Abstract
Aims/hypothesis
We examined whether measures of glycaemic variability (GV), assessed by continuous glucose monitoring (CGM) and self-monitoring of blood glucose (SMBG), can complement or replace measures of beta cell function and insulin action in detecting the progression of preclinical disease to type 1 diabetes.
Methods
Twenty-two autoantibody-positive (autoAb+) first-degree relatives (FDRs) of patients with type 1 diabetes who were themselves at high 5-year risk (50%) for type 1 diabetes underwent CGM, a hyperglycaemic clamp test and OGTT, and were followed for up to 31 months. Clamp variables were used to estimate beta cell function (first-phase [AUC5–10 min] and second-phase [AUC120–150 min] C-peptide release) combined with insulin resistance (glucose disposal rate; M 120–150 min). Age-matched healthy volunteers (n = 20) and individuals with recent-onset type 1 diabetes (n = 9) served as control groups.
Results
In autoAb+ FDRs, M 120–150 min below the 10th percentile (P10) of controls achieved 86% diagnostic efficiency in discriminating between normoglycaemic FDRs and individuals with (impending) dysglycaemia. M 120–150 min outperformed AUC5–10 min and AUC120–150 min C-peptide below P10 of controls, which were only 59–68% effective. Among GV variables, CGM above the reference range was better at detecting (impending) dysglycaemia than elevated SMBG (77–82% vs 73% efficiency). Combined CGM measures were equally efficient as M 120–150 min (86%). Daytime GV variables were inversely correlated with clamp variables, and more strongly with M 120–150 min than with AUC5–10 min or AUC120–150 min C-peptide.
Conclusions/interpretation
CGM-derived GV and the glucose disposal rate, reflecting both insulin secretion and action, outperformed SMBG and first- or second-phase AUC C-peptide in identifying FDRs with (impending) dysglycaemia or diabetes. Our results indicate the feasibility of developing minimally invasive CGM-based criteria for close metabolic monitoring and as outcome measures in trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prompt detection of type 1 diabetes enables patients to avoid diabetic ketoacidosis and start insulin treatment early in order to maximise beta cell preservation and minimise the risk of complications [1–3]. Moreover, secondary and tertiary prevention trials with immune interventions require the identification of individuals with impending or asymptomatic clinical onset of diabetes and relatively preserved beta cell function [4–6]. Virtually all first-degree relatives (FDRs) of patients with type 1 diabetes who have positivity for at least two diabetes-associated autoantibodies will develop diabetes within 20 years [7]. Those with dysglycaemia or low stimulated C-peptide release are likely to develop the disease rapidly (i.e. within 3 years) [8–12]. This subgroup can be detected by repetitive hyperglycaemic clamps or OGTTs, but these are not simple procedures to implement, especially in children [13, 14]. Moreover, OGTT data are subject to large inter- and intra-individual variability [13]. Elevated HbA1c is a stable and specific indicator of impending diabetes, but occurs at a later phase of the disease and is therefore an insensitive detector [15, 16].
We hypothesised that glycaemic variability (GV), as measured by continuous glucose monitoring (CGM), can provide early and easily accessible detection of reduced beta cell function and impending type 1 diabetes in at-risk groups. An inverse relationship between crude measures of GV (as determined by self-monitoring of blood glucose [SMBG]) and residual beta cell function (as assessed by the hyperglycaemic clamp) has previously been demonstrated in islet graft recipients [17]. Here, we investigated this correlation in earlier disease phases (i.e. before and at clinical onset) [18].
We evaluated GV by CGM and SMBG in parallel with measurements of first- and second-phase C-peptide release, the glucose disposal rate and the insulin-sensitivity index (ISI) derived from hyperglycaemic clamps [10], the gold standard for assessing beta cell function [19, 20]. We examined whether GV above the range of healthy controls predicts the development of dysglycaemia or diabetes in autoantibody-positive (autoAb+) FDRs of patients with type 1 diabetes and how this correlates with clamp-derived variables. This analysis could indicate whether minimally invasive CGM- or SMBG-derived data might serve as markers for the early diagnosis of type 1 diabetes, and as surrogate endpoints in prevention and curative trials.
Methods
Participants
Informed consent was obtained from each participant, and also from their parents in the case of minors. The study protocol was approved by the ethics committees of the Belgian Diabetes Registry and the participating university hospitals, and was conducted in accordance with the Declaration of Helsinki as revised in 2013.
High-risk FDRs
A total of 22 FDRs of patients with type 1 diabetes (12 siblings, nine offspring, one parent) were recruited by the Belgian Diabetes Registry and underwent an OGTT, followed by CGM for 5 days and finally a hyperglycaemic clamp test. All of the participants were positive for autoantibodies against insulinoma-associated protein 2 [IA-2A] or zinc transporter 8 [ZnT8A] and at least one other diabetes autoantibody, a profile that has previously been shown to confer about a 50% risk of developing diabetes within 5 years [18]. Seven FDRs carried the high-risk HLA-DQ2/DQ8 genotype (Table 1).
The participants were followed (median [range]: 18 [3–31] months) for glucose tolerance and diabetes onset (OGTT), GV (CGM and seven-point profile with SMBG) and beta cell function (hyperglycaemic clamp) every 6 months. Impaired fasting glucose, impaired glucose tolerance (IGT) and diabetes were defined according to ADA criteria [21]. At diagnosis, FDRs were shifted to intensive insulin treatment and excluded from the study.
Patients with type 1 diabetes
Six patients with recent-onset diabetes and fewer than 4 weeks of intensive insulin treatment and three patients in clinical remission (<0.5 U/kg/day insulin and HbA1c <7% [<53 mmol/mol]; 5–15 months after diagnosis) [22] were recruited. These participants underwent a hyperglycaemic clamp, followed by 5 days of CGM.
Healthy volunteers
CGM measurements were taken and hyperglycaemic clamps were performed in 20 healthy volunteers. None of these participants had a family history of type 1 diabetes or an FDR with type 2 diabetes. All tested negative for diabetes-associated autoantibodies (islet-cell cytoplasm autoantibodies, glutamate decarboxylase autoantibodies, IA-2A, insulin autoantibodies and ZnT8A) [18] and all had a normal OGTT (Table 1).
OGTTs
Blood samples were collected for glucose analysis before and 2 h after an oral glucose load of 1.75 g/kg without exceeding the maximum of 75 g [8].
Hyperglycaemic clamps
A hyperglycaemic clamp was performed 1–2 weeks after the OGTT, as previously described, with the omission of a glucagon injection at 150 min [8, 19]. In patients treated with long-acting insulin, this insulin type was replaced by an intermediately acting insulin on the evening before the clamp.
Briefly, after an overnight fast, a 20% glucose solution (Baxter, Brussels, Belgium) was infused via the left antecubital vein at time 0. During the first 14 min, a priming glucose dose was administered and the blood glucose level was raised to reach the plateau of 10 mmol/l. Thereafter, this hyperglycaemic target was maintained by adjusting the glucose infusion rate upon assessment of bedside blood glucose levels every 5 min using the Accu-Chek Inform II glucose monitor (Roche Diagnostics, Mannheim, Germany) calibrated as plasma glucose.
Blood samples for C-peptide and proinsulin determination were collected at 5, 7.5 and 10 min to derive the first-phase C-peptide release (AUC5–10 min C-peptide), and at 120, 135 and 150 min for the second-phase release (AUC120–150 min C-peptide). AUC C-peptide release was calculated using the trapezoidal rule and expressed per minute [8]. The glucose disposal rate between 120 and 150 min (M 120–150 min, expressed as μmol/[kg × min]) corresponds to the amount of glucose metabolised during hyperglycaemia and was calculated as the average glucose infusion rate between 120 and 150 min minus a ‘space correction’ [19]. The ISI (ISI120–150 min) was calculated by dividing M 120–150 min (expressed as mmol/[kg × min]) by the average insulin concentrations (expressed as pmol/l) during the same period, multiplied by 100. The disposition index was computed by multiplying AUC120–150 min C-peptide with the HOMA2-IR [23]. Percentile 10 (P10) of the healthy control group (n = 20) was used to indicate low AUC5–10 min C-peptide, AUC120–150 min C-peptide and M 120–150 min. No development of diabetes was reported in this reference population.
GV
An iPro2 CGM device (Medtronic, Northridge, CA, USA) was inserted following the OGTT (FDRs and volunteers) or hyperglycaemic clamp (patients). The median blinded CGM time was 120 h per participant, with a minimum of 96 h. During this period, participants performed a seven-point SMBG profile (preprandial, 2 h postprandial and pre-bedtime) using a Contour Link glucometer (Bayer, Leverkusen, Germany). The three preprandial and the pre-bedtime glucose values were used to calibrate each 24 h period. Participants were also asked to complete a simple log of their dietary intake, drug intake, activity, and sleep and wake times. Healthy volunteers (n = 20), autoAb+ FDRs (n = 22) and patients with type 1 diabetes (n = 9) did not differ in the percentages of missing CGM data (<6%). This study presents the baseline CGM and SMBG data; the collection of longitudinal data is ongoing.
Analytical methods
Plasma glucose was assessed using a glucose oxidase method (Vitros 5.1FS, Ortho Clinical Diagnostics, Rochester, NY, USA); C-peptide and insulin by electrochemiluminescence immunoassay (Cobas e411, Elecsys, Basel, Switzerland); proinsulin by time-resolved fluorescence immunoassay (AutoDELFIA, Perkin-Elmer, Waltham, MA, USA) [24]; and HbA1c by HPLC (HLC-723G7, Tosoh Bioscience, Tessenderlo, Belgium). Because of the 100% cross-reactivity of proinsulin in the C-peptide assay, free C-peptide levels were obtained by subtracting the proinsulin concentration from the total C-peptide result [8]. Diabetes autoantibodies (insulin autoantibodies, glutamate decarboxylase autoantibodies, IA-2A and ZnT8A) were determined by liquid-phase radiobinding assays and HLA-DQ polymorphisms by allele-specific oligonucleotide genotyping, as previously described [18].
Data analysis and statistical analysis
All GV variables are shown in the electronic supplementary material (ESM) Methods. SMBG-derived variables were obtained from at least five fingerstick measurements (two preprandial, two postprandial and one pre-bedtime) per 24 h for a minimum of 4 days. CGM-derived variables were calculated using the GlyVarT program, version 1.0 (Medtronic Bakken Research Center, Maastricht, the Netherlands). GV indices did not include the initial 2 h of monitoring, as this is an unstable calibration period. Daytime CGM measurements were calculated between awakening and bedtime (and night-time measurements between bedtime and awakening), as documented in the participants’ logbooks. Data from a given day were excluded if more than 20% of CGM data were missing or if fewer than three valid calibration values per 24 h period were available [14]. GV measures were considered to be elevated if they exceeded the maximum value found in healthy controls (n = 20). Fasting C-peptide and glucose values before the start of the hyperglycaemic clamp were used to determine HOMA2-IR using the calculator available at www.OCDEM.ox.ac.uk [25].
Statistical analyses were performed two-tailed using SPSS version 22.0 for Windows (IBM SPSS Statistics, Chicago, IL, USA); figures were generated using GraphPad Prism version 5.00 for Windows (GraphPad, San Diego, CA, USA); and differences between groups were assessed using the Mann–Whitney U or Kruskal–Wallis tests for continuous variables, and by the χ 2 or Fisher’s exact tests for categorical variables. p < 0.05 or p < 0.05/k in the case of k comparisons was considered statistically significant. Correlations between variables were assessed using the Spearman rank test. Curve fitting was performed in GraphPad Prism version 5.00 according to the least-square ordinary fitting method. The extra sum-of-squares F test was used to compare fitting models. The more complicated model (H1; e.g. two-phase model) was chosen over the simpler model (H0; e.g. one-phase model) if p < 0.05.
Results
Characteristics of the study groups
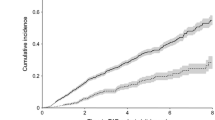
The healthy volunteer (n = 20), autoAb+ FDR (n = 22) and type 1 diabetes (n = 9) groups did not significantly differ in age, the ratio of males to females or BMI z score (Table 1). All FDRs and eight out of nine patients with type 1 diabetes were IA-2A or ZnT8A positive and carried at least one additional autoantibody among the four specificities tested. Healthy controls and FDRs did not differ in their HbA1c levels at baseline, with all values being below 6.0% (42 mmol/mol). Five of the 22 FDRs had IGT at baseline, with one of these participants also having impaired fasting glucose. Two of these five participants developed diabetes within 20 months, while the other three remained glucose intolerant during follow-up (4–19 months). Of the 17 initially normoglycaemic FDRs, two developed IGT after 10–12 months and three developed diabetes after 4–14 months (Table 1, Fig. 1).
Baseline hyperglycaemic clamp-derived and GV variables of study groups according to outcome
Figure 2 shows the average CGM profiles in healthy volunteers (n = 20; Fig. 2a), FDRs with persistent euglycaemia (n = 12; Fig. 2b), FDRs with euglycaemia at baseline but who became glucose intolerant or developed diabetes during follow-up (n = 5; Fig. 2c), FDRs with dysglycaemia at baseline (n = 5; Fig. 2d), patients with type 1 diabetes in remission (n = 3; Fig. 2e) and patients with recent-onset type 1 diabetes (n = 6; Fig. 2f). From the CGM and SMBG measurements, we derived 201 GV variables (ESM Methods). Among these variables, we first investigated how simple baseline measures of GV during daytime (CGM-derived % CVday and % timeday >7.8 mmol/l glucose; SMBG-derived SDday) were able to discriminate between the six above-mentioned groups of participants in comparison with hyperglycaemic clamp-derived variables of insulin secretion and action (Fig. 3).
Average CGM profiles of the different study groups. Each curve represents the average CGM profile over 4–5 days for one participant. (a) Healthy volunteers (n = 20); (b) autoAb+ FDRs with persistent euglycaemia (n = 12); (c) autoAb+ FDRs with euglycaemia at baseline and dysglycaemia during follow-up (n = 5); (d) FDRs with dysglycaemia at baseline (n = 5); (e) patients with type 1 diabetes in remission (n = 3); (f) patients with recent-onset type 1 diabetes (n = 6). Broken lines indicate the glycaemia range between 3.9 and 7.8 mmol/l [21]
Baseline hyperglycaemic clamp-derived and GV variables of the study groups. (a) First-phase AUC C-peptide release (AUC5–10 min); (b) second-phase AUC C-peptide release (AUC120–150 min); (c) glucose disposal rate (M 120–150 min); (d) glucose CVday measured by CGM; (e) glucose SDday measured by SMBG; (f) % timeday >7.8 mmol/l measured by CGM. Data are dot plots with indications of median values and IQR. *p < 0.05, **p < 0.01, ***p < 0.001. In each panel, the overall significance was p < 0.001 (the threshold for significance was p < 0.05/k: p < 0.05/6 or p < 0.008). The threshold for significance of comparisons within each panel was p < 0.05/10 or p < 0.005
Persistently euglycaemic autoAb+ FDRs (n = 12) did not differ from healthy controls for these variables (Fig. 3b,c), except for a trend (p = 0.009; threshold p < 0.005; Bonferroni correction) towards a lower first-phase C-peptide release (Fig. 3a; ESM Fig. 1). FDRs who developed IGT or diabetes during follow-up (n = 5) had lower first- and second-phase C-peptide release, and a lower glucose disposal rate (M 120–150 min) during the hyperglycaemic clamp, compared with healthy controls (p = 0.006 to p < 0.001; Fig. 3a–c); they also tended to have lower clamp-derived values and higher GV variables than FDRs who remained euglycaemic (Fig. 3a–f).
M 120–150 min best discriminated between persistently normoglycaemic FDRs and FDRs with dysglycaemia at baseline (p < 0.001; Fig. 3a–f). Overall, FDRs who developed diabetes did not differ from those who remained glucose intolerant (data not shown). Patients with recent-onset diabetes had no measurable AUC5–10 min C-peptide (Fig. 3a); all clamp-derived variables (p = 0.009 to p < 0.001) and some GV measures tended to differ from those of dysglycaemic autoAb+ FDRs (Fig. 3b–f). Patients with type 1 diabetes in remission tended to have GV values more similar to those of dysglycaemic FDRs than of patients with recent-onset diabetes (no statistical test performed because of low numbers) (Fig. 3d–f). Other clamp-derived measures (e.g. ISI120–150 min; disposition index) [8], HOMA2-IR and more sophisticated CGM variables (e.g. continuous overall net glycaemic action [CONGA]) [26] performed less well in discriminating between the various groups (data not shown).
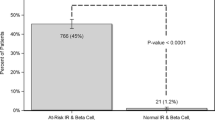
Diagnostic performance of hyperglycaemic clamp-derived variables and measures of GV to detect or predict dysglycaemia
Of the ten autoAb+ FDRs who had (n = 5) or developed (n = 5) dysglycaemia, seven had a low first-phase C-peptide release, five a low second-phase release and seven a low glucose disposal rate (M 120–150 min) when taking P10 of the healthy volunteers (n = 20) as the cut-off. Only four FDRs had HbA1c levels ≥5.7% (39 mmol/mol). Because of its higher diagnostic specificity, M 120–150 min achieved 86% diagnostic efficiency, thereby tending to outperform AUC C-peptide.
CGM measurements (SDday, interquartile range [IQR]day and CVday) above the range of those from healthy controls tended to achieve a higher diagnostic efficiency for detecting or predicting dysglycaemia than elevated SMBG variables (rangeday and SDday) (77–82% vs 73%). Especially when considering multiple variables (e.g. elevated SDday and/or IQRday), CGM achieved a diagnostic efficiency similar to that of M 120–150 min (86%) and higher than that of SMBG (73%) (Table 2).
Correlation of GV with beta cell function and glucose disposal rate
Among the 201 GV variables (ESM Methods), 31% were significantly and inversely correlated with beta cell function (AUC120–150 min C-peptide) and with glucose disposal rate during this phase (M 120–150 min) when considering all groups of participants together. ESM Table 1 shows the Spearman rank correlation coefficients and p values for the variables with r ≥ |0.700| for at least one of the two correlations. Overall, GV variables were more strongly correlated (higher |r| values and all p < 0.001) with clamp-derived M 120–150 min than with AUC120–150 min (p = 0.017 to p < 0.001) (ESM Table 1) or AUC5–10 min (data not shown). Some 24 h CGM variables, but none of the night-time indices, showed significant inverse correlations with AUC120–150 min and M 120–150 min (ESM Table 1). Good correlations were observed for postprandial variables, but these proved less practical because they required food intake to be logged and were more sensitive to interindividual variations.
The strongest correlations with clamp-derived variables were obtained for daytime GV measures derived from CGM (glucose CVday; Fig. 4a–c) or SMBG (glucose SDday; Fig. 4d–f). In addition, GV here was more closely related to M 120–150 min than to first- or second-phase C-peptide release. To allow comparison with data from Steck et al [14], we included correlations for CGM-derived % timeday >7.8 mmol/l (Fig. 4g–i). The best curve-fitting model was a hyperbolic function (Fig. 4). For all patients (recent-onset type 1 diabetes: n = 6; type 1 diabetes in remission: n = 3), AUC5–10 min, AUC120–150 min and M 120–150 min were below the P10 of healthy controls (Fig. 4), while CGM-derived glucose CVday (Fig. 4a–c) and % timeday >7.8 mmol/l glucose (Fig. 4g–i) exceeded the range of controls. For SMBG-derived glucose SDday, this was only the case in seven out of nine patients (Fig. 4d–f). Most autoAb+ FDRs had clamp-derived values below the P50 of controls, and most of those with (impending) dysglycaemia scored below the P10 (Fig. 4a–i). Of note, two FDRs with persistent dysglycaemia and disproportionally high beta cell function, as judged from AUC120–150 min C-peptide values (>P75), had high HOMA2-IR values (1.90 and 2.10, respectively) and high BMI z scores (2.06 and 2.18, respectively), yet low M 120–150 min (<P10) and elevated or borderline GV variables.
Correlations between GV measures and clamp-derived variables. CGM glucose CVday vs (a) AUC5–10 min C-peptide release (r s = −0.581; p < 0.001), (b) AUC120–150 min C-peptide release (r s = −0.632; p < 0.001) and (c) M 120–150 min (r s = −0.767; p < 0.001). SMBG glucose SDday vs (d) AUC5–10 min C-peptide release (r s = −0.775; p < 0.005), (e) AUC120–150 min C-peptide release (r s = −0.631; p < 0.001) and (f) M 120–150 min (r s = −0.852; p < 0.001). CGM % timeday >7.8 mmol/l vs (g) AUC5–10 min C-peptide release (r s = −0.637; p < 0.05), (h) AUC120–150 min C-peptide release (r s = −0.481; p < 0.01) and (i) M 120–150 min (r s = −0.807; p < 0.001). Red filled circles, patients with recent-onset diabetes (n = 6); red open circles, patients with diabetes in remission (n = 3); orange filled circles, FDRs with dysglycaemia at baseline (n = 5); orange open circles, FDRs with euglycaemia at baseline and dysglycaemia during follow-up (n = 5); blue filled circles, FDRs with persistent euglycaemia (n = 12). In each panel, vertical lines represent, from left to right, the P10, P25 and P50 of healthy controls (n = 20). Horizontal dashed lines represent the cut-off values for GV variables, determined as the maximum value in healthy volunteers (n = 20): glucose CVday, 16% (a–c), glucose SDday, 1.06 mmol/l (d–f) and % timeday >7.8 mmol/l, 2% (g–i). r s = Spearman rank correlation coefficient
M 120–150 min correlated better with AUC120–150 min (p < 0.001) than with AUC5–10 min (p < 0.05; Fig. 5a,b). Unlike AUC C-peptide (data not shown), M 120–150 min was significantly and inversely correlated with HOMA2-IR (r = −0.530, p = 0.007) (Fig. 5c); however, neither AUC C-peptide (data not shown) nor M 120–150 min were significantly correlated with ISI120–150 min (Fig. 5d) or with the disposition index (data not shown). Consistent with this, the GV variables analysed in Figs 3 and 4 were significantly correlated with HOMA2-IR (r = 0.505–0.740, p < 0.005–0.001), but not with ISI120–150 min or with the disposition index (data not shown).
Correlation of M 120–150 min with (a) AUC5–10 min C-peptide release (r p = 0.436; p < 0.05), (b) AUC120–150 min C-peptide release (r p = 0.622; p < 0.001), (c) HOMA2-IR (r s = −0.530; p < 0.01) and (d) ISI120–150 min (r p = 0.233; NS). Red filled circles, patients with recent-onset diabetes (n = 6); red open circles, patients with diabetes in remission (n = 3); orange filled circles, FDRs with dysglycaemia at baseline (n = 5); orange open circles, FDRs with euglycaemia at baseline and dysglycaemia during follow-up (n = 5); blue filled circles, FDRs with persistent euglycaemia (n = 12). r s , Spearman rank correlation coefficient; r p , Pearson’s correlation coefficient
Discussion
This study assessed the relationship between GV variables, clinical outcomes and residual beta cell function in combination with insulin action in an early phase of type 1 diabetes. It was conducted with the long-term perspective of identifying minimally invasive criteria for the impending clinical onset of disease and treatment goals for novel beta cell therapies. Comparison with healthy, normoglycaemic controls allowed the establishment of tentative cut-off values for the biomarkers tested.
GV variables were measured under real-life conditions (i.e. without dietary restrictions or compulsory meal times). Their use in predicting diabetes will, however, require studies of larger cohorts for longer periods of time in order to establish robust and harmonised cut-off values. The observed normal ranges for various CGM variables were in line with some previous studies [27–29], but lower than in others [14, 30, 31]. Apart from the limited number of participants in most studies, including the current study, these discrepancies might relate to differences in measuring devices, age ranges, ethnicities, dietary restrictions, risk levels for diabetes or criteria to ascertain normoglycaemia.
Our study provides the first demonstration that GV variables are equally as effective as a hyperglycaemic clamp, the gold standard for assessing beta cell function [19, 20], in discriminating normoglycaemic autoAb+ FDRs from FDRs with (impending) dysglycaemia or diabetes. In this respect, a combination of CGM-derived indices was equally efficient as the glucose disposal rate (M 120–150 min) and better than AUC5–10 min or AUC120–150 min C-peptide, or a combination of SMBG-derived variables.
Our study also provides the first demonstration of a correlation in (pre)type 1 diabetes between CGM data and clamp-derived variables. This correlation is present for different stages of glucose tolerance, ranging from healthy controls to normoglycaemic and dysglycaemic risk groups and patients with recent-onset diabetes. Overall, a significant inverse and hyperbolic relationship was documented between GV variables, as assessed by CGM or SMBG, and measures of beta cell function and/or insulin sensitivity, as assessed by the hyperglycaemic clamp. GV variables demonstrated better correlation with M 120–150 min, reflecting both insulin secretion and action [19, 20], than with first- or second-phase hormone discharge, and thus performed better in discriminating FDRs who were or who became glucose intolerant, or who developed diabetes within 20 months, from those who remained normoglycaemic.
We have previously validated the hyperglycaemic clamp for the accurate and precise determination of beta cell function in (pre)type 1 diabetes, which has proven useful as an inclusion criterion and outcome measure in beta cell therapy trials [4, 8, 9, 17]. Although the hyperinsulinaemic–euglycaemic clamp is the gold standard for determining insulin sensitivity [20], the hyperglycaemic clamp has also been validated for this purpose [32–35]. This therefore allows measurements of beta cell function relative to insulin sensitivity without the need to perform two clamp tests, which is undesirable because of an excessive burden on the patient, lack of participant or parent acceptability and inflated research costs [30]. We did not correct M 120–150 min for urinary glucose loss as it was assumed to be negligible for glycaemia clamped at 10 mmol/l [19, 33–35]. Likewise, we assumed that endogenous hepatic glucose production would be suppressed by high glucose levels during the procedure, but did not quantify this by administrating tritiated glucose [19]. Despite these limitations, M 120–150 min proved to be the best clamp-derived marker of (impending) glucose intolerance.
We recently observed that AUC C-peptide release during the hyperglycaemic clamp outperformed OGTT-derived variables in predicting diabetes within 3 years in autoAb+ FDRs [8, 9]. Consistent with this, AUC5–10 min best distinguished healthy controls from autoAb+ FDRs [9], but clamp-derived M 120–150 min was more informative than AUC120–150 min C-peptide release with respect to the short-term metabolic outcomes of individuals at high autoantibody-inferred risk: this is supported by the better correlation of M 120–150 min with GV variables and with the presence or development of dysglycaemia or diabetes within 20 months.
Glucose disposal and tolerance are determined not only by insulin secretion, but also by insulin action [36]. Consistent with this, M 120–150 min was significantly correlated with HOMA2-IR and AUC C-peptide. Our results are in line with observations that the ratio of HOMA-IR to first-phase insulin release during the IVGTT test better predicted type 1 diabetes than first-phase insulin release alone, particularly in individuals with already-compromised insulin release [37–40], and with the strong inverse correlation between oral disposition index and GV variables in individuals at different stages of glucose tolerance, ranging from normoglycaemia to overt type 2 diabetes [41]. Indeed, while in our study euglycaemic FDRs and healthy controls tended to differ only in AUC5–10 min, M 120–150 min was the best discriminator between FDRs with or without (impending) dysglycaemia.
The fact that a combination of CGM variables was strongly correlated with M120–150 min and equally effective in predicting dysglycaemia or diabetes indicates their potential significance for defining selection criteria or intermediate therapeutic endpoints in secondary prevention trials [5, 42]. This is consistent with observations in recipients of beta cell allografts, where a relationship was seen between clamp-derived variables and a simple measure of GV—the per cent CV of fasting glucose—making the latter a clinically relevant read-out [17]. In our group of participants with (pre)type 1 diabetes, such correlations could be demonstrated for several simple measures of GV obtained with CGM or even SMBG, such as SDday, % CVday or % timeday >7.8 mmol/l glucose. These variables have also the advantage of being easily understood by patients or their relatives [26]. CGM recordings seem preferable to SMBG measurements because they register all variability [26], as illustrated by the fact that combining different variables improved the efficiency of recognising dysglycaemia with CGM, but not with SMBG.
In conclusion, a decreased glucose disposal rate and simple measures of increased GV are closely associated with impending type 1 diabetes. Our results illustrate the feasibility of using these variables to develop entry criteria and therapeutic endpoints in secondary prevention trials. Larger prospective studies will be needed in order to achieve this.
Abbreviations
- autoAb+ :
-
Autoantibody-positive
- CGM:
-
Continuous glucose monitoring
- FDR:
-
First-degree relative
- GV:
-
Glycaemic variability
- IA-2A:
-
Insulinoma-associated protein 2 autoantibodies
- IGT:
-
Impaired glucose tolerance
- ISI:
-
Insulin-sensitivity index
- IQR:
-
Interquartile range
- P10:
-
Percentile 10
- SMBG:
-
Self-monitoring of blood glucose
- ZnT8A:
-
Zinc transporter 8 autoantibodies
References
Elding Larsson H, Vehik K, Bell R et al (2011) Reduced prevalence of diabetic ketoacidosis at diagnosis of type 1 diabetic in young children participating in longitudinal follow-up. Diabetes Care 34:2347–2352
Winkler C, Schober E, Ziegler AG, Holl RW (2012) Markedly reduced rate of diabetic ketoacidosis at onset of type 1 diabetes in relatives screened for islet autoantibodies. Pediatr Diabetes 13:308–313
Steffes MW, Sibley S, Jackson M (2003) Beta-cell function and the development of diabetes-related complications in the diabetes control and complications trial. Diabetes Care 26:832–836
Keymeulen B, Vandemeulebroucke E, Ziegler AG et al (2005) Insulin needs after CD3-antibody therapy in new-onset type 1 diabetes. N Engl J Med 352:2598–2608
Gorus FK, Keymeulen B, In’t Veld PA, Pipeleers DG (2013) Predictors of progression to type 1 diabetes: preparing for immune interventions in the preclinical disease phase. Expert Rev Clin Immunol 9:1173–1183
Skyler JS, Ricordi C (2011) Stopping type 1 diabetes: attempts to prevent or cure type 1 diabetes in man. Diabetes 60:1–8
Ziegler AG, Rewers M, Simell O et al (2013) Seroconversion to multiple islet autoantibodies and risk of progression to diabetes in children. JAMA 309:2473–2479
Vandemeulebroucke E, Keymeulen B, Decochez K et al (2010) Hyperglycaemic clamp test for diabetes risk assessment in IA-2-antibody-positive relatives of type 1 diabetic patients. Diabetologia 53:36–44
Balti EV, Vandemeulebroucke E, Weets I et al (2015) Hyperglycaemic clamp and oral glucose tolerance test for 3-year prediction of clinical onset in persistently autoantibody-positive offspring and siblings of type 1 diabetic patients. J Clin Endocrinol Metab 100:551–560
Mahon JL, Sosenko JM, Rafkin-Mervis et al (2009) The TrialNet Natural History Study of the Development of Type 1 Diabetes: objectives, design, and initial results. Pediatr Diabetes 10:97–104
Sosenko JM, Skyler JS, Herold KC, Palmer JP, Type 1 Diabetes TrialNet and Diabetes Prevention Trial-Type 1 Study Groups (2012) The metabolic progression to type 1 diabetes as indicated by serial oral glucose tolerance testing in the Diabetes Prevention Trial-type 1. Diabetes 61:1331–1337
Sosenko JM, Skyler JS, Beam AC et al (2013) Acceleration of the loss of the first-phase insulin response during the progression to type 1 diabetes in diabetes prevention trial-type 1 participants. Diabetes 62:4179–4183
Brancato D, Saura G, Fleres M et al (2013) Prognostic accuracy of continuous glucose monitoring in the prediction of diabetes mellitus in children with incidental hyperglycaemia: receiver operating characteristic analysis. Diabetes Technol Ther 15:580–585
Steck AK, Dong F, Taki I, Hoffman M, Klingensmith GJ, Rewers MJ (2014) Early hyperglycaemia detected by continuous glucose monitoring in children at risk for type 1 diabetes. Diabetes Care 37:2031–2033
Stene LC, Barriga K, Hoffman M et al (2006) Normal but increasing hemoglobin A1c levels predict progression from islet autoimmunity to overt type 1 diabetes: Diabetes Autoimmunity Study in the Young (DAISY). Pediatr Diabetes 7:247–253
Vehik K, Cuthbertson D, Boulware D et al (2012) Performance of HbA1c as an early diagnostic indicator of type 1 diabetes in children and youth. Diabetes Care 35:1821–1825
Gillard P, Hilbrands R, Van De Velde U et al (2013) Minimal functional β-cell mass in intraportal implants that reduces glycaemic variability in type 1 diabetic recipients. Diabetes Care 36:3483–3488
Gorus FK, Balti EV, Vermeulen I et al (2013) Screening for insulinoma antigen 2 and zinc transporter 8 autoantibodies: a cost-effective and age-independent strategy to identify rapid progressors to clinical onset among relatives of type 1 diabetic patients. Clin Exp Immunol 171:82–90
DeFronzo RA, Tobin JD, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237:E214–E223
Elahi D (1996) In praise of the hyperglycaemic clamp test. Diabetes Care 19:278–286
American Diabetes Association (2014) Diagnosis and classification of diabetes mellitus. Diabetes Care 37(Suppl 1):S81–S90
Lombardo F, Valenzise M, Wasniewska M et al (2002) Two-year prospective evaluation of the factors affecting honeymoon frequency and duration in children with insulin dependent diabetes mellitus: the key-role of age at diagnosis. Diabetes Nutr Metab 15:246–251
Ahren B, Pacini G (2004) Importance of quantifying insulin secretion in relation to insulin sensitivity to accurately assess beta cell function in clinical studies. Eur J Endocrinol 150:97–104
De Pauw PE, Mackin RB, Goubert P, Van Schravendijk C, Gorus FK (2009) Total error profiling of a proinsulin time-resolved fluorescence immunoassay. J Chromatogr B Analyt Technol Biomed Life Sci 877:2403–2406
Levy JC, Matthews DR, Hermans MP (1998) Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care 21:2191–2192
Siegelaar SE, Holleman F, Hoekstra JB, DeVries JH (2010) Glucose variability: does it matter? Endocr Rev 31:171–182
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group (2010) Variation of interstitial glucose measurements assessed by continuous glucose monitors in healthy, nondiabetic individuals. Diabetes Care 33:1297–1299
Mazze RS, Strock E, Wesley D et al (2008) Characterizing glucose exposure for individuals with normal glucose tolerance using continuous glucose monitoring and ambulatory glucose profile. Diabetes Technol Ther 10:149–159
Zhou J, Li H, Ran X et al (2009) Reference values for continuous glucose monitoring in Chinese subjects. Diabetes Care 32:1188–1193
Borg R, Kuenen JC, Carstensen B et al (2010) Real-life glycaemic profiles in non-diabetic individuals with low fasting glucose and normal HbA1c: the A1C-Derived Average Glucose (ADAG) study. Diabetologia 52:1608–1611
Hill NR, Oliver NS, Choudhary LJC, Hindmarsh P, Matthews DR (2011) Normal reference range for mean tissue glucose and glycemic variability derived from continuous glucose monitoring for subjects without diabetes in different ethnic groups. Diabetes Technol Ther 13:921–928
Sjaarda L, Lee S, Tfayli H, Bacha F, Bertolet M, Arslanian S (2013) Measuring β-cell function relative to insulin sensitivity in youth. Diabetes Care 36:1607–1612
Uwaifo GI, Fallon EM, Chin J, Elberg J, Parikh SJ, Yanovski JA (2001) Indices of insulin action, disposal and secretion derived from fasting samples and clamps in normal glucose-tolerant black and white children. Diabetes Care 25:2081–2087
Uwaifo GI, Parikh SJ, Keil M, Elberg J, Chin J, Yanovski JA (2002) Comparison of insulin sensitivity, clearance, and secretion estimates using euglycaemic and hyperglycaemic clamps in children. J Clin Endocrinol Metab 87:2899–2905
Mitrakou A, Vuorinen-Markkola H, Raptis G et al (1992) Simultaneous assessment of insulin secretion and insulin sensitivity using a hyperglycaemic clamp. J Clin Endocrinol Metab 75:379–382
Kahn SE, Prigeon RL, Mcculloch DK et al (1993) Quantification of the relationship between insulin sensitivity and β-cell function in human subjects. Evidence for a hyperbolic function. Diabetes 42:1663–1672
Xu P, Cuthbertson D, Greenbaum C, Palmer JP, Krischer JP, the Diabetes Prevention Trial-Type 1 Study Group (2007) Role of insulin resistance in predicting progression to type 1 diabetes. Diabetes Care 30:2314–2320
Siljander HT, Hermann R, Hekkala A et al (2013) Insulin secretion and sensitivity in the prediction of type 1 diabetes in children with advanced beta-cell autoimmunity. Eur J Endocrinol 169:479–485
Fourlanos S, Narendran P, Byrnes GB, Colman PG, Harrison LC (2004) Insulin resistance is a risk factor for progression to type 1 diabetes. Diabetologia 47:1661–1667
Bingley PJ, Mahon JL, Gale EA, the European Nicotinamide Diabetes Intervention Trial (ENDIT) Group (2008) Insulin resistance and progression to type 1 diabetes in the European Nicotinamide Diabetes Intervention Trial (ENDIT). Diabetes 31:146–150
Chen T, Xu F, Su J et al (2013) Glycaemic variability in relation to oral disposition index in the subjects with different stages of glucose tolerance. Diabetol Metabol Syndr 5:38
Krischer JP, the Type 1 Diabetes TrialNet Study Group (2013) The use of intermediate endpoints in the design of type 1 diabetes prevention trials. Diabetologia 56:1919–1924
Acknowledgements
We gratefully acknowledge the expert technical assistance of co-workers at the central unit of the Belgian Diabetes Registry, Brussels Free University (VUB, Brussels; V. Baeten, A. de Brabanter, T. De Mesmaeker, H. Dewinter, N. Diependaele, S. Exterbille, T. Glorieux, P. Goubert, C. Groven, T. Haulet, A. Ivens, D. Kesler, F. Lebleu, E. Quartier, G. Schoonjans, M. Van Molle and S. Vanderstraeten). We would also like to thank the different university teams of co-workers for their excellent assistance in organising the fieldwork for the screening of potentially eligible relatives and for performing OGTTs and hyperglycaemic clamps: at the University Hospital Antwerp (UZA, Antwerp; L. Van Gaal, R. Braspenning, J. Michiels and P. Aerts); University Hospital Brussels (UZ Brussel, Brussels; T. De Mesmaeker, S. Exterbille, P. Goubert, C. Groven, V. Kemels, C. Tettelin, S. Vanderstraeten and A. Walgraeve); University Hospital Ghent (UZ Gent, Ghent; J.M. Kaufman, A. Hutse, A. Rawoens, N. Steyaert, S. Deneve and N. Platteau) and University Hospital Leuven (UZ Leuven, Leuven; C. Mathieu, M. Carpentier, M. Robijn, K. Rouffé, A. Schoonis, H. Morobé, S. Achten and R. Van Heyste). We gratefully acknowledge A. Arrieta (Medtronic Bakken Research Center BV, Maastricht, the Netherlands), who developed the GlyVarT program. We sincerely thank the members of the Belgian Diabetes Registry who contributed to the recruitment of relatives and handling of samples for the present study: K. Casteels, C. Mathieu, P. Gillard (UZ Leuven, Leuven); L. Crenier (Hôpital Erasme, Brussels); J. De Schepper, I. Gies, B. Keymeulen, J. Vanbesien, I. Weets (UZ Brussel, Brussels); K. Decochez, E. Vandemeulebroucke (AZ Jan Portaels, Vilvoorde); C. De Block, A. France, L. Van Gaal (UZA, Edegem); G. Lamberigts (AZ St Jan, Bruges); G. Massa (Virga Jesse Ziekenhuis, Hasselt); A. Messaaoui (HUDERF, Brussels); T. Mouraux (UCL Mont- Godinne, Yvoir); A. Nollet (Regionaal Ziekenhuis Jan Yperman, Ieper); D. Rocour-Brumioul (CHR de la Citadelle, Liège); A. Scheen (CHU Sart Tilman, Liège); N. Seret (CH St Joseph, Liège); J. Tits (ZOL Campus A. Dumont, Genk); J. Ruige, G. T’Sjoen, S. Van Aken (UZ Gent, Ghent), A. Verhaegen (ZNA Jan Palfijn, Merksem); E. Weber (Clinique St Joseph, Arlon).
We gratefully thank Å. Lernmark (then at the University of Washington, Seattle, WA, USA), M. Christie (King’s College School of Medicine and Dentistry, London, UK) and the late J.C. Hutton (Barbara Davis Center for Childhood Diabetes, Aurora, CO, USA) for their kind gifts of cDNAs for the preparation of the radioligands used to measure autoantibodies against GAD, IA2 and ZnT8, respectively.
Part of this work was presented at the 50th Annual Meeting of the EASD in Vienna, 15–19 September 2014, and at the 14th Meeting of the Immunology of Diabetes Society in Munich, 12–16 April 2015.
Funding
Medtronic provided the iPro2 devices and ENLITE sensors free of charge, and the Contour Link glucometers were donated by Bayer. The present work was supported by grants from the JDRF (Center grant 4-2005-1327 to DGP and project 17-2012-615 to FKG), the European Union (FP-7 project 241 883), the Research Foundation Flanders (FWO Vlaanderen projects G.0319.01, G.0514.04, G.0311.07, G.0374.08 and G.0868.11; senior clinical research fellowship for IW, BK and KD), the Flemish Government (grant IWT 130 138), the Vrije Universiteit Brussel (projects OZR1150, 1149 and 1615) and the Willy Gepts Fund (projects 3-2005 and 3/22-2007, and grant 2013; University Hospital Brussels [UZ Brussel]). During the past 5 years, the Belgian Diabetes Registry and its associated BioBank have been sponsored by the Center for Medical Innovation Flanders and Hippo & Friends.
Duality of interest
All authors declare that there is no duality of interest associated with this manuscript. Medtronic and Bayer were not involved in the study design, or in the collection, analysis and interpretation of data, the writing of the report or the decision to submit the paper for publication.
Contribution statement
AVD drafted the article, designed the research, contributed to the recruitment of participants, acquired data, analysed and interpreted the data, and provided statistical analysis. SD, EVB, UVdV and AW contributed to the recruitment of participants, acquired, analysed and interpreted data, provided statistical analysis, and reviewed and edited the manuscript. KD, IW, EV, PG, CDB, JR, NS, BK, DGP and FKG designed the research, contributed to the recruitment of participants, acquired, analysed and interpreted data, provided statistical analysis, and reviewed and edited the manuscript. All of the authors approved the manuscript. FKG is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Methods
(PDF 73 kb)
ESM Fig. 1
(PDF 13 kb)
ESM Table 1
(PDF 189 kb)
Rights and permissions
About this article
Cite this article
Van Dalem, A., Demeester, S., Balti, E.V. et al. Relationship between glycaemic variability and hyperglycaemic clamp-derived functional variables in (impending) type 1 diabetes. Diabetologia 58, 2753–2764 (2015). https://doi.org/10.1007/s00125-015-3761-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-015-3761-y