Abstract
Objective
To characterize hemodynamic changes during experimental aspiration pneumonitis, paying special attention to echocardiographic assessment.
Design and setting
Animal study in a university-based research laboratory.
Subjects
Fourteen mechanically ventilated New Zealand white rabbits
Interventions
We instilled 1 ml/kg human gastric juice (mean pH: 4.1 + 0.2) intratracheally. Hemodynamic and respiratory parameters were measured every hour for 4 h, associated with a transthoracic echocardiography.
Measurements and results
Lung injury occurred within 1 hour with a marked decrease in PaO2/FIO2 and an increase in plateau pressure; after this initial drop the ratio remained stable throughout the experiment. Seven rabbits experienced only a mild to moderate alteration in lung oxygenation function as defined by a PaO2/FIO2 ratio above 200 (group A), while the other seven developed a severe alteration with a ratio below 200 (group B). At the end of the experiment pH and cardiac output were lower in group B than in group A. Using a PaO2/FIO2 threshold value of 150, pH, mean arterial pressure, and cardiac output were lower in the animals with the more severe hypoxemia. Neither left nor right ventricular dysfunction occurred during the experiment, and no animal experienced circulatory failure
Conclusion
Experimental aspiration pneumonitis after intratracheal infusion of human gastric juice is characterized by a stable fall in PaO2/FIO2. Animals with the most severe lung injury experienced a lower systemic arterial pressure, cardiac output, and metabolic acidosis without circulatory failure or cardiac dysfunction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult acute lung injury/acute respiratory distress syndrome (ALI/ARDS) has numerous pulmonary and extrapulmonary causes but occurs rather frequently after sepsis or aspiration of gastric contents [1, 2, 3, 4]. In addition to pulmonary injury, patient outcome may be altered by coexisting circulatory failure due to systemic inflammatory response [5], pulmonary hypertension, left and/or right ventricular dysfunction [6, 7], and due to the hemodynamic deleterious effects of mechanical ventilation [3, 8, 9]. At the origin of circulatory failure, right heart failure and pulmonary hypertension occur in approx. 25% of ALI/ARDS cases in adults [10] and are correlated with the severity of lung injury [11] and with outcome [3, 12].
Aspiration of gastric contents causes aspiration pneumonitis [13] and is the cause of ALI/ARDS in 9–19% of cases [4], especially in mechanically ventilated patients [14]. It combines caustic effects and the chemical and inflammatory effects of enzymes and particulates of the gastric juice [13, 15, 16]. In clinical and in experimental studies on aspiration pneumonitis there is scarce information on the frequency and the precise pathogenesis of circulatory failure [14, 16, 17, 18]. Because the gastric contents aspiration model of acute respiratory failure is particularly relevant for its clinical implication, it seems of paramount importance to clarify its hemodynamic profile. Therefore we designed this experimental animal model to characterize the mechanism, extent, and variability in hemodynamic changes during the acute phase of aspiration pneumonitis, paying special attention to the effect of alteration in lung oxygenation function on the hemodynamic profile.
Materials and methods
Human gastric content preparation
Human gastric content was collected during the first hours following admission from 14 patients requiring mechanical ventilation in the intensive care unit via nasogastric tube. No antacid was administered before gastric content collection. The gastric juice was sampled for bacteriological analysis, and initial bacterial cultures were negative. To obtain different degrees of respiratory response after gastric juice inhalation than in the clinical setting, samples were not pooled. They were aliquoted and stored at −80°C. At the time of the experiment the aliquots were thawed until particulates self-sedimented in the bottom of the tube. The water fraction was then sampled and filtrated through a sterile gauze sponge to remove debris. Measurement of the pH was performed (mean 4.1 ± 0.2). A second bacteriological culture of gastric juice samples was negative in all cases.
Animal preparation
Fourteen New Zealand white rabbits (Charles River Laboratories, l'Abresle, France) weighing 2.5–3.3 kg (mean 2.7 kg) were studied. Baseline characteristics of the 14 animals are reported in Table 1. The protocol conformed to the guidelines laid out in the Guide for the Care and Use of Laboratory Animals [19] and was approved by the animal research committee of the Université de la Méditerranée, Marseille, France. The animals were anesthetized with intravenous injection of ethylcarbamate (Urethane at 1 g/kg) into an ear vein. Continuous infusion of saline was initially set at 5 ml/kg per hour. Body temperature was continuously monitored and held between 37.5°C and 38.5°C by a thermostatically controlled heating pad. Tracheotomy was performed. A pediatric endotracheal tube (4 mm diameter) was inserted and connected to the ventilator (Servo 900c (Siemens-Elema, Solna, Sweden)). Animals were left in supine position.
Aspiration pneumonitis usually occurs in conventionally mechanically ventilated patients [13] during the perioperative period with a tidal volume (Vt) around 10 ml/kg and often without positive end-expiratory pressure (PEEP) [20]. Hence to reproduce this clinical setting volume-controlled ventilation was deliberately used with Vt set at 10 ml/kg and without PEEP at the beginning and also throughout the experiment since in the present study we did not aim to test any lung protective ventilation in ARDS. The respiratory rate and fraction of inspired oxygen (FIO2) were initially fixed at 40 cycles/min and 21%, respectively. The animals were paralyzed with vecuronium bromide 0.2 mg/kg, followed by hourly injections of 0.2 mg/kg. A catheter was inserted into the right femoral artery for collection of blood samples and measurement of blood pressure.
Measurements of blood pressure, pulmonary gas exchanges, and mechanical ventilation
Systemic arterial pressure was continuously monitored with a calibrated pressure transducer. Blood was taken hourly for measurements of pH, arterial blood oxygen tension (PaO2), and arterial blood carbon dioxide tension (PaCO2) with an automatic blood gas analyzer (ABL 330, Radiometer, Copenhagen, Denmark).
Echocardiographic measurements
Each rabbit underwent Doppler echocardiographic examination at baseline and every hour by an experienced echocardiographer (A.F.). Commercially available echocardiographic equipment (Cypress, Siemens) with a 7.5-MHz tranthoracic transducer was used. Based on previous study that has shown reliable calculation of left ventricular volume, function and cardiac output (CO) in the rabbit [21], the left ventricular ejection fraction (LVEF) was calculated by the modified Teicholz formula, and CO was quantified by using the following measurements: aortic or pulmonary artery annulus diameter; Doppler aortic or pulmonary flow at the level of the annulus followed by measurement of the velocity time integral (VTI) at the end expiratory level; CO = VTI × π (D2)/4 × heart rate. The annulus diameter was measured in end-systole since this is not subject to change significantly during the respiratory cycle [8]. Right ventricular systolic function was determined qualitatively (graded as normal, mildly, moderately, or severely depressed) by two-dimensional echocardiography. The degree of tricuspid regurgitation was graded as none, mild, moderate, or severe according to the ratio of the regurgitant jet area to the right atrial area with color Doppler. Systolic pulmonary artery pressure (SPAP) was measured by applying the modified Bernoulli equation to the peak velocity of tricuspid regurgitation: p = 4v2, where p is peak pressure drop from the right ventricle to the right atrium and v is peak velocity of tricuspid regurgitation (m/s). Each echocardiographic and Doppler measurement is presented as the average of three measurements.
Echocardiography was also used to qualitatively assess the need for fluid resuscitation in cases of hemodynamic impairment. A partial inspiratory collapse of the superior vena cava was considered as a sign for decrease in right ventricular preload [9].
Experiment protocol
A recruitment maneuver was performed to standardize lung volume history just before gastric juice instillation. This consisted in two 10-s dynamic sustained inflations with a mean airway pressure of 25 cmH2O. Then a 5-F intratracheal catheter was inserted into the trachea; its position was checked by transillumination, and 1 ml/kg gastric content was intratracheally instilled (one-half of the volume in each lung). The animal was then gently rocked on both sides, and another recruitment maneuver was performed to widespread gastric juice in the lungs. Mechanical ventilation was pursued for 4 h or until death. The initial ventilator settings were maintained except the respiratory rate that was adjusted to maintain PaCO2 at 30–40 mmHg and the FIO2 that was increased to maintain a PaO2 above 60 mmHg when possible. The hemodynamic and respiratory parameters were determined every hour, in association with echocardiography.
This protocol was preliminarily tested in five test animals not included in the present study. This assessment showed that intratracheal instillation of 1 ml/kg gastric juice induced a well tolerated acute pulmonary inflammatory injury characterized by a decrease in pulmonary gas-exchange efficiency. After killing of the animals histopathological examination showed a bilateral and homogeneous distribution of alveolar damages characteristics of ALI. To assess whether the cardiopulmonary response is related to the severity of lung injury the animals with the greatest deterioration in lung oxygenation function (group B) were compared with the others (group A) based on clinical studies that define ARDS by a PaO2/FIO2 ratio less than 200 [3, 4, 8]. A PaO2/FIO2 threshold value of 150 was also assessed since this cutoff is readily used to characterize severe ARDS [22, 23]. In the case of a significant drop in mean arterial pressure (MAP) or CO during the experiment 10 ml/kg saline was infused when inspiratory superior vena cava collapse was diagnosed by echocardiography. Circulatory failure was defined as the need for hemodynamic support by a vasoactive agent to maintain MAP above 65 mmHg despite adequate fluid resuscitation. The two groups did not significantly differ in any baseline parameter. All the animals in group A completed the experiment, but two animals in group B died prematurely from sudden cardiac arrest with profound hypoxemia (last PaO2 at 41 and 39 mmHg, respectively); the cardiac arrest was not preceded by circulatory failure or ventricular dysfunction by echocardiography.
Lung processing
At the end of the experiment midline sternotomy was performed, and the lungs were checked for evidence of pneumothorax. The animals were killed by an intracardiac overdose of 5% pentobarbital sodium. The lungs were clamped at the hilum at end-inspiration. In two animals of each group the lungs were filled with 10% buffered formalin at a transpulmonary pressure of 15 cmH2O via a 3-F catheter for histological analysis.
Statistical analysis
Data for continuous variables are presented as means ± SEM. Data analysis was performed using SPSS version 13.0 (SPSS, Chicago, Ill., USA). The nonparametric Wilcoxon test was used to compare values on continuous variables between the two groups. The nonparametric Wilcoxon test for paired data was used to test repeated measures. When a parameter was measured twice only (i.e., pulmonary mechanics), comparisons over time were also assessed by the Wilcoxon test for paired data. A p value less than 0.05 was considered as statistically significant.
Results
Pulmonary changes
Baseline characteristics of the 14 animals are reported on Table 1. Inhalation of human gastric juice altered the lung oxygenation function within 1 hour (Fig. 1) as reflected by marked decrease in PaO2/FIO2 (p = 0.01) and increase in Pplat (p = 0.02). Seven rabbits experienced a mild to moderate lung injury as defined by a PaO2/FIO2 ratio higher than 200 (group A) while the other seven developed a severe lung injury with a PaO2/FIO2 ratio less than 200 (group B). Of particular interest, the ratio remained stable throughout the experiment in both groups after the initial drop (Fig. 1a). Lung injury was characterized by focal acute inflammatory changes. Macroscopically they showed massive consolidation that involved more than 70% of lung volume with predominance in posterior and dependent areas. Damage was characterized by hemorrhage, inflammatory cell recruitment (polynuclears), and hyaline membranes and was predominant in lower and middle lobes while upper lobes were almost normal (Fig. 2).
Lung injury parameters in rabbits (n = 14) during the course of the experiment. a Mean arterial partial pressure of oxygen fraction/fraction of inspired oxygen (PaO2/FIO2). b Mean plateau pressure (Pplat). Values at baseline represent conditions before the inhalation of human gastric juice. For PaO2/FIO2 and Pplat the difference by Wilcoxon test between baseline and 1 hour was significant (p = 0.01 and 0.02, respectively)
Two representative lung microphotographs (light microscopy) after tracheal instillation of 1 ml/kg human gastric juice in rabbits with mild to moderate (a) and severe (b) lung injury; hematoxylin and eosin × 400. a The inflammatory response (arrows polynuclears) was moderate and hyaline membranes were observed. b Inflammation and hemorrhage were more intense, and edema was present. RBC Red blood cells; Hy hyaline membranes; E edema
Metabolic and cardiovascular response
Baseline LVEF, CO, and SPAP were normal in all the cases (Table 1), without significant differences between the two groups. At the end of the experiment group B animals had significantly lower pH than in group A (Fig. 3). There was no need for hemodynamic support by a vasoactive agent to maintain adequate MAP during the experiment in any group. All together, the animals' SPAP increased from 16.4 ± 0.9 mmHg at baseline to 21.3 ± 1.4 mmHg at the end of the experiment (p = 0.002). However, SPAP did not differ significantly between the two groups at anytime. CO decreased in group B but tended to increase in group A, resulting in values significantly lower (Fig. 4). LVEF did not differ significantly in either group throughout the experiment. Using a PaO2/FIO2 threshold of 150, animals with a PaO2/FIO2 ratio less than 150 (n = 6) had significantly lower pH, MAP, and CO at the end of the experiment (p < 0.05). Qualitatively, right ventricular systolic function was normal at baseline and throughout the experiment in all the cases. No abnormal septal motion or right ventricular dilation was seen during the experiment. No animal had a more than mild tricuspid regurgitation at baseline and throughout the experiment.
Discussion
The present study shows that tracheal instillation of 1 ml/kg gastric contents in rabbits induces lung injury characterized by (a) a wide range of PaO2/FIO2 decrease within 1 hour after inhalation followed by a stability that was sustained over the rest of the experiment, (b) a mild elevation in SPAP without right heart failure, and (c) in the animals with the most severe lung injury a lower MAP, CO, and metabolic acidosis but without circulatory failure.
The pulmonary response to tracheal instillation of gastric juice that we observed here is characteristic of ARDS with a decreased PaO2/FIO2 and an increased Pplat. Histological findings were similar to what is commonly reported after aspiration pneumonitis (Fig. 2) showing pulmonary edema, hemorrhage, necrosis, inflammatory cells infiltrates [24]. It confirms the reliability of this model in producing damage characteristic of ARDS. The animal-to-animal variability in the PaO2/FIO2 decrease reflects what is observed in clinical practice [25]. Importantly, nonprotective ventilation was used in our experiment (Vt at 10 ml/kg without PEEP), a clearly harmful ventilation in ARDS [3, 4]. The application of PEEP in ARDS/ALI allows reinflation of the collapsed lung segments and improvement in the ventilation/perfusion relationship of areas with low ventilation/perfusion ratios [26]. In clinical setting a lung-protective ventilation strategy with a Vt of 6 ml/kg has been shown significantly to reduce mortality compared with volumes of 12 ml/kg [27]. However, the effects of elevated PEEP and low Vt are not widely studied in experimental ARDS/ALI, especially in small animal models. In a rabbit model of ALI circulatory failure occurred with elevated PEEP (10 cmH2O) and low Vt (6 ml/kg) [28], whereas adult patients with ARDS generally do not experience hemodynamic instability when ventilated with high PEEP. In our experiment conventional mechanical ventilation at high volumes certainly aggravated the lung injury through volutrauma but did not induce circulatory failure.
Several factors can affect the severity of lung injury after gastric juice instillation into the trachea: a more acidic pH and the size and the amount of gastric particles and the volume instilled [16, 29, 30]. In the present study, after the initial drop, the level of PaO2/FIO2 was very stable throughout the study period for a given animal. This is different from other animal models of ALI/ARDS where a wide range of hypoxemia has been documented, with or without compromised cardiovascular performance [31]. In our model the variability in respiratory response mimics that which is seen in clinical practice and provides the opportunity to assess various diagnostic tools and therapies within this wide range of gas exchange impairment. The stability of the respiratory parameters after the initial response should facilitate experimental diagnostic and therapeutic studies with this model.
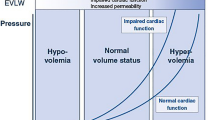
In our experiment animals with the greatest degree of lung injury experienced metabolic acidosis, lower CO, and even lower MAP when a PaO2/FIO2 threshold of 150 was chosen. In addition a mild but significant elevation in SPAP was documented throughout the experiment. Nevertheless, circulatory failure as defined by the need for hemodynamic support by a vasoactive agent [3] did not occur. However, maintaining a PaO2 above 60 mmHg, as stated in our experiment protocol, could favor hemodynamic stability. The fact that the two more hypoxemic animals (PaO2 41 and 39 mmHg, respectively, on FIO2 = 1.0) died abruptly from sudden cardiac arrest without any documented hemodynamic/echocardiographic changes prior to death seems to argue for the absence of major influence of our supplemental oxygen strategy on the hemodynamic outcome. Several factors can contribute to circulatory failure in lung injury. Pulmonary production of inflammatory mediators and overspill of these agents into the systemic circulation can cause hypotension and ultimately multiple organ failure [5]. Also, many factors can induce left and/or right ventricular dysfunction: hypoxemia causing generalized myocardial ischemia, pulmonary hypertension, sepsis, and metabolic acidemia [6, 7]. Finally, mechanical ventilation by itself can potentially compromise hemodynamics by increasing right ventricular afterloading [3, 8] and impairing venous return from superior vena cava [9], thus decreasing the filling reserve for the left ventricle. In the present study the absence of right ventricular dysfunction is in contrast with some experimental and clinical studies which have documented right ventricular failure in ALI and ARDS [10, 31]. Clinical findings in ARDS patients show an incidence of approx. 25% of pulmonary hypertension and right heart failure [10]. However, one striking difference is that our model of aspiration pneumonitis contains no bacteria [13] and differs from "septic" condition of ARDS in which endotoxin favors pulmonary vasocontriction and then hypertension [32]. In our experiment the decrease in CO and MAP cannot be attributed to the development of cardiac dysfunction. Hence it is reasonable to hypothesize that it was rather due to systemic inflammatory response with vasoplegia and/or to impairment of venous return from superior vena cava due to increased intrathoracic pressure.
In ARDS the management of patients with compromised circulatory status is often based on information provided by right heart catheterization [33] or by echocardiographic evaluation [3, 12]. Although measurements of LVEF, CO, and SPAP have been validated in the normal rabbit [23, 34], the value of the various Doppler echocardiographic measurements has not been established in experimental ALI/ARDS. Several approaches have been focused on right ventricular function [35, 36] because ARDS may induce acute cor pulmonare [10]. However, assessment of the right ventricular function by echocardiography is difficult due to its complex geometric shape. Moreover, right ventricular ejection fraction is at least twice as sensitive as LVEF to changes in ventricular afterload [37]. Finally, in the setting of an intensive care unit one needs to know a relatively simple and fast method to assess right ventricular function in unstable patients with ARDS. This is what we aimed to do in our study by assessing right ventricular function qualitatively [36] or indirectly by the importance of tricuspid regurgitation [38].
In the present study the lack of mechanistic study on gastric juice represents a limitation. Indeed, in addition to the pH value, the presence of small particles of 2–30 μm causes lung inflammation that is distinct from the acidic component of the gastric aspirate [30]. Further work should investigate particulate matter to properly conduct mechanistic studies.
Conclusions
Intratracheal infusion of 1 ml/kg human gastric juice in mechanically ventilated rabbits consistently results in a model of lung injury picture remarkable by its stability over 4 h with regard to the PaO2/FIO2 ratio and hemodynamic measurements. Hemodynamic compromise occurred in the animals presenting the more altered respiratory status, presumably via mechanisms different from hypoxemia, but without circulatory failure.
References
Hudson LD, Steinberg KP (1999) Epidemiology of acute lung injury and ARDS. Chest 116:74S–82S
Montgomery AB, Stager MA, Carrico CJ, Hudson LD (1985) Causes of mortality in patients with the adult respiratory distress syndrome. Am Rev Respir Dis 132:485–489
Page B, Vieillard-Baron A, Beauchet A, Aegerter P, Prin S, Jardin F (2003) Low stretch ventilation strategy in acute respiratory distress syndrome: eight years of clinical experience in a single center. Crit Care Med 31:765–769
Estenssoro E, Dubin A, Laffaire E, Canales H, Saenz G, Moseinco M, Pozo M, Gomez A, Baredes N, Jannello G, Osatnik J (2002) Incidence, clinical course, and outcome in 217 patients with acute respiratory distress syndrome. Crit Care Med 30:2450–2456
Goodman RB, Pugin J, Lee JS, Matthay MA (2003) Cytokine-mediated inflammation in acute lung injury. Cytokine Growth Factors Rev 14:523–535
Malbouisson LM, Busch CJ, Puybasset L, Lu Q, Cluzel P, Rouby JJ, and the CT Scan ARDS Study Group (2000) Role of the heart in the loss of aeration characterizing lower lobes in acute respiratory distress syndrome. Am J Respir Crit Care Med 161:1005–1012
Jardin F, Brun-Ney B, Auvert B, Beauchet A, Bourdarias JP (1990) Sepsis-related cardiogenic shock. Crit Care Med 18:1055–1060
Vieillard-Baron A, Loubières Y, Schmitt JM, Dubourg O, Jardin F (1999) Cyclic changes in right ventricular output impedance during mechanical ventilation. J Appl Physiol 87:1644–1650
Vieillard-Baron A, Augarde R, Prin S, Page B, Beauchet A, Jardin F (2001) Influence of superior vena caval zone condition on cyclic changes in right ventricular outflow during respiratory support. Anesthesiology 95:1083–1088
Vieillard-Baron A, Schmitt JM, Augarde R, Desfonds P, Page B, Beauchet A, Jardin F (2002) Acute cor pulmonare in acute respiratory distress syndrome submitted to protective ventilation: incidence, clinical implications, and prognosis. Crit Care Med 29:1551–1555
Zapol WM, Snider MT (1977) Pulmonary hypertension in severe acute respiratory failure. N Engl J Med 296:476–480
Jardin F, Gueret P, Dubourg O, Farcot JC, Margairaz A, Bourdarias JP (1985) Two-dimensional echocardiographic evaluation of right ventricular size and contractility in acute respiratory failure. Crit Care Med 13:952–956
Marik PE (2001) Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 344:665–671
Warner MA, Warner ME, Weber JG (1993) Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology 78:56–62
Davidson BA, Knight PR, Wang Z, Chess PR, Holm BA, Russo TA, Hutson A, Notter RH (2005) Surfactant alterations in acute inflammatory lung injury from aspiration of acid and gastric particulates. Am J Physiol Lung Cell Mol Physiol 288:L699–L708
Davidson BA, Knight PR, Paul R, Nader ND, Shanley TP, Johnson KJ (1999) The role of tumor necrosis factor in the pathogenesis of aspiration pneumonitis in rats. Anesthesiology 91:486–499
Hamelberg W, Bosomworth PP (1964) Aspiration pneumonitis: experimental studies and clinical observations. Anesth Analg 43:669–677
Fabre J, Martin C, Pomane C, Long P, François G (1984) The early period of experimental Mendelson's syndrome in dogs with PaCO2 and pH in the normal range. Resuscitation 11:103–110
Institute of Laboratory Animals Resources Commission on Life Sciences (1996) Guide for the care and use of laboratory animals. National Research Council, National Academy Press, Washington
Boker A, Haberman CJ, Girling L, Guzman RP, Louridas G, Tanner JR, Cheang M, Maycher BW, Bell DD, Doak GJ (2004) Variable ventilation improves perioperative lung function in patients undergoing abdominal aneurysmectomy. Anesthesiology 100:608–616
Pye MP, Black M, Cobbe SM (1996) Comparison of in vivo and in vitro haemodynamic function in experimental heart failure: use of echocardiography. Cardiovasc Res 31:873–881
Michard F, Wolff MA, Herman B, Wysocki M (2001) Right ventricular response to high-dose almitrine infusion in patients with severe hypoxemia related to acute respiratory distress syndrome. Crit Care Med 29:32–36
Papazian L, Gainnier M, Marin V, Donati S, Arnal JM, Demory D, Roch A, Forel JM, Bongrand P, Bregeon F, Sainty JM (2005) Comparison of prone positioning and high-frequency oscillatory ventilation in patients with acute respiratory distress syndrome. Crit Care Med 33:2162–2171
Teabeaut JRII (1952) Aspiration of gastric contents an experimental study. Am J Pathol 28:51–67
Brun-Buisson C, Minelli C, Bertolini G, Brazzi L, Pimentel J, Lewandowski K, Bion J, Romand JA, Villar J, Thorsteinsson A, Dan Armaganidis A, Lemaire F ALIVE Study Group (2004) Epidemiology and outcome of acute lung injury in European intensive care units: Results from the ALIVE study. Intensive Care Med 30:51–61
Räsänen J, Gavriely N (2005) Response of acoustic transmission to positive airway pressure therapy in experimental lung injury. Intensive Care Med 31:1434–1441
Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Rotta AT, Gunnarson B, Fuhrman BP, Hernan L, Steinhorn DM (2001) Comparison of lung protective ventilation strategies in a rabbit model of acute lung injury. Crit Care Med 29:2176–2184
Kennedy TP, Johnson KJ, Kunkle RG, Ward PA, Knight PR, Finch JS (1989) Acute acid aspiration lung injury in the rat: biphasic pathogenesis. Anesth Analg 69:87–92
Knight PR, Rutter T, tait AR, Coleman EC, Johnson K (1993) pathogenesis of gastric particulate lung injury: a comparison and interaction with acidic pneumonitis. Anesth Analg 77:754–760
Rosenthal C, Caronia C, Quinn C, Lugo N, Mayer S (1998) A comparison among animal models of acute lung injury. Crit Care Med 26:912–916
Gerbino AJ, McKinney S, Glenny RW (2000) Correlation between ventilation and perfusion determines VAQ heterogeneity in endotoxemia. J Appl Physiol 88:1933–1942
Vieillard-Baron A, Girou E, Valente E, Brun Buisson C, Jardin F, Lemaire F, Brochard L (2000) Predictors of mortality in acute respiratory distress syndrome. Focus on the role of right heart catheterization. Am J Respir Crit Care Med 161:1597–1601
Slama M, Masson H, Teboul JL, Arnout ML, Susic D, Frohlich E, Andrejak M (2002) Respiratory variations of aortic VTI: a new index of hypovolemia and fluid responsiveness. Am J Physiol Heart Circ Physiol 283:H1729–H1733
Uchida T, Ichikawa K, Yokohama K, Mitaka C, Toyooka H, Amaha K (1996) Inhaled nitric oxide improved the outcome of severe right ventricular failure caused by lipopolysaccharide administration. Intensive Care Med 22:1203–1206
Duggan M, McCaul CL, McNamara PJ, Engelberts D, Ackerley C, Kavanagh BP (2003) Atelectasis causes vascular leak and lethal right ventricular failure in uninjured rats lungs. Am J Respir Crit Care Med 167:1633–1640
Weber KT, Janicki JS, Shroff S, Fishman AP (1981) Contractile mechanics and interactions of the right and left ventricles. Am J Cardiol 47:686–695
Aziz TM, Saad RA, Burgess MI, Campbell CS, Yonan NA (2002) Clinical significance of tricuspid valve dysfunction after orthotopic heart transplantation. J Heart Lung Transplant 21:1101–1108
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fraisse, A., Bregeon, F., Delpierre, S. et al. Hemodynamics in experimental gastric juice induced aspiration pneumonitis. Intensive Care Med 33, 300–307 (2007). https://doi.org/10.1007/s00134-006-0457-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0457-2