterate meglumine only. Finally, 13 normal brain samples were analyzed.
All glioblastomas showed distinct contrast enhancement whereas in diffuse gliomas the enhancement was more variable. Gadoterate meglumine (Dotarem, Guerbet, Villepinte, France) was used in 60 patients, gadobutrol (Gadovist, Bayer, Whippany, NJ, USA) in two, gadodiamide (Omniscan, GE Healthcare, Chicago, IL, USA) in four, and gadopentetate dimeglumine (Magnevist, Bayer, Whippany, NJ, USA) in three patients, respectively. Linear GBCAs were administered during 2006–2009 and macrocyclic agents 2005–2013. Sixty patients received only one GBCA dose, and nine patients received two to three doses (exclusively gadoterate meglumine) prior to surgery and with evidence of the tumor occurring in the brain MRI. The mean interval between the last GBCA administration and operation was 24 days (range 1–104 days). None of the patients suffered from renal failure.
Gadolinium is detected both in enhancing and non-enhancing gliomas
Gadolinium was detected in 39 out of 69 (57%) tumor samples. Gadolinium retention was most common in glioblastomas, however, without significant difference among diagnoses. In contrast, gadolinium retention associated with contrast enhancement (chi-square p = 0.04, Table 2). Gadolinium was significantly higher in gliomas with noticeable contrast enhancement compared to non-enhancing gliomas (p = 0.02, Fig. 1). However, it should be noted that 7 out of 21 (33%) patients with non-enhancing gliomas showed detectable gadolinium (Fig. 2). Among these, six had received gadoterate meglumine and one gadobutrol, respectively. The routinely used dosage of GBCAs was 0.2 ml/kg. For four patients with one GBCA MRI, the dosage was 0.1 ml/kg. No difference in gadolinium retention was detected with regard to the dose (p = 0.62), GFR value (p = 0.17), or number of GBCA doses administered (p = 0.34; gadoterate meglumine was exclusively used in patients receiving multiple GBCA doses).
Levels of tumor gadolinium by contrast enhancement (CE) on T1W MRI. Gadolinium concentration is significantly higher in noticeably enhancing gliomas compared to non-enhancing gliomas (*p = 0.02). Three outliers are distinguished with their gadolinium concentration. Data points are shown with medians and interquartile ranges
Representative images of contrast-enhanced T1W MRI and corresponding H&E stainings (×200 magnification). a Astrocytoma, IDH-mutant grade II with no contrast enhancement on MRI and b no signs of endothelial proliferation in tumor vessels (black arrow). c Oligodendroglioma, IDH-mutant, and 1p19q-codeleted grade II with a minor focus of enhancement (white arrow) but d H&E showing thin-walled tumor vessels and no signs of endothelial proliferation. (e) Glioblastoma IDH-wild type with noticeable contrast enhancement and (f) tumor vasculature showing endothelial proliferation with multiple layers of endothelial cells and glomeruloid structures within tumor vessels (black arrow). Gadolinium was detected in each of these tumors
Gadolinium retention in gliomas is related to linear GBCAs
As presented in Fig. 3, significantly higher gadolinium concentrations were detected in tumors after administration of linear gadodiamide (median 627 μg/kg, range 319–2624 μg/kg, P25th 322 μg/kg, P75th 2199 μg/kg, n = 4; p = 0.002) and linear gadopentetate dimeglumine (median 349 μg/kg, range 164–3549 μg/kg, n = 3, p = 0.03) when compared with the macrocyclic gadoterate meglumine (median 4.5 μg/kg, range 0–1648 μg/kg, P25th 0 μg/kg, P75th 82 μg/kg, n = 60). No difference in tumor gadolinium was measured between the two linear agents or gadobutrol (range 34–627 μg/kg, n = 2) and other GBCAs. A negative correlation was found between tumor gadolinium concentration and the time interval between MRI and operation (Spearman’s rho = − 0.28, p = 0.02).
For the purpose of linear multivariate regression, GBCA type was analyzed as macrocyclic (gadoterate meglumine and gadobutrol) or linear (gadodiamide and gadopentetate dimeglumine). Linear regression was calculated to predict tumor gadolinium concentration (dependent variable) based on age, sex, tumor contrast enhancement, GBCA type, and MRI–operation interval (independent variables). Thirty one percent of the tumor gadolinium variance could be explained by the predictors (R2 = 0.312). GBCA type (macrocyclic versus linear) was the only significant predictor of tumor gadolinium concentration, which was 1042 μg/kg higher with linear compared with macrocyclic agents (p < 0.001, unstandardized coefficient 1042 μg/kg, 95% CI 628–1457 μg/kg).
Gadolinium retention in normal brain and necrosis is higher after exposure to linear gadodiamide
Gadolinium was detected in 8 out of 13 (62%) samples of histologically normal appearing brain (Table 2) with a significant correlation between gadolinium concentrations in the tumor and normal brain (Spearman’s rho = 0.65; p = 0.016; n = 13). Of these eight patients with gadolinium detected in the normal brain, two had received linear gadodiamide and six macrocyclic gadoterate meglumine, respectively. As shown in Fig. 4, gadolinium concentration in normal brain was significantly higher after exposure to linear gadodiamide (range 361–447 μg/kg, n = 2) compared with macrocyclic gadoterate meglumine (median 13 μg/kg, range 0–403 μg/kg, P25th 0 μg/kg, P75th 32 μg/kg; n = 11; p = 0.04).
Gadolinium retention was also detected in 12 out of 14 (86%) necrotic tissue samples (Table 2) with a significant correlation between gadolinium concentration in the tumor and necrosis (Spearman’s rho = 0.66; p = 0.01; n = 14). Necrosis gadolinium was significantly higher after exposure to linear gadodiamide (median 2852 μg/kg, range 639–15,012 μg/kg, n = 3) compared with macrocyclic gadoterate meglumine (median 118 μg/kg, range 0–1518 μg/kg, P25th 16 μg/kg, P75th 348 μg/kg; n = 9) as presented in Fig. 5 (p = 0.04). No difference in necrosis gadolinium was measured between gadoterate meglumine and gadopentetate dimeglumine (range 1734–1847 μg/kg, n = 2), or the two linear agents.
No significant difference in gadolinium concentrations were detected between tumor and normal brain, or tumor and necrosis, when comparing the concentrations within patients that had either normal brain (n = 13) or necrotic tissue samples (n = 14) available, respectively. Three patients had all three tissue specimens available. No significant difference, however, was detected in gadolinium concentrations between tumor, normal brain, and necrosis within the three patients.
Discussion
Gadolinium deposited in both enhancing and non-enhancing gliomas with the highest concentrations detected among tumors with gross enhancement on T1W MRI. Gadolinium was not only found in the viable tumor tissue but also in the normal-appearing adjacent brain and necrotic tissue, with a positive correlation between the amounts deposited in the tumor and normal brain or necrosis. Gadolinium retention was significantly higher after administering linear GBCAs compared with macrocyclic gadoterate meglumine. In multivariate regression analysis, GBCA type (macrocyclic versus linear) was the only significant predictor of tumor gadolinium concentration.
To date, five postmortem studies have demonstrated the pathologic accumulation of gadolinium in the human brain after exposure to linear [12, 13, 17, 18] or macrocyclic [14, 18] GBCAs. None of the studies, however, included decedents who had received gadoterate meglumine that was the most common GBCA used in our cohort of glioma patients. While the highest gadolinium concentrations were detected in DN and GP, two of these studies additionally showed small but measurable concentrations in the brain cortex and white matter suggesting more widespread low-level gadolinium retention in brain parenchyma than just the posterior fossa and basal ganglia [13, 14]. Our results are in line with this and further support the notion of gadolinium retention in small quantities in brain parenchyma of other regions than DN and GP after administration of both linear and macrocyclic agents.
Autopsy studies have shown that gadolinium deposition in the posterior fossa and basal ganglia is not limited to patients with intracranial abnormalities but can also be detected in patients with normal brains at the time of autopsy [17, 18]. Several mechanisms of this gadolinium transit and retention in brain regions without impaired BBB have been suggested including active metal transporters [19, 20], passage from the cerebrospinal fluid [21,22,23], and brain glymphatic system [24]. The exact mechanism behind the retention, however, remains unsolved. While the brain tumor provides an obvious explanation for gadolinium retention, we additionally found gadolinium deposits in the adjacent normal brain. Furthermore, a small but significant correlation between the amount of gadolinium in the tumor and normal brain was detected implying passage of gadolinium from the site of pathologic brain lesion. While further studies are needed to confirm this association, an interesting question arises whether gadolinium traverses from the region of brain lesion to neighboring sites in other brain abnormalities such as ischemia, infection, or multiple sclerosis.
Gadolinium concentration was significantly higher in both the tumor tissue and normal brain, as well as in necrosis, after exposure to linear GBCAs compared with the macrocyclic agent gadoterate meglumine. Our results emphasize the higher stability of macrocyclic agents and correspond to animal models showing higher gadolinium retention in brain tissue after exposure to linear relative to macrocyclic GBCAs [25, 26]. In humans, several studies have demonstrated increased T1W MRI signal intensities in the DN and GP after serial application of linear GBCAs [5, 6, 8, 10] but not after the use of macrocyclic agents [9, 10, 27].
We detected gadolinium deposits in 33% of gliomas that showed no evident contrast enhancement on T1W MR images. Whereas contrast enhancement indicates disrupted and leaky BBB and provides an obvious explanation for gadolinium retention, the mechanism on how gadolinium accumulates in non-enhancing gliomas is unclear. Despite the lack of contrast enhancement on conventional MRI, several studies have detected heterogeneity in non-enhancing gliomas when using dynamic perfusion-weighted MR imaging (PWI) [28,29,30]. PWI and quantitative tumor blood volume maps assess tumor vascularity and reflect the degree of angiogenesis. Therefore, although there is no obvious BBB destruction, it may be speculated that different degrees of angiogenesis and potential microleaks result in gadolinium deposits that remain, however, visually undetectable on conventional T1W MRI due to low gadolinium concentration.
To our knowledge, this is the first study to provide quantitative data of gadolinium retention in gliomas and neighboring normal brain with respect to tumor enhancement and type of GBCA used. Despite the fact that GBCAs have been used for decades in MRI of brain tumors to identify BBB breakdown and characterize tumor vasculature, only one previous study can be found where gadolinium deposits in brain tumor biopsies have been evaluated [15]. Xia et al. visually assessed gadolinium deposits in tissue sections of gliomas or other brain tumors from 28 patients using SEM/EDS. Gadolinium deposits were detected in five of these patients (two glioblastomas and three anaplastic gliomas) and were primarily found in highly vascular tumor areas and in association with calcifications. The study provided important information on the spatial occurrence of gadolinium deposits. However, contrast enhancement of the tumors was not reported. Furthermore, all patients received linear GBCA with no potential comparison between macrocyclic and linear agents.
Our study has several limitations. First, two different digestion and dilution strategies were used to measure gadolinium concentrations from the tissue samples with ICP-MS. Lower concentrations in the first set of analyses resulted in higher variability in the measurements and, therefore, the limit of detection was set at RSD 33%. This may have increased the margin of error for both false-negative and false-positive concentrations and is a major limitation of this study in general. Second, it cannot be excluded that the patients received undocumented GBCA doses given the widespread use of MRIs and the fact that we did not have access to other hospitals’ imaging archives. Since the treatment of gliomas is centralized in the university hospital, and at the time of treatment all related MRIs are transferred to its PACS, we assume this not to be a major issue regarding gadolinium retention in the tumor. However, prior GBCA exposure most likely would affect gadolinium retention in the normal brain. In our cohort, we identified one patient with available normal brain tissue who received gadoterate meglumine at the time of diagnosis, but who had been exposed to three doses of gadopentetate dimeglumine 11 years earlier. Whereas no gadolinium was detected in the tumor, the normal brain showed gadolinium at a concentration of 37 μg/kg. This normal brain specimen was excluded from analyses. However, it cannot be excluded that the remaining 13 patients with normal brain specimens were exposed to other GBCAs earlier. Third, it is unknown whether BBB in the normal tissue around the tumor was intact or compromised. Since no control subjects without brain tumor–receiving GBCA were included, it remains unclear whether normal brain gadolinium would be observed in patients without brain malignancies and definite intact BBB, or whether it is related to the tumor and/or compromised BBB. Fourth, control subjects without GBCA exposure were not included. However, because gadolinium is very rare in nature, its presence in the human body is most likely due to GBCA administration.
Conclusions
Gadolinium retention occurred both in the enhancing and non-enhancing tumors but was greatest in gliomas with noticeable enhancement as expected. In addition to tumor tissue, gadolinium was detected in the neighboring normal brain. The levels of gadolinium in the tumor and normal brain correlated suggesting a possible transit of gadolinium to the surroundings of the brain lesion. The most powerful predictor of gadolinium retention was the type of GBCA administered with significantly higher gadolinium accumulation detected with linear (gadodiamide and gadopentetate dimeglumine) relative to macrocyclic (gadoterate meglumine and gadobutrol) agents. While the clinical significance of gadolinium retention into the brain remains unsolved, the European Medicines Agency has taken a significant step and has given recommendations to suspend the usage of certain linear GBCAs related to gadolinium accumulation [31]. In USA, the US Food and Drugs Administration requires warning labeling to all GBCAs [32]. Our study elucidates gadolinium retention in brain tumors and surrounding normal tissue with an implication of higher retention associated with linear agents.
References
Idee J-M, Port M, Robic C et al (2009) Role of thermodynamic and kinetic parameters in gadolinium chelate stability. J Magn Reson Imaging 30:1249–1258
Frenzel T, Lengsfeld P, Schirmer H, Hütter J, Weinmann HJ (2008) Stability of gadolinium-based magnetic resonance imaging contrast agents in human serum at 37°C. Investig Radiol 43:817–828
Tweedle MF, Wedeking P, Kumar K (1995) Biodistribution of radiolabeled, formulated gadopentetate, gadoteridol, gadoterate, and gadodiamide in mice and rats. Investig Radiol 30:372–380
Grobner T (2006) Gadolinium—a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transplant 21:1104–1108
Kanda T, Ishii K, Kawaguchi H, Kitajima K, Takenaka D (2014) High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology 270:834–841
Errante Y, Cirimele V, Mallio CA, di Lazzaro V, Zobel BB, Quattrocchi CC (2014) Progressive increase of T1 signal intensity of the dentate nucleus on unenhanced magnetic resonance images is associated with cumulative doses of intravenously administered gadodiamide in patients with normal renal function, suggesting dechelation. Investig Radiol 49:685–690
Adin ME, Kleinberg L, Vaidya D, Zan E, Mirbagheri S, Yousem DM (2015) Hyperintense dentate nuclei on T1-weighted MRI: relation to repeat gadolinium administration. Am J Neuroradiol 36:1859–1865
Weberling LD, Kieslich PJ, Kickingereder P, Wick W, Bendszus M, Schlemmer HP, Radbruch A (2015) Increased signal intensity in the dentate nucleus on unenhanced T1-weighted images after gadobenate dimeglumine administration. Investig Radiol 50:743–748
Kanda T, Osawa M, Oba H, Toyoda K, Kotoku J’, Haruyama T, Takeshita K, Furui S (2015) High signal intensity in dentate nucleus on unenhanced T1-weighted MR images: association with linear versus macrocyclic gadolinium chelate administration. Radiology 275:803–809
Radbruch A, Weberling LD, Kieslich PJ, Eidel O, Burth S, Kickingereder P, Heiland S, Wick W, Schlemmer HP, Bendszus M (2015) Gadolinium retention in the dentate nucleus and globus pallidus is dependent on the class of contrast agent. Radiology 275:783–791
Radbruch A, Haase R, Kieslich PJ, Weberling LD, Kickingereder P, Wick W, Schlemmer HP, Bendszus M (2017) No signal intensity increase in the dentate nucleus on unenhanced T1-weighted MR images after more than 20 serial injections of macrocyclic gadolinium-based contrast agents. Radiology 282:699–707
McDonald RJ, McDonald JS, Kallmes DF et al (2015) Intracranial gadolinium deposition after contrast-enhanced MR imaging. Radiology 275:772–782
Kanda T, Fukusato T, Matsuda M, Toyoda K, Oba H, Kotoku J’, Haruyama T, Kitajima K, Furui S (2015) Gadolinium-based contrast agent accumulates in the brain even in subjects without severe renal dysfunction: evaluation of autopsy brain specimens with inductively coupled plasma mass spectroscopy. Radiology 276:228–232
Murata N, Gonzalez-Cuyar LF, Murata K, Fligner C, Dills R, Hippe D, Maravilla KR (2016) Macrocyclic and other non–group 1 gadolinium contrast agents deposit low levels of gadolinium in brain and bone tissue. Investig Radiol 51:447–453
Xia D, Davis RL, Crawford JA, Abraham JL (2010) Gadolinium released from MR contrast agents is deposited in brain tumors: in situ demonstration using scanning electron microscopy with energy dispersive X-ray spectroscopy. Acta Radiol 51:1126–1136
Thomsen, Volker; Schatzlein, Debbie; Mercuro D (2003) Limits of detection in spectroscopy. Spectroscopy 18:112–114
McDonald RJ, McDonald JS, Kallmes DF et al (2017) Gadolinium deposition in human brain tissues after contrast-enhanced MR imaging in adult patients without intracranial abnormalities. Radiology 285:546–554
Fingerhut S, Sperling M, Holling M, Niederstadt T, Allkemper T, Radbruch A, Heindel W, Paulus W, Jeibmann A, Karst U (2018) Gadolinium-based contrast agents induce gadolinium deposits in cerebral vessel walls, while the neuropil is not affected: an autopsy study. Acta Neuropathol 136:127–138
Kanda T, Nakai Y, Hagiwara A, Oba H, Toyoda K, Furui S (2017) Distribution and chemical forms of gadolinium in the brain: a review. Br J Radiol 90:20170115
Bressler JP, Olivi L, Cheong JH, Kim Y, Maerten A, Bannon D (2007) Metal transporters in intestine and brain: their involvement in metal-associated neurotoxicities. Hum Exp Toxicol 26:221–229
Öner AY, Barutcu B, Aykol Ş, Tali ET (2017) Intrathecal contrast-enhanced magnetic resonance imaging-related brain signal changes: residual gadolinium deposition? Investig Radiol 52:195–197
Berger F, Kubik-Huch RA, Niemann T, Schmid HR, Poetzsch M, Froehlich JM, Beer JH, Thali MJ, Kraemer T (2018) Gadolinium distribution in cerebrospinal fluid after administration of a gadolinium-based MR contrast agent in humans. Radiology 288:703–709
Nehra AK, McDonald RJ, Bluhm AM et al (2018) Accumulation of gadolinium in human cerebrospinal fluid after gadobutrol-enhanced MR imaging: a prospective observational cohort study. Radiology 288:416–423
Iliff JJ, Lee H, Yu M, Feng T, Logan J, Nedergaard M, Benveniste H (2013) Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J Clin Invest 123:1299–1309
Robert P, Lehericy S, Grand S, Violas X, Fretellier N, Idée JM, Ballet S, Corot C (2015) T1-weighted hypersignal in the deep cerebellar nuclei after repeated administrations of gadolinium-based contrast agents in healthy rats. Investig Radiol 50:473–480
Lohrke J, Frisk A-L, Frenzel T, Schöckel L, Rosenbruch M, Jost G, Lenhard DC, Sieber MA, Nischwitz V, Küppers A, Pietsch H (2017) Histology and gadolinium distribution in the rodent brain after the administration of cumulative high doses of linear and macrocyclic gadolinium-based contrast agents. Investig Radiol 52:324–333
Yoo R-E, Sohn C-H, Kang KM, Yun TJ, Choi SH, Kim JH, Park SW (2018) Evaluation of gadolinium retention after serial administrations of a macrocyclic gadolinium-based contrast agent (gadobutrol). Investig Radiol 53:20–25
Morita N, Wang S, Chawla S, Poptani H, Melhem ER (2010) Dynamic susceptibility contrast perfusion weighted imaging in grading of nonenhancing astrocytomas. J Magn Reson Imaging 32:803–808
Fan GG, Deng QL, Wu ZH, Guo QY (2006) Usefulness of diffusion/perfusion-weighted MRI in patients with non-enhancing supratentorial brain gliomas: a valuable tool to predict tumour grading? Br J Radiol 79:652–658
Batra A, Tripathi RP, Singh AK (2004) Perfusion magnetic resonance imaging and magnetic resonance spectroscopy of cerebral gliomas showing imperceptible contrast enhancement on conventional magnetic resonance imaging. Australas Radiol 48:324–332
EMA (2017) EMA’s final opinion confirms restrictions on use of linear gadolinium agents in body scans. In: https://www.ema.europa.eu/documents/press-release/emas-final-opinion-confirms-restrictions-use-linear-gadolinium-agents-body-scans_en.pdf
FDA (2017) FDA drug safety communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warnings. In: https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm
Acknowledgements
Open access funding provided by University of Turku (UTU) including Turku University Central Hospital.
Funding
This study was funded by EVO research funding from the Southwest Finland Hospital District (AK) and a grant from the Cancer Societies of Southwest Finland (MG).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of retrospective study formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
OpenAccess This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kiviniemi, A., Gardberg, M., Ek, P. et al. Gadolinium retention in gliomas and adjacent normal brain tissue: association with tumor contrast enhancement and linear/macrocyclic agents. Neuroradiology 61, 535–544 (2019). https://doi.org/10.1007/s00234-019-02172-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-019-02172-6