Abstract
Purpose of Review
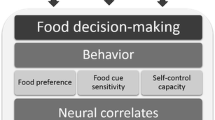
The goal of the current paper is to review the literature on the neural and behavioral factors involved in food decision-making in youth.
Recent Findings
Recent neuroimaging studies that employ passive viewing paradigms have found that exposure to food-related cues activate reward, motor planning, and attentional salience signals in children. Greater activations of reward signals and/or lower activations of control signals are associated with overeating and weight gain. Neuroimaging studies with decision-making paradigms have found the reward network in the brain activates during food choices, while control network activates less strongly.
Summary
Findings suggest that exposure to food cues activates reward/valuation network, but activation of control network tends to be relatively weaker in children. Hedonic aspects of foods are predominantly considered in children’s food choices, and their dietary self-control is not matured yet. The increased activation in reward network and the decreased activation in control network are associated with risk of developing obesity.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Linabery AM, Nahhas RW, Johnson W, Choh AC, Towne B, Odegaard AO, et al. Stronger influence of maternal than paternal obesity on infant and early childhood body mass index: the Fels Longitudinal Study. Pediatr Obes. 2013;8(3):159–69. https://doi.org/10.1111/j.2047-6310.2012.00100.x.
Arain M, Haque M, Johal L, Mathur P, Nel W, Rais A, et al. Maturation of the adolescent brain. Neuropsychiatr Dis Treat. 2013;9:449–61. https://doi.org/10.2147/NDT.S39776.
Casey BJ, Tottenham N, Liston C, Durston S. Imaging the developing brain: what have we learned about cognitive development? Trends Cogn Sci. 2005;9(3):104–10. https://doi.org/10.1016/j.tics.2005.01.011.
Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007-2008 to 2015-2016. Jama. 2018;319(16):1723–5. https://doi.org/10.1001/jama.2018.3060.
Cali AM, Caprio S. Obesity in children and adolescents. J Clin Endocrinol Metab. 2008;93(11 Suppl 1):S31–6. https://doi.org/10.1210/jc.2008-1363.
Flynn MA, McNeil DA, Maloff B, Mutasingwa D, Wu M, Ford C, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with 'best practice' recommendations. Obes Rev. 2006;7(Suppl 1):7–66. https://doi.org/10.1111/j.1467-789X.2006.00242.x.
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. Jama. 2016;315(21):2292–9. https://doi.org/10.1001/jama.2016.6361.
Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12–7.e2. https://doi.org/10.1016/j.jpeds.2006.08.042.
van Geel M, Vedder P, Tanilon J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the correlation between weight status and bullying. Int J Obes. 2014;38(10):1263–7. https://doi.org/10.1038/ijo.2014.117.
Puhl RM, King KM. Weight discrimination and bullying. Best Pract Res Clin Endocrinol Metab. 2013;27(2):117–27. https://doi.org/10.1016/j.beem.2012.12.002.
May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999-2008. Pediatrics. 2012;129(6):1035–41. https://doi.org/10.1542/peds.2011-1082.
Rankin J, Matthews L, Cobley S, Han A, Sanders R, Wiltshire HD, et al. Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolesc Health Med Ther. 2016;7:125–46. https://doi.org/10.2147/ahmt.s101631.
Obesity WHTFoC. Solving the problem of childhood obesity within a generation. Washington, DC: White House Task Force on Childhood Obesity Report to the President; 2010.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17(2):95–107. https://doi.org/10.1111/obr.12334.
Bruce AS, Lim SL, Smith TR, Cherry JB, Black WR, Davis AM, et al. Apples or candy? Internal and external influences on children's food choices. Appetite. 2015;93:31–4. https://doi.org/10.1016/j.appet.2015.04.061.
Scaglioni S, Arrizza C, Vecchi F, Tedeschi S. Determinants of children's eating behavior. Am J Clin Nutr. 2011;94(6 Suppl):2006s–11s. https://doi.org/10.3945/ajcn.110.001685.
Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. J Law, Med Ethics. 2007;35(1):22–34. https://doi.org/10.1111/j.1748-720X.2007.00111.x.
Yee AZ, Lwin MO, Ho SS. The influence of parental practices on child promotive and preventive food consumption behaviors: a systematic review and meta-analysis. Int J Behav Nutr Phys Activity. 2017;14(1):47. https://doi.org/10.1186/s12966-017-0501-3.
Larsen JK, Hermans RC, Sleddens EF, Engels RC, Fisher JO, Kremers SP. How parental dietary behavior and food parenting practices affect children's dietary behavior. Interacting sources of influence? Appetite. 2015;89:246–57. https://doi.org/10.1016/j.appet.2015.02.012.
Gibbs H, Chapman-Novakofski K. A review of health literacy and its relationship to nutrition education. Top Clin Nutr. 2012;27(4):325–33. https://doi.org/10.1097/TIN.0b013e31826f8dc5.
Houldcroft L, Haycraft E, Farrow C. Peer and friend influences on children's eating. Soc Dev. 2014;23(1):19–40.
Moss M. Salt, sugar, fat: how the food giants hooked us. New York: Random House; 2014.
Ha O-R, Bruce AS, Pruitt SW, Cherry JBC, Smith TR, Burkart D, et al. Healthy eating decisions require efficient dietary self-control in children: a mouse-tracking food decision study. Appetite. 2016;105:575–81. https://doi.org/10.1016/j.appet.2016.06.027.
Hare TA, Camerer CF, Rangel A. Self-control in decision-making involves modulation of the vmPFC valuation system. Science. 2009;324(5927):646–8. https://doi.org/10.1126/science.1168450.
Casey BJ, Getz S, Galvan A. The adolescent brain. Dev Rev. 2008;28(1):62–77. https://doi.org/10.1016/j.dr.2007.08.003.
Crone EA, Steinbeis N. Neural perspectives on cognitive control development during childhood and adolescence. Trends Cogn Sci. 2017;21(3):205–15. https://doi.org/10.1016/j.tics.2017.01.003.
Carnell S, Gibson C, Benson L, Ochner CN, Geliebter A. Neuroimaging and obesity: current knowledge and future directions. Obes Rev. 2012;13(1):43–56. https://doi.org/10.1111/j.1467-789X.2011.00927.x.
Van den Eynde F, Treasure J. Neuroimaging in eating disorders and obesity: implications for research. Child Adolesc Psychiatr Clin N Am. 2009;18(1):95–115. https://doi.org/10.1016/j.chc.2008.07.016.
Stoeckel LE, Weller RE, Cook Iii EW, Twieg DB, Knowlton RC, Cox JE. Widespread reward-system activation in obese women in response to pictures of high-calorie foods. NeuroImage. 2008;41(2):636–47. https://doi.org/10.1016/j.neuroimage.2008.02.031.
Rothemund Y, Preuschhof C, Bohner G, Bauknecht H-C, Klingebiel R, Flor H, et al. Differential activation of the dorsal striatum by high-calorie visual food stimuli in obese individuals. NeuroImage. 2007;37(2):410–21. https://doi.org/10.1016/j.neuroimage.2007.05.008.
Le DSN, Pannacciulli N, Chen K, Salbe AD, Hill JO, Wing RR, et al. Less activation in the left dorsolateral prefrontal cortex in the reanalysis of the response to a meal in obese than in lean women and its association with successful weight loss. Am J Clin Nutr. 2007;86(3):573–9.
DelParigi A, Chen K, Salbe AD, Hill JO, Wing RR, Reiman EM, et al. Successful dieters have increased neural activity in cortical areas involved in the control of behavior. Int J Obes. 2006;31(3):440–8.
Leng G, Adan RAH, Belot M, Brunstrom JM, de Graaf K, Dickson SL, et al. The determinants of food choice. Proc Nutr Soc. 2016;76:1–12. https://doi.org/10.1017/S002966511600286X.
Roefs A, Franssen S, Jansen A. The dynamic nature of food reward processing in the brain. Curr Opin Clin Nutr Metab Care. 2018;21(6):444–8. https://doi.org/10.1097/mco.0000000000000504.
van der Laan LN, de Ridder DT, Viergever MA, Smeets PA. The first taste is always with the eyes: a meta-analysis on the neural correlates of processing visual food cues. Neuroimage. 2011;55(1):296–303. https://doi.org/10.1016/j.neuroimage.2010.11.055.
van Meer F, van der Laan LN, Adan RA, Viergever MA, Smeets PA. What you see is what you eat: an ALE meta-analysis of the neural correlates of food viewing in children and adolescents. NeuroImage. 2015;104:35–43. https://doi.org/10.1016/j.neuroimage.2014.09.069.
Leigh S-J, Morris MJ. The role of reward circuitry and food addiction in the obesity epidemic: an update. Biol Psychol. 2018;131:31–42. https://doi.org/10.1016/j.biopsycho.2016.12.013.
Devoto F, Zapparoli L, Bonandrini R, Berlingeri M, Ferrulli A, Luzi L, et al. Hungry brains: a meta-analytical review of brain activation imaging studies on food perception and appetite in obese individuals. Neurosci Biobehav Rev. 2018;94:271–85. https://doi.org/10.1016/j.neubiorev.2018.07.017.
Luo S, Alves J, Hardy K, Wang X, Monterosso J, Xiang AH, et al. Neural processing of food cues in pre-pubertal children. Pediatr Obes. 2019;14(2):e12435. https://doi.org/10.1111/ijpo.12435.
van Meer F, van der Laan LN, Charbonnier L, Viergever MA, Adan RA, Smeets PA, et al. Developmental differences in the brain response to unhealthy food cues: an fMRI study of children and adults. Am J Clin Nutr. 2016;104(6):1515–22. https://doi.org/10.3945/ajcn.116.137240.
Samara A, Li X, Pivik RT, Badger TM, Ou X. Brain activation to high-calorie food images in healthy normal weight and obese children: a fMRI study. BMC Obes. 2018;5:31. https://doi.org/10.1186/s40608-018-0209-1.
• English LK, Fearnbach SN, Wilson SJ, Fisher JO, Savage JS, Rolls BJ, et al. Food portion size and energy density evoke different patterns of brain activation in children. Am J Clin Nutr. 2017;105(2):295–305. https://doi.org/10.3945/ajcn.116.136903Large Portion sizes suppressed activation of inhibitory control network, and high energy-dense foods provoked greater activations in reward and gustatory networks.
Fearnbach SN, English LK, Lasschuijt M, Wilson SJ, Savage JS, Fisher JO, et al. Brain response to images of food varying in energy density is associated with body composition in 7- to 10-year-old children: results of an exploratory study. Physiol Behav. 2016;162:3–9. https://doi.org/10.1016/j.physbeh.2016.03.007.
Carnell S, Benson L, Chang KV, Wang Z, Huo Y, Geliebter A, et al. Neural correlates of familial obesity risk and overweight in adolescence. NeuroImage. 2017;159:236–47. https://doi.org/10.1016/j.neuroimage.2017.07.052.
Bohon C. Brain response to taste in overweight children: a pilot feasibility study. PLoS One. 2017;12(2):e0172604. https://doi.org/10.1371/journal.pone.0172604.
•• Shearrer GE, Stice E, Burger KS. Adolescents at high risk of obesity show greater striatal response to increased sugar content in milkshakes. Am J Clin Nutr. 2018;107(6):859–66. https://doi.org/10.1093/ajcn/nqy050Activations in striatal, hedonic reward systems in response to sweet liquid foods were greater in adolescents with parental obesity risk compare to those without parental obesity risk. Increased level of reward network activation is related to high-obesity-risk.
•• Stice E, Yokum S. Gain in body fat is associated with increased striatal response to palatable food cues, whereas body fat stability is associated with decreased striatal response. J Neurosci. 2016;36(26):6949–56. https://doi.org/10.1523/JNEUROSCI.4365-15.2016Increased activations in reward network in response to anticipations to liquid foods were shown in adolescents who gained body fat, whereas adolescents who maintained or lost body fat showed decreased activations in reward network.
Stice E, Yokum S. Relation of neural response to palatable food tastes and images to future weight gain: using bootstrap sampling to examine replicability of neuroimaging findings. NeuroImage. 2018;183:522–31. https://doi.org/10.1016/j.neuroimage.2018.08.035.
Adise S, Geier CF, Roberts NJ, White CN, Keller KL. Is brain response to food rewards related to overeating? A test of the reward surfeit model of overeating in children. Appetite. 2018;128:167–79. https://doi.org/10.1016/j.appet.2018.06.014.
Powell LM, Schermbeck RM, Chaloupka FJ. Nutritional content of food and beverage products in television advertisements seen on children's programming. Child Obes. 2013;9(6):524–31. https://doi.org/10.1089/chi.2013.0072.
Gearhardt AN, Yokum S, Harris JL, Epstein LH, Lumeng JC. Neural response to fast food commercials in adolescents predicts intake. Am J Clin Nutr. 2020;111:493–502. https://doi.org/10.1093/ajcn/nqz305.
Masterson TD, Stein WM, Beidler E, Bermudez M, English LK, Keller KL. Brain response to food brands correlates with increased intake from branded meals in children: an fMRI study. Brain Imaging Behav. 2019;13(4):1035–48. https://doi.org/10.1007/s11682-018-9919-8.
•• Lim SL, Cherry JB, Davis AM, Balakrishnan SN, Ha OR, Bruce JM, et al. The child brain computes and utilizes internalized maternal choices. Nat Commun. 2016;7:11700. https://doi.org/10.1038/ncomms11700When children made own food choices, reward signals activated primarily and faster than control signals. When children made perceived maternal food choices for them, inhibitory signals involved in food decision-making, which suggested that neural internalization of parental regulation may guide children’s decision-making until the maturation of dietary self-control.
•• van Meer F, van der Laan LN, Viergever MA, Adan RAH, Smeets PAM, Consortium IF. Considering healthiness promotes healthier choices but modulates medial prefrontal cortex differently in children compared with adults. NeuroImage. 2017;159:325–33. https://doi.org/10.1016/j.neuroimage.2017.08.007Choices of accepting foods activated greater responses in the ventromedial prefrontal cortex (reward network). Compared to adults, the activation of the dorsolateral prefrontal cortex (control network) in response to foods was weaker in children during food choices.
• Bruce AS, Pruitt SW, Ha OR, Cherry JB, Smith TR, Bruce JM, et al. The influence of televised food commercials on children's food choices: evidence from ventromedial prefrontal cortex activations. J Pediatr. 2016;177:27–32 e1. https://doi.org/10.1016/j.jpeds.2016.06.067Exposure to food commercials increased activations in the ventromedial prefrontal cortex (reward network) during food choices.
Brown TJ, Mead E, Ells LJ. Behavior-changing interventions for treating overweight or obesity in children aged 6 to 11 years. JAMA Pediatr. 2019;173(4):385–6. https://doi.org/10.1001/jamapediatrics.2018.5494.
Brown T, Moore TH, Hooper L, Gao Y, Zayegh A, Ijaz S, et al. Interventions for preventing obesity in children. Cochrane Database System Rev. 2019;7:Cd001871. https://doi.org/10.1002/14651858.CD001871.pub4.
Rollins BY, Savage JS, Fisher JO, Birch LL. Alternatives to restrictive feeding practices to promote self-regulation in childhood: a developmental perspective. Pediatr Obes. 2016;11(5):326–32. https://doi.org/10.1111/ijpo.12071.
Fonagy P, Target M. Early intervention and the development of self-regulation. Psychoanal Inq. 2002;22(3):307–35. https://doi.org/10.1080/07351692209348990.
Diamond A, Barnett WS, Thomas J, Munro S. Preschool program improves cognitive control. Science. 2007;318(5855):1387–8. https://doi.org/10.1126/science.1151148.
Blair C, Diamond A. Biological processes in prevention and intervention: the promotion of self-regulation as a means of preventing school failure. Dev Psychopathol. 2008;20(3):899–911. https://doi.org/10.1017/S0954579408000436.
Ha O-R, Killian H, Bruce JM, Lim S-L, Bruce AS. Food advertising literacy training reduces the importance of taste in children’s food decision-making: a pilot study. Front Psychol. 2018;9(1293). https://doi.org/10.3389/fpsyg.2018.01293.
Kochanska G, Philibert RA, Barry RA. Interplay of genes and early mother-child relationship in the development of self-regulation from toddler to preschool age. J Child Psychol Psychiatry Allied Discip. 2009;50(11):1331–8. https://doi.org/10.1111/j.1469-7610.2008.02050.x.
Kochanska G, Coy KC, Murray KT. The development of self-regulation in the first four years of life. Child Dev. 2001;72(4):1091–111.
Bandura A, Grusec JE, Menlove FL. Observational learning as a function of symbolization and incentive set. Child Dev. 1966;37(3):499–506.
Frankel LA, Hughes SO, O'Connor TM, Power TG, Fisher JO, Hazen NL. Parental influences on children's self-regulation of energy intake: insights from developmental literature on emotion regulation. J Obes. 2012;2012:327259–12. https://doi.org/10.1155/2012/327259.
Galinsky AD, Maddux WW, Gilin D, White JB. Why it pays to get inside the head of your opponent: the differential effects of perspective taking and empathy in negotiations. Psychol Sci. 2008;19(4):378–84. https://doi.org/10.1111/j.1467-9280.2008.02096.x.
Anderson SE, Keim SA. Parent-child interaction, self-regulation, and obesity prevention in early childhood. Curr Obes Rep. 2016;5(2):192–200. https://doi.org/10.1007/s13679-016-0208-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Nutrition and the Brain
Rights and permissions
About this article
Cite this article
Ha, OR., Lim, SL. & Bruce, A.S. Neural Mechanisms of Food Decision-Making in Children. Curr Nutr Rep 9, 236–250 (2020). https://doi.org/10.1007/s13668-020-00321-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-020-00321-5