Abstract
Aims/hypothesis
Ideal cardiovascular health (CVH) is associated with lower diabetes risk. However, it is unclear whether this association is similar across glycaemic levels (normal [<5.6 mmol/l] vs impaired fasting glucose [IFG] [5.6–6.9 mmol/l]).
Methods
A secondary data analysis was performed in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Incident diabetes was assessed among 7758 participants without diabetes at baseline (2003–2007) followed over 9.5 years. Baseline cholesterol, blood pressure, diet, smoking, physical activity and BMI were used to categorise participants based on the number (0–1, 2–3 and ≥4) of ideal CVH components. Risk ratios (RRs) were calculated using modified Poisson regression, adjusting for cardiovascular risk factors.
Results
Among participants (mean age 63.0 [SD 8.4] years, 56% female, 73% white, 27% African-American), there were 891 incident diabetes cases. Participants with ≥4 vs 0–1 ideal CVH components with normal fasting glucose (n = 6004) had 80% lower risk (RR 0.20; 95% CI 0.10, 0.37), while participants with baseline IFG (n = 1754) had 13% lower risk (RR 0.87; 95% CI 0.58, 1.30) (p for interaction by baseline glucose status <0.0001). Additionally, the magnitude of the association of ideal CVH components with lower diabetes risk was stronger among white than African-American participants (p for interaction = 0.0338).
Conclusions/interpretation
A higher number of ideal CVH components was associated with a dose-dependent lower risk of diabetes for participants with normal fasting glucose but not IFG. Tailored efforts that take into account observed differences by race and glycaemic level are needed for the primordial prevention of diabetes.
Similar content being viewed by others

Introduction
The American Heart Association (AHA) published 2020 Impact Goals for cardiovascular health (CVH) promotion aiming to improve CVH and reduce deaths from cardiovascular disease (CVD) and stroke by 20% from 2010 to 2020 [1]. Through this effort, the AHA identified ideal levels of seven health factors or behaviours that have been associated with healthy ageing without cardiovascular and other chronic diseases (also known as ‘Life’s Simple 7’) [1]. The health factors include total cholesterol <5.18 mmol/l, blood pressure <120/<80 mmHg and fasting plasma glucose <5.6 mmol/l, all without the use of medication. The health behaviours include a healthy dietary pattern, no prior tobacco use or having stopped smoking more than 12 months previously, ≥150 min/week of moderate intensity or ≥75 min/week of vigorous intensity physical activity and BMI <25 kg/m2. Adherence to these factors and behaviours has been associated with a lower incidence of CVD and all-cause mortality [2, 3].
There are many shared cardiovascular and diabetes risk factors, and we have previously shown that attainment of a higher number of ideal CVH factors is associated with lower risk of diabetes in multi-ethnic populations, with a greater magnitude of risk reduction among non-Hispanic white participants [4, 5]. Recent analyses have challenged whether attainment of more optimal levels of classic risk factors is associated with similar risk reductions among individuals with lower or higher diabetes risk [5, 6]. Thus, we examined whether the association of ideal CVH with diabetes risk differed for participants with higher levels of diabetes risk (i.e. impaired fasting glucose [IFG], African-Americans) compared with participants at lower baseline risk (i.e. normal fasting glucose, whites).
Methods
This paper reports the results of a secondary analysis of data from the REGARDS cohort. The REGARDS study is a prospective national cohort of 30,239 community-dwelling African-American and white adults ≥45 years of age from the 48 contiguous US states that was designed to examine regional and racial influences on stroke mortality [7, 8]. Full details are described elsewhere [7]. Briefly, participants—English-speaking adults aged 45 years or older—were enrolled between January 2003 and October 2007, with commercially available lists combining mail and telephone contacts used for recruitment. Race and sex were balanced by design, with oversampling from the south-eastern USA; the final cohort composition was 58% women and 42% African-American. Overall, 56% of participants resided in the stroke belt (NC, SC, GA, AL, MS, TN, AR and LA) with the rest from the other 40 contiguous states. An initial telephone interview was used to survey participants and establish eligibility. Following verbal consent, demographic information and medical history, including data on stroke risk factors and sociodemographic, lifestyle and psychosocial characteristics were collected via computer-assisted telephone interviews using validated questionnaires. Participants were asked to fast for 10–12 h and physical and physiological measures including BP, anthropometric measures, blood samples, urine samples, electrocardiogram and medication use by pill bottle review were collected during an in-home examination by trained staff following standardised, quality-controlled protocols. Blood and urine samples were shipped overnight on ice to the REGARDS central laboratory in Burlington, VT, USA. Participants were contacted via telephone at 6 month intervals to ascertain hospitalisations and vital status. A second in-person assessment was conducted 10 years (2013–2016) following baseline and included a telephone interview and an in-home examination to collect physical and physiological measures. Study methods were reviewed and approved by the institutional review board at the participating institutions and all participants gave written informed consent.
Exposure
The primary exposure was ideal CVH, assessed using six baseline metrics: cigarette smoking status; diet; physical activity; BMI; serum cholesterol; and blood pressure [4]. The blood glucose metric was excluded in the analyses, as diabetes was the outcome of interest. Each baseline metric was evaluated separately using poor, intermediate and ideal categories (electronic supplementary material [ESM] Table 1) [1]. Additionally, the number of ideal CVH metrics was summed across the six individual metrics and categorised as poor (0–1 ideal metrics), intermediate (2–3 ideal metrics) and ideal (4+ ideal metrics) CVH [4].
Cigarette smoking
Self-reported cigarette smoking was categorised as: current = poor; former ≤12 months (smoking at least 100 cigarettes in a lifetime) = intermediate; or never or quit ≥12 months = ideal.
Dietary intake
Dietary intake was assessed with the Block 98 food frequency questionnaire (FFQ), a validated semi-quantitative FFQ that assessed usual dietary intake of 110 food items (NutritionQuest, Berkeley, CA, USA) [9]. The FFQ was self-administered by participants after the baseline in-home visit and mailed to the REGARDS operations centre, where it was checked for completeness, scanned and forwarded to NutritionQuest for processing and analysis. The amounts of each food on the FFQ consumed by a participant were calculated by multiplying the frequency of consumption of that food by the usual amount consumed; the food groups were constructed as has been described previously [10]. The REGARDS questionnaire had some slight differences from the 2020 guidelines regarding units of servings, which required modification of the metrics. Components of the modified ideal diet score were: fruits and vegetables ≥4.5 cups/day; fish ≥2 × 98 g servings per week (non-fried); fibre-rich whole grains ≥3 × 28 g-equivalent servings/day; sodium <1500 mg/day; and sugar-sweetened beverages ≤1884 kJ/week. Participants were given one point per dietary component at goal for a total score ranging from 0 to 5. Participants were classified as ideal (4–5 of 5 components), intermediate (2–3 of 5 components) or poor (0–1 of 5 components).
Physical activity
Participants in REGARDS were asked ‘How many times per week do you engage in intense physical activity, enough to work up a sweat?’ We defined ideal physical activity as a frequency of four or more times per week, intermediate as 1–3 times per week, and poor as none, as previously [11].
Serum cholesterol, BMI, BP, plasma glucose
Serum concentrations of total cholesterol were measured using colorimetric reflectance spectrophotometry. Poor, intermediate and ideal levels of total cholesterol were categorised as ≥6.21 mmol/l, 5.18–<6.21 mmol/l or treated to goal, < 5.18 mmol/l, respectively. Calibrated devices were used to measure participants’ weight and height to calculate BMI as weight (kg)/height2 (m2). BMI was categorised as poor, intermediate and ideal as follows: ≥30 kg/m2, 25–29.9 kg/m2 and <25 kg/m2, respectively. Resting seated BP was measured following a standard protocol in the left arm. The average of two seated BP measurements was used for analysis. BPs were categorised as poor, intermediate and ideal as follows: systolic (S)BP ≥140 or diastolic (D)BP ≥90 mmHg, SBP 120–139 or DBP 80–89 mmHg or treated to goal, <120/<80 mmHg, respectively. Fasting plasma glucose was categorised as intermediate or ideal as 5.6–6.9 mmol/l and <5.6 mmol/l, respectively. Because participants with diabetes at baseline were excluded from this analysis, no participants were in the poor category for glucose (≥7.0 mmol/l).
Outcome
The primary outcome was incident diabetes, defined as fasting glucose ≥7.0 mmol/l, non-fasting glucose ≥11.1 mmol/l or diabetes medication use at the follow-up examination in those without prevalent diabetes at baseline. Glucose was measured using colorimetric reflectance spectrophotometry on the Ortho Vitros 950 IRC Clinical Analyzer (Johnson & Johnson Clinical Diagnostics, Rochester, NY, USA) with a coefficient of variation of 1% [12].
Covariates
Age, race, sex, annual household income and education were self-reported. Self-reported alcohol use was categorised as none, moderate (1–7 drinks/week for women or 1–14 drinks/week for men) or heavy (>7 drinks/week for women or >14 drinks/week for men) [7]. Estimated GFR (eGFR) was calculated according to the 2012 Chronic Kidney Diseases Epidemiology Collaboration (CKD-EPI) equation, which includes both creatinine and cystatin C, and urinary albumin concentrations [13]. Serum creatinine was measured and calibrated to isotope dilution mass spectrometry-traceable methods [13]. Cystatin C was measured by means of a particle-enhanced immunonephelometry assay (N Latex Cystatin C on a BNII nephelometer [Siemens, Munich, Germany]) [13]. Urine albumin was measured by nephelometry using a BNII ProSpec nephelometer (Siemens) and urine creatinine was measured by the rate Jaffe method using the Modular-P chemistry analyser (Roche/Hitachi, Basel, Switzerland) [13] to calculate the urinary albumin-to-creatinine ratio (ACR). High-sensitivity C-reactive protein (hsCRP) was measured by particle-enhanced immunonephelometry using the BNII nephelometer (N High Sensitivity CRP; Siemens) with interassay coefficients of variation of 2.1–5.7%.
Statistical analysis
In this secondary analysis using data collected from the REGARDS cohort, we included participants who completed the follow-up visit or computer-assisted telephone interview (n = 16,150), then excluded participants with diabetes at baseline (n = 2729) and those who were missing diabetes status at baseline (n = 521), diabetes status at follow-up (n = 1580), one of the CVH metrics (n = 3202) or data on baseline covariates (n = 360) (ESM Fig. 1). The 5663 participants excluded because of missing diabetes and covariate status had a higher percentage of African-Americans, higher BMI, higher smoking, higher blood pressure, lower education and were less physically active (all p < 0.01; ESM Table 2). Descriptive statistics were used to compare the baseline characteristics overall and by baseline glycaemic status and race (Table 1; ESM Table 3). Risk ratios (RR) for incident diabetes were calculated using modified Poisson regression adjusting for age, sex, race, education, income, alcohol use, eGFR, ACR and hsCRP.
The number of ideal CVH components and each CVH metric separately were evaluated to estimate the proportion of cases in the population that might be attributable to suboptimal levels of CVH (population-attributable risk [PAR]%). The PAR% was calculated using the formula p(RR − 1)/(1 + p[RR − 1]), where p is the prevalence of individuals not in the low-risk group and RR is the associated multivariable-adjusted relative risk of those individuals. Upper and lower 95% CIs of the PAR% were derived using this formula and the upper and lower 95% CI estimates of the multivariable-adjusted RR [14]. Given that the association of ideal CVH with diabetes risk may differ by age, sex, race, glycaemic status (normal <5.6 mmol/l vs IFG 5.6–6.9 mmol/l) and history of coronary heart disease, we tested for interaction by these factors with CVH measures by inserting an interaction term in the model and using the likelihood ratio test.
We performed sensitivity analyses (ESM Tables 4–8) to confirm the robustness of our findings. These analyses included: (1) adjusting for baseline fasting glucose in the main analysis (ESM Table 4); (2) using the World Health Organization classification of IFG (<6.1 mmol/l vs 6.1–6.9 mmol/l in stratified models (ESM Table 5); (3) examining RRs for incident dysglycaemia (IFG and diabetes combined [ESM Table 6]; IFG only [ESM Table 7]) among participants with normal fasting glucose at baseline; and (4) performing the main analysis with full adjustment except for eGFR, ACR and hsCRP, as these may be in the pathway from risk to diabetes (ESM Table 8). Statistical significance was defined as two-sided α < 0.05 for all analyses except for interactions (p < 0.10). Analyses were performed using SAS 9.4 (SAS, Cary, NC, USA).
Results
Characteristics of the cohort
Among the 7758 included participants, the 1754 with IFG had significantly higher smoking prevalence, BMI, waist circumference, BP, fasting glucose and hsCRP than the 6004 participants with normal fasting glucose. Additionally, participants with IFG had fewer ideal CVH components compared with those with normal fasting glucose (all p < 0.05; Table 1). Similar to the IFG group vs normal fasting glucose, African-American participants had a more adverse cardiometabolic profile compared with white participants (ESM Table 3).
Incidence of diabetes
During a median follow-up of 9.5 years (interquartile range [IQR] 8.6–9.9 years), there were 891 participants who developed diabetes (incidence rate 11.5 per 1000 person-years). The incidence rates were higher among participants with IFG vs normal fasting glucose (30.4 vs 6.0 per 1000 person-years) (Table 1) and among African-American vs white participants (17.3 vs 9.4 per 1000 person-years) (ESM Table 3).
Ideal CVH and incident diabetes
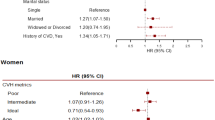
The unadjusted and adjusted RRs for incident diabetes associated with baseline ideal CVH are presented in Table 2. The RRs for 2–3 ideal CVH components or ≥4 ideal CVH components compared with 0–1 ideal CVH components were 0.70 (95% CI 0.62, 0.79) and 0.29 (95% CI 0.20, 0.41), respectively. Among the individual CVH components, ideal vs poor status was associated with a lower risk of incident diabetes for blood pressure (RR 0.39, 95% CI 0.31, 0.49), BMI (RR 0.23, 95% CI 0.18, 0.29), current smoking (RR 0.75, 95% CI 0.63, 0.89) and dietary intake (RR 0.81, 95% CI 0.68, 0.97) in adjusted analyses (Table 3).
Cardiovascular health and incident diabetes by glycaemic status
There were significant differences by glycaemic status (p for interaction <0.0001) in the association of baseline CVH components with risk of diabetes. Having ≥4 ideal CVH components vs 0–1 ideal CVH components was associated with a greater magnitude of diabetes risk-lowering in participants with normoglycaemia than in those with IFG (RR 0.20, 95% CI 0.10, 0.37 vs RR 0.87, 95% CI 0.58, 1.30; Table 2). Among the individual CVH components, there were significant differences for BMI, blood pressure, smoking and dietary intake by glycaemic status (all p < 0.05; Table 3).
Cardiovascular health and incident diabetes by race
There were significant differences by race (p for interaction = 0.0338) in the association of baseline CVH components with risk of diabetes. Participants having 2–3 and ≥4 ideal CVH components vs 0–1 ideal CVH components was associated with a greater magnitude of diabetes risk-lowering in white (39% and 73%) than in African-American (14% and 66%) participants. In Table 3, among the individual CVH components, there were significant differences for BMI and BP by race (both p < 0.05).
Age (p for interaction = 0.2385), sex (p for interaction = 0.4420) and history of coronary heart disease (p for interaction = 0.5464) did not modify the association of ideal CVH with incident diabetes. Findings were similar in sensitivity analyses: (1) adjusted for glucose in the main analysis (ESM Table 4); (2) using the World Health Organization classification of IFG <6.1 mmol/l vs 6.1–6.9 mmol/l in stratified models (ESM Table 5); (3) evaluating incident IFG and diabetes combined (ESM Table 6) and incident IFG alone at follow-up (ESM Table 7) among those with normal fasting glucose at baseline; and (4) excluding adjustment for eGFR, ACR and hsCRP from the main analysis (ESM Table 8). The exception was that there were no significant racial/ethnic differences in the association of CVH with incident IFG alone.
Population-attributable diabetes risk
We present the results of the evaluation of diabetes risk by baseline number of CVH components and categories at baseline, compared with all others not in that group in Table 4. Overall, participants with ≥4 ideal CVH components at baseline (10% of participants) had a 70% lower risk of diabetes, and 6.8 out of ten new cases of diabetes appeared attributable to not being in the ideal CVH group at baseline. Participants with normal fasting glucose in the ≥4 ideal CVH components category at baseline (12% of participants) had a 79% lower risk of diabetes and 7.6 out of ten new cases of diabetes appeared attributable to not being in the ideal CVH group at baseline; among individuals with IFG, this was only 1.9 out of ten new cases.
Discussion
In this large contemporary cohort study, a higher number of ideal CVH components at baseline showed a graded, inverse association with incident diabetes, consistent with previous studies [4, 5, 14, 15]. However, the magnitude of the association of ideal CVH with lower diabetes risk varied by glycaemic status, with a strong inverse association observed among those with normal glucose and no association observed among those with IFG. These findings suggest population-level public health promotion of the AHA 2020 ideal CVH metrics may be beneficial for primordial prevention of diabetes, but may not be as beneficial for preventing progression to diabetes from IFG over 10 years in black and white middle-aged and older adults.
Ideal CVH, baseline glycaemic status and incident diabetes
Our study is consistent with previous analyses examining the association of ideal CVH with incident diabetes, revealing a dose-dependent inverse association with incident diabetes [4, 5, 16], both continuously and categorically. These findings confirm the importance of focusing on increased attainment of ideal CVH in the USA as only 27.9% of the REGARDS participants in this analysis had ≥4 out of seven ideal CVH metrics. Among participants with IFG, the prevalence of ≥4 out of six ideal CVH metrics was low at 4.4% compared with 11.9% among those with normal fasting glucose. These differences in baseline ideal CVH for individuals with IFG are even more concerning given the lower (non-significant) magnitude of risk reduction with higher levels of ideal CVH among individuals with IFG. Previously, we evaluated modifiable lifestyle factors, including exercise, diet, cigarette smoking, television watching and sleep-disordered breathing, among African-Americans in the Jackson Heart Study and showed lower risk of incident diabetes with more ideal levels of these risk factors. However, similar to this analysis, the results were driven by individuals at the lower end of the diabetes-risk spectrum (BMI <30 kg/m2 and normoglycaemia) [6], suggesting broader public health interventions may work well for primordial prevention but not as well for those with IFG. As noted by Tuomilehto et al [17], lower-intensity population-level interventions involving multiple stakeholders are well suited for primordial prevention of diabetes, but individuals later in the natural history of glucose dysregulation with significant pathophysiological derangements (i.e. IFG [hepatic insulin resistance and decreased first-phase insulin response], impaired glucose tolerance [skeletal muscle insulin resistance and reduced early- and late-phase insulin response]) may require participation in higher intensity interventions. Interestingly, while high-intensity interventions among participants with impaired glucose tolerance, such as the diabetes prevention programme [18], have been successful in reducing the development of diabetes, high-intensity interventions in isolated IFG have not produced the same response [17, 19]. Thus, our findings support the need for further investigation of novel approaches including newer pharmacotherapies such as glucagon-like peptide-1 receptor agonists in individuals with IFG [20].
Racial differences
Consistent with prior studies [4, 21, 22], African-American participants in the REGARDS cohort had a lower prevalence of ideal CVH at baseline compared with white participants (17.2% vs 31.8%). The racial differences are concerning given that ideal CVH in African-Americans was associated with lower magnitude of diabetes risk-lowering, especially for individuals with attainment of 2–3 ideal metrics, which represented 55% of African-Americans. Notably, there were no racial differences in incident IFG (ESM Table 7). In addition to overall ideal CVH differences, ideal vs poor levels of blood pressure and BMI were associated with much lower risk among white vs African-American participants (81% vs 66%, p = 0.0309 and 69% vs 37%, p = 0.0194), respectively. Physical activity and dietary intake were associated with significantly lower risk of incident diabetes among white participants but not among African-Americans. In the Multi-Ethnic Study of Atherosclerosis [4], more ideal levels of BP were associated with lowest risk among white participants, consistent with REGARDS, but there were no racial differences for BMI. The findings for discrepancy of the association of BP with insulin resistance and incident diabetes have also been reported in prior race-stratified analyses [23, 24]. These differences may result from co-existing cardiometabolic risk factors including adiposity, fasting hyperinsulinaemia, inflammation, endothelial dysfunction and socioeconomic status. In this analysis, we adjusted for inflammation (hsCRP) and socioeconomic status and the findings persisted. Consistent with prior studies, African-Americans had higher waist circumference and fasting glucose, which may partly explain the findings for BP [25]. Investigations have also shown that hormonal actions underlying hypertension and diabetes, including aldosterone, may be different in African-American vs white participants. Aldosterone is associated with a dose-dependent higher risk of incident diabetes among African-Americans [26]. African-Americans are sensitive to the effects of aldosterone and mineralocorticoid receptor agonists, as evidenced by studies showing that aldosterone and 9-α fludrocortisone (mineralocorticoid receptor agonist) increase BP in African-American but not white participants [27]. Given the high rates of hypertension and diabetes among African-Americans, further research exploring mechanistic links explaining pathophysiological racial differences is of paramount importance. The lower magnitude of diabetes risk-lowering with ideal CVH in African-Americans provides one potential explanation for the continued rise in incident diabetes among African-Americans, which contrasts with the plateauing of risk among the white population over the last 20 years [28].
Strengths/limitations
The strengths of our analysis include a large, biracial population-based cohort with a decade of follow-up and rigorously ascertained physiological measures. We used validated questionnaires and an objective assessment of diabetes using fasting glucose and medication use. This study also has several potential limitations. Dietary data were obtained using an FFQ of usual diet over the previous year and was modified from the original definition. Additionally, we did not scale the dietary components based on total energy intake because of the difficulty in ascertaining an accurate estimate and this may have resulted in misclassification. In our study, the majority of participants (78.5%) were in the poor category for diet, which is consistent with findings reported in other studies [21]. Our study assessed the frequency of intense physical activity. Although geographic region and season may influence the intensity of physical activity required to work up a sweat, this widely used measure of physical activity is well validated [29]. We did not collect data on physical activity duration, thus our measure may over- or underestimate the actual adherence to the original definition of the AHA physical activity goal, which is based on minutes of physical activity per week. Our findings of a non-significant relationship between ideal CVH and incident diabetes in those with IFG could be due to several factors that could not be evaluated, such as genetic susceptibility and lifestyle changes after being identified as high risk for diabetes. We were unable to distinguish between type 1 diabetes and type 2 diabetes, but in this age range, incident type 1 diabetes is extremely uncommon, so we assumed a predominance of type 2 diabetes in our population.
Conclusions
Our study demonstrated that increasing levels of ideal CVH were associated with a lower risk of diabetes, especially among participants with normal fasting glucose at baseline. However, only one in four participants overall and fewer than one in 20 participants with IFG had ≥4 ideal CVH components at baseline. The lower magnitude of risk reduction with ideal CVH among those with IFG warrants further investigation and suggests this group requires higher intensity interventions to lower long-term diabetes risk. Primordial prevention through attainment of ideal CVH has the potential to dramatically reduce the burden of diabetes.
Data availability
This study uses data from the REGARDS cohort. In order to abide by its obligations with National Institutes of Health/National Institute of Neurological Disorders and Stroke and the Institutional Review Board of the University of Alabama at Birmingham, REGARDS facilitates data sharing through formal data-use agreements. Any investigator is welcome to access the REGARDS data through this process. Requests for data access may be sent to regardsadmin@uab.edu.
Abbreviations
- ACR:
-
Albumin-to-creatinine ratio
- AHA:
-
American Heart Association
- CVD:
-
Cardiovascular disease
- CVH:
-
Cardiovascular health
- CKD-EPI:
-
Chronic Kidney Diseases Epidemiology Collaboration
- eGFR:
-
Estimated GFR
- FFQ:
-
Food frequency questionnaire
- hsCRP:
-
high-sensitivity C-reactive protein
- IFG:
-
Impaired fasting glucose
- IQR:
-
Interquartile range
- PAR:
-
Population-attributable risk
- REGARDS:
-
REasons for Geographic and Racial Differences in Stroke
- RR:
-
Risk ratio
References
Lloyd-Jones DM, Hong Y, Labarthe D et al (2010) Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation 121(4):586–613. https://doi.org/10.1161/CIRCULATIONAHA.109.192703
Folsom AR, Yatsuya H, Nettleton JA et al (2011) Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol 57(16):1690–1696. https://doi.org/10.1016/j.jacc.2010.11.041
Ford ES, Greenlund KJ, Hong Y (2012) Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation 125(8):987–995. https://doi.org/10.1161/CIRCULATIONAHA.111.049122
Joseph JJ, Echouffo-Tcheugui JB, Carnethon MR et al (2016) The association of ideal cardiovascular health with incident type 2 diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis. Diabetologia 59(9):1893–1903. https://doi.org/10.1007/s00125-016-4003-7
Effoe VS, Carnethon MR, Echouffo Tcheugui JB et al (2017) The American Heart Association ideal cardiovascular health and incident type 2 diabetes mellitus among blacks: the Jackson Heart Study. J Am Heart Assoc 6(6):e005008. https://doi.org/10.1161/JAHA.116.005008
Joseph JJ, Echouffo-Tcheugui JB, Talegawkar SA et al (2017) Modifiable lifestyle risk factors and incident diabetes in African Americans. Am J Prev Med 53(5):e165–e174. https://doi.org/10.1016/j.amepre.2017.06.018
Howard VJ, Cushman M, Pulley L et al (2005) The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology 25(3):135–143. https://doi.org/10.1159/000086678
Cushman M, Cantrell RA, McClure LA et al (2008) Estimated 10-year stroke risk by region and race in the United States. Ann Neurol 64(5):507–513. https://doi.org/10.1002/ana.21493
Block G, Woods M, Potosky A, Clifford C (1990) Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol 43(12):1327–1335. https://doi.org/10.1016/0895-4356(90)90099-B
Judd SE, Letter AJ, Shikany JM et al (2015) Dietary patterns derived using exploratory and confirmatory factor analysis are stable and generalizable across race, region, and gender subgroups in the REGARDS Study. Front Nutr 1:29. https://doi.org/10.3389/fnut.2014.00029
Kulshreshtha A, Vaccarino V, Judd SE et al (2013) Life’s simple 7 and risk of incident stroke the reasons for geographic and racial differences in stroke study. Stroke 44(7):1909–1914. https://doi.org/10.1161/STROKEAHA.111.000352
Gillett SR, Boyle RH, Zakai NA et al (2014) Validating laboratory results in a national observational cohort study without field centers: the Reasons for Geographic and Racial Differences in Stroke cohort. Clin Biochem 47(16-17):243–246. https://doi.org/10.1016/j.clinbiochem.2014.08.003
Peralta CA (2011) Detection of chronic kidney disease with creatinine, cystatin C, and urine albumin-to-creatinine ratio and association with progression to end-stage renal disease and mortality. JAMA 305(15):1545–1552. https://doi.org/10.1001/jama.2011.468
Mozaffarian D, Kamineni A, Carnethon M et al (2009) Lifestyle risk factors and new-onset diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med 169(8):798–807. https://doi.org/10.1001/archinternmed.2009.21
Reis JP, Loria CM, Sorlie PD, Park Y, Hollenbeck A, Schatzkin A (2011) Lifestyle factors and risk for new-onset diabetes: a population-based cohort study. Ann Intern Med 155(5):292–299. https://doi.org/10.7326/0003-4819-155-5-201109060-00006
Fretts AM, Howard BV, McKnight B et al (2014) Life’s simple 7 and incidence of diabetes among American Indians: the Strong Heart Family Study. Diabetes Care 37(8):2240–2245. https://doi.org/10.2337/dc13-2267
Tuomilehto J, Schwarz PEH (2016) Preventing diabetes: early versus late preventive interventions: table 1. Diabetes Care 39(Suppl 2):S115–S120. https://doi.org/10.2337/dcS15-3000
The Diabetes Prevention Program (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346(6):393–403. https://doi.org/10.1056/NEJMoa012512
Saito T, Watanabe M, Nishida J et al (2011) Lifestyle modification and prevention of type 2 diabetes in overweight Japanese with impaired fasting glucose levels: a randomized controlled trial. Arch Intern Med 171(15):1352–1360. https://doi.org/10.1001/archinternmed.2011.275
le Roux CW, Astrup A, Fujioka K et al (2017) 3 years of liraglutide versus placebo for type 2 diabetes risk reduction and weight management in individuals with prediabetes: a randomised, double-blind trial. Lancet 389(10077):1399–1409. https://doi.org/10.1016/S0140-6736(17)30069-7
Shay CM, Ning H, Allen NB et al (2012) Status of cardiovascular health in US adults prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation 125(1):45–56. https://doi.org/10.1161/CIRCULATIONAHA.111.035733
Mujahid MS, Moore LV, Petito LC et al (2017) Neighborhoods and racial/ethnic differences in ideal cardiovascular health (the Multi-Ethnic Study of Atherosclerosis). Health Place 44:61–69. https://doi.org/10.1016/j.healthplace.2017.01.005
Saad MF, Lillioja S, Nyomba BL et al (1991) Racial differences in the relation between blood pressure and insulin resistance. N Engl J Med 324(11):733–739. https://doi.org/10.1056/NEJM199103143241105
Wei GS, Coady SA, Goff DC et al (2011) Blood pressure and the risk of developing diabetes in African Americans and whites: ARIC, CARDIA, and the Framingham Heart Study. Diabetes Care 34(4):873–879. https://doi.org/10.2337/dc10-1786
Zhang T, Zhang H, Li S et al (2016) Impact of adiposity on incident hypertension is modified by insulin resistance in AdultsNovelty and significance: longitudinal observation from the Bogalusa Heart Study. Hypertension 67(1):56–62. https://doi.org/10.1161/HYPERTENSIONAHA.115.06509
Joseph JJ, Echouffo-Tcheugui JB, Kalyani RR et al (2016) Aldosterone, renin, and diabetes mellitus in African Americans: the Jackson Heart Study. J Clin Endocrinol Metab 101(4):1770–1778. https://doi.org/10.1210/jc.2016-1002
Tu W, Eckert GJ, Hannon TS et al (2014) Racial differences in sensitivity of blood pressure to aldosterone. Hypertension 63(6):1212–1218. https://doi.org/10.1161/HYPERTENSIONAHA.113.02989
Geiss LS, Wang J, Cheng YJ et al (2014) Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980-2012. JAMA 312(12):1218. https://doi.org/10.1001/jama.2014.11494
McDonnell MN, Hillier SL, Hooker SP et al (2013) Physical activity frequency and risk of incident stroke in a national US study of blacks and whites. Stroke 44(9):2519–2524. https://doi.org/10.1161/STROKEAHA.113.001538
Acknowledgements
The authors thank the other investigators, the staff and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at www.regardsstudy.org.
Parts of this study were presented as an oral presentation at the AHA EPI/LIFESTYLE 2018 Scientific Sessions, New Orleans, LA, USA 20–23 March 2018.
Contribution statement
JJJ researched data, performed data interpretation and wrote the manuscript. AB performed data analysis and contributed to data interpretation, methods and revision of the manuscript. JBET, VSE, JBO, BH, AD, MMS, DMC, MC and APC contributed to methods, data interpretation and reviewed/edited the manuscript. JJJ is the guarantor of this work and, as such, had full access to all the data and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors gave final approval of the version to be published.
Funding
This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health and the Department of Health and Human Service. Additional support was provided by U01DP006302 from the Centers for Disease Control and Prevention and K23DK117041 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Centers for Disease Control and Prevention, the National Institute of Neurological Disorders and Stroke, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institutes of Health or the Department of Health and Human Services.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
JJJ and MC are members of the American Heart Association/American Stroke Association 2020 Goal Metrics Committee. APC and MMS report receiving research support from Amgen that is unrelated to the current work. All other authors declare that there is no duality of interest associated with their contribution to this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM
(PDF 179 kb)
Rights and permissions
About this article
Cite this article
Joseph, J.J., Bennett, A., Echouffo Tcheugui, J.B. et al. Ideal cardiovascular health, glycaemic status and incident type 2 diabetes mellitus: the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Diabetologia 62, 426–437 (2019). https://doi.org/10.1007/s00125-018-4792-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4792-y