Abstract
Allogeneic hematopoietic cell transplantation (HCT) is the most potent therapy for preventing relapse of acute myeloid leukemia (AML). Although its efficacy is compromised by a high risk of treatment-related morbidity and mortality, an accumulating body of evidence has led to the general recommendation favoring allogeneic HCT from a matched sibling donor during first complete remission (CR1) for younger patients with cytogenetically intermediate- or high-risk AML. Over the past few decades, this field has seen a great many advancements. The indications for allogeneic HCT have been refined by taking into account the molecular profiles of leukemic cells and the degree of comorbidities. The introduction of high-resolution human leukocyte antigen-typing technology and advances in immunosuppressive therapy and supportive care measures have improved outcomes in alternative donor transplantation, while the parallel growth of unrelated donor registries and greater use of umbilical cord blood and haploidentical donors have considerably improved the chance of finding an alternative donor. The development of reduced-intensity and non-myeloablative conditioning has made it possible to receive allogeneic HCT for patients who might once have been considered ineligible due to advanced age or comorbidities. Thanks to these advances, the role of allogeneic HCT during CR1 has become progressively more important in the treatment of AML.
Similar content being viewed by others
Introduction
Achievement of complete remission (CR) is the first step in improving outcomes for patients with acute myeloid leukemia (AML). With standard induction chemotherapy, more than 70 % of younger patients and approximately 50 % of older patients can achieve CR [1, 2]. Post-remission chemotherapy plays a critical role in eradicating residual leukemic cells and obtaining long-term disease control, because CR cannot last long without further therapy [3]. However, the same holds true even if post-remission chemotherapy is used for a substantial proportion of patients.
In this context, allogeneic hematopoietic cell transplantation (HCT) is currently the most potent therapy for preventing relapse of AML, owing to cytoreduction induced by the pre-transplantation conditioning therapy and the post-transplantation graft-versus-leukemia effect. The efficacy of allogeneic HCT is, however, compromised by a high risk of treatment-related morbidity and mortality, making it a matter of continuing debate whether allogeneic HCT during first CR (CR1) yields net benefits for patients with AML.
Recently, there have been great many advancements potentially related to this question, including refinements of AML risk stratification, increased availability of alternative donors, and widespread use of reduced-intensity conditioning (RIC). This article reviews and discusses current clinical aspects of allogeneic HCT for AML during CR1, with the focus on indications for allogeneic HCT, timing of transplantation, donor sources, and conditioning regimens.
Who will benefit from allogeneic HCT during CR1?
AML represents a heterogeneous disease consisting of various biological, clinical and prognostic subgroups. While the anti-leukemic effect of allogeneic HCT is more powerful than that of standard chemotherapy, the associated morbidity and mortality warrant careful selection of patients who are most likely to benefit from the procedure. Thorough assessment is, therefore, needed when determining whether to opt for allogeneic HCT during CR1 in terms of balancing between the risks of non-relapse mortality and of relapse, with special emphasis on the anticipated risk of relapse following chemotherapy and that of non-relapse mortality following allogeneic HCT.
Prediction of outcomes following chemotherapy
Several factors are known to differentiate AML patients at different levels of risk of relapse following chemotherapy. These include age, initial white blood cell count, cytogenetics, molecular status, prior history of myelodysplastic syndrome or cytotoxic therapy for another disorder, and number of induction courses required to achieve CR1. Among these, cytogenetic findings identified at diagnosis have been the mainstay for prognostication of AML. On the basis of these findings, patients are generally stratified into favorable, intermediate and adverse risk categories (Table 1) [4–6]. Although not included in these risk-stratification systems, the monosomal karyotype, defined as two or more distinct autosomal monosomies or a single autosomal monosomy in the presence of other structural abnormalities, has recently been shown to be predictive of extremely poor prognosis, with virtually no long-term survival expected without allogeneic HCT [7–11].
Despite the clinical usefulness of risk stratification based on cytogenetics, patients in each cytogenetic risk group remain prognostically heterogeneous. This is especially true for those with cytogenetically normal AML (CN-AML), which accounts for approximately 40–50 % of all AML cases [12].
Recent advances in understanding the molecular pathogenesis of AML have further refined prognostication of patients with CN-AML. Specifically, the presence or absence of genetic aberrations in the FLT3, NPM1, and CEBPA genes has proven helpful for categorizing patients with CN-AML into different prognostic subgroups [13–24]. By integrating cytogenetic and molecular profiles, an expert panel of the European LeukemiaNet proposed a risk-stratification system for AML (Table 2) [25]. In addition, the expansion of molecular testings to other mutations involving genes such as KIT, DNMT3A, TET2, IDH1, IDH2 can be expected to further refine our current ability to predict outcomes following chemotherapy for AML patients [26–33].
In addition to these disease-related factors, recent studies have shown that findings for minimal residual disease detected by flow cytometry or quantitative reverse-transcribed polymerase chain reaction during or after chemotherapy can identify patients in CR who are at high risk of subsequent relapse [34, 35]. Further information regarding such response-related factors may well improve the currently available risk stratification, for which the results of ongoing and future investigations are eagerly awaited.
Prediction of outcomes following allogeneic HCT during CR1
Although previous studies have demonstrated the prognostic impact of cytogenetic findings at diagnosis on the risk of relapse after allogeneic HCT during CR1 [36–38], the degree to which they affect the outcomes for transplanted patients appears to be much smaller than for patients treated with chemotherapy alone. Results of recent studies suggest that the adverse effect of unfavorable cytogenetics on post-transplantation outcomes is due, at least partly, to poor results for those with monosomal karyotype [10, 11, 39, 40]. Post-transplantation relapse occurs significantly more frequently in patients with monosomal karyotype than in other cytogenetic subgroups, indicating that allogeneic HCT during CR1 may be able to improve, but not completely override the poor prognosis associated with monosomal karyotype. Likewise, the presence of internal tandem duplication of the FLT3 gene (FLT3-ITD) was shown to correlate with poorer outcomes for CN-AML patients undergoing allogeneic HCT during CR1 [41]. While such information can be useful for predicting outcomes after transplantation, a high risk of post-transplantation relapse alone does not abandon allogeneic HCT during CR1 as an option because much more unfavorable prognosis can be expected if allogeneic HCT is not used for such patients.
Of greater importance is the assessment of the risk of non-relapse mortality after transplantation. Investigators at the Fred Hutchinson Cancer Research Center have demonstrated that comorbidities have an independent value for predicting post-transplantation outcomes by developing a scoring system called “HCT-specific comorbidity index (HCT-CI)” (Table 3) [42, 43]. The HCT-CI evaluates 17 kinds of comorbidities, to each of which 0–3 points are assigned based on severity, and the total score has been shown to be significantly associated with overall survival (OS) for patients with AML undergoing allogeneic HCT during CR1 [43]. Another well-known risk assessment tool is the European Group for Blood and Marrow Transplantation (EBMT) risk score (Table 4) [44, 45]. The EBMT risk score has five components: disease stage, patient age, donor type, time interval from diagnosis to transplantation, and donor-recipient sex combination. Although the EBMT risk score was originally developed for patients with chronic myeloid leukemia undergoing allogeneic HCT [44], it has been subsequently validated for AML [45]. These predictive models are increasingly being used in both clinical studies and clinical practice.
Timing of transplantation
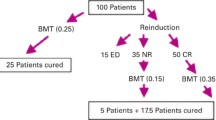
Retrospective studies reported a disease-free survival (DFS) rate of 40–50 % for patients receiving allogeneic HCT during second CR (CR2), intimating that the chance of a cure remains relatively high even if the first-line chemotherapy fails [46]. This notion often leads to the recommendation to wait until relapse to administer allogeneic HCT. However, caution should be exercised in view of the fact that such favorable results were obtained from highly selected patients who had achieved CR2 and remained relapse-free and fit enough for allogeneic HCT until transplantation could be performed. In reality, a majority of patients who have experienced relapse do not qualify for allogeneic HCT during CR2, because of failure to achieve CR2, relapse after achieving CR2, or development of organ toxicity or serious infection associated with chemotherapy for disease relapse, and the prognosis of such patients is quite dismal [47, 48]. This situation argues against the strategy of waiting until relapse to perform allogeneic HCT.
Another question regarding the timing of transplantation is, if allogeneic HCT during CR1 is chosen, when it should be performed. Moreover, do patients undergoing allogeneic HCT during CR1 benefit from receiving additional chemotherapy before transplantation? While no prospective studies have addressed the latter question, several retrospective studies have evaluated the effect of post-remission chemotherapy before allogeneic HCT [49–53], with none of those studies showing any benefit of adding chemotherapy prior to transplantation. Even when RIC allogeneic HCT is used, where pre-transplantation chemotherapy may conceivably have some advantage in terms of reducing the risk of post-transplantation relapse, there is no evidence to support the use of additional consolidation chemotherapy [52, 53]. On the other hand, several observational studies have reported that the primary reason for not proceeding to allogeneic HCT during CR1 was early relapse [54, 55]. There also remains concern over the possibility that the toxicity resulting from extra consolidation chemotherapy may increase the risk of transplantation-related mortality and even preclude the use of subsequent allogeneic HCT. Taking these findings and considerations together suggests it is advisable, provided a suitable donor is readily available, to perform allogeneic HCT as soon as possible after achievement of CR1.
Donor sources
A human leukocyte antigen (HLA)-identical related donor is the donor of choice for allogeneic HCT. However, since only approximately 40 % of individuals have a matched related donor [54–56], the remaining 60 % need to find an alternative donor to receive allogeneic HCT, such as a matched unrelated donor, umbilical cord blood (UCB), and mismatched related and unrelated donors. Outcomes of alternative donor transplantation have improved over the past decades, primarily due to the introduction of high-resolution HLA-typing technology as well as improvements in immunosuppressive therapy and supportive care measures. In addition, the growth of unrelated donor registries, and the increasing use of UCB and haploidentical donors have enhanced the chances of finding an alternative donor. This section discusses allogeneic HCT from various types of donors.
Related donors
The question of whether allogeneic HCT during CR1 is beneficial for AML patients has historically been examined in prospective studies that used biologic assignment according to donor availability, in which patients with and without an HLA-identical sibling donor were assigned to allogeneic HCT and chemotherapy/autologous HCT, respectively [57–64]. The results for all patients were then analyzed in terms of intention-to-treat, that is, as belonging to the treatment group they were assigned to, regardless of the treatment actually performed. Although such a study design is not truly randomized, the methodology reduces the selection bias that could not be eliminated in retrospective comparisons. When we combine the results from such “donor vs no-donor” studies, we find that allogeneic HCT during CR1 confers a survival advantage for patients with cytogenetically intermediate and adverse risk, but not for those with cytogenetically favorable risk [62, 65, 66]. This has led to the general recommendation favoring allogeneic HCT from a matched sibling donor during CR1 for younger patients with cytogenetically non-favorable AML. More recently, studies have been conducted regarding the interactions between molecular profiles of leukemia and effects of allogeneic HCT during CR1 for patients with CN-AML. A meta-analysis using individual patient data of four “donor versus no-donor” studies conducted by the German-Austrian AML Study Group showed that patients in the donor group had significantly better relapse-free survival than those in the no-donor group if the patients presented with FLT3-ITD or with wild-type NPM1/no FLT3-ITD [67]. However, no beneficial effect of allogeneic HCT was observed for patients with mutant NPM1/no FLT3-ITD. While these “donor versus no-donor” studies undoubtedly have made significant contributions to the elucidations of the role of allogeneic HCT during CR1, they do not provide an accurate picture of current clinical practice, because an HLA-identical sibling is not the only donor source any longer. Results of previous studies, therefore, need to be interpreted with this in mind.
Regarding HLA-mismatched related donors, several studies have made it clear that a one-antigen mismatch appears to be acceptable [68, 69]. However, an HLA-B antigen mismatch in the graft-versus-host (GVH) direction may be associated with higher risk of non-relapse mortality and inferior OS [70].
Unrelated donors
Non-relapse mortality is the primary obstacle to the success of unrelated HCT. Early studies showed less satisfactory results with unrelated HCT due to a high incidence of non-relapse mortality [71, 72]. However, there have been significant improvements in the outcome of unrelated HCT with the aid of high-resolution HLA typing, increased use of RIC, and better immunosuppressive therapy and supportive care measures. As a consequence, more recent data have shown that allogeneic HCT from an unrelated donor matched at HLA-A, -B, -C, and -DRB1 at the allelic level (hereafter referred to as an 8/8 match) yields results very similar to those of allogeneic HCT from a matched related donor [56, 73–75]. The use of an 8/8 matched unrelated donor is now a fully established choice when a matched related donor is not available. Recently, several groups have conducted prospective “donor versus no-donor” studies for patients with high-risk AML by expanding the type of donor to include unrelated donors [76, 77]. Although the number of patients in each of these studies was limited, they showed not only significantly superior OS for patients with a donor compared to those without a donor, but also similar OS for patients undergoing related and unrelated HCT.
A single HLA allele mismatch is significantly associated with development of graft-versus-host disease (GVHD) and non-relapse mortality, making outcomes for 7/8 unrelated HCT inferior to those for 8/8 unrelated HCT [78, 79]. Nevertheless, given the reported OS rate of approximately 30 % following 7/8 unrelated HCT for patients with cytogenetically unfavorable AML [74], this procedure still appears to be an acceptable choice if the patient has a high-risk disease and no alternative donor is available.
One major problem associated with unrelated HCT involves the time required for donor search, which generally takes several months and sometimes prevents the use of unrelated HCT during CR1.
Umbilical cord blood
The use of UCB as an alternative hematopoietic cell sources has been rapidly expanding in recent years. As UCB units are already cryopreserved and HLA typed, they may overcome the problems associated with lengthy search time. Another advantage of UCB is fewer restrictions to HLA matching. On the other hand, the most important limitation of UCB is the low cell dose contained in a single unit, which can lead to delayed engraftment, with subsequent post-transplantation infection and even early death. Several large retrospective studies have been conducted to compare UCB transplantation (UCBT) and unrelated bone marrow transplantation (UBMT) [80–83]. Two earlier studies analyzed registry data of adult patients with acute leukemia who had undergone UCBT or UBMT. One of these showed that UCBT was equivalent to mismatched UBMT, but inferior to matched UBMT in terms of non-relapse mortality and OS [80], while another found no differences in outcomes [81]. A more recent study reported that UCBT exhibited worse leukemia-free survival (LFS) and OS than UBMT for patients with AML, with the difference seemingly more pronounced if the analysis was restricted to those receiving their transplantation during CR1 [82]. These observations lead to the notion that outcomes for the use of UCBT in AML therapy may be similar or possibly inferior to those for UBMT. However, all of these studies are confounded by significant bias, because they dealt only with patients who actually underwent transplantation, thus did not consider immediate availability of UCBT, which is a clinically significant factor for opportunities to receive allogeneic HCT before relapse occurs. Given that prospective comparisons of UCBT versus UBMT seem to be difficult to conduct practically, an alternative analytical approach such as a decision analysis is warranted to provide more accurate insights into this issue.
Many attempts have been made to improve UCB outcomes, while others are in progress. Several investigators have used the strategies of double UCB transplantation [84], intra-bone marrow injection of UCB [85], and expansion of UCB units [86]. These efforts are expected to overcome the current limitations of UCBT, especially the relatively high risk of non-relapse mortality.
Haploidentical donors
Allogeneic HCT from haploidentical donors has the unique advantages of rapid availability and a very high chance of finding a donor (theoretically 100 % for a biological parent or child, and 50 % for a sibling). The major obstacle to the success of haploidentical HCT is intense alloreactivity via T-cells both in the GVH and host-versus-graft (HVG) directions. Early attempts to use T-cell-replete grafts resulted in unacceptable rates of GVHD, graft rejection, and non-relapse mortality [87, 88], while ex vivo T-cell depletion reduces the risk of GVHD, but likely produces graft failure [89, 90]. The problem of graft failure may be overcome by infusing a large dose of donor hematopoietic cells [91]; however, this approach is limited by slow immune recovery, resulting in high risks of post-transplantation infectious complications and non-relapse mortality. These attempts, made over a few decades, have, on the one hand, evidenced the considerable difficulties in overcoming the HLA barriers, but have also contributed to improvement in outcomes of haploidentical HCT. In their recently published prospective study, investigators in China compared T-cell-replete haploidentical HCT using G-CSF-primed grafts and anti-thymocyte globulin, with chemotherapy alone as post-remission therapy for patients with AML with intermediate- or high-risk cytogenetics [92]. They were able to demonstrate that haploidentical HCT produced a significant survival advantage over chemotherapy in terms of DFS and OS. The introduction of post-transplantation cyclophosphamide represents a recently developed alternative approach for improving T-cell-replete haploidentical HCT. When administered just after transplantation, high-dose cyclophosphamide depletes alloreactive T-cells from the donor and host, and prevents both GVH and HVG reactions. By employing this approach, acceptable rates of GVHD and non-relapse mortality have been reported [93, 94]. Haploidentical HCT is currently being developed, and further research is needed to establish optimal conditioning regimens and methods for GVHD prophylaxis. However, more favorable results can be expected to have a profound impact on the future alternative donor selection.
Conditioning regimens
The conditioning regimen administered prior to allogeneic HCT for AML has two aims: (1) suppression of the recipient’s immune system to facilitate engraftment of donor hematopoietic cells, and (2) exertion of anti-leukemic effect. Historically, myeloablative conditioning regimens were used for allogeneic HCT based on the concept that conditioning regimens must be intensive to ensure engraftment and eradicate the disease. As a matter of course, conventional conditioning regimens caused substantial morbidity and mortality, and thus limited the use of this potentially curative treatment to young patients in good medical condition. However, the development of methods to enable engraftment of donor hematopoietic cells with less intensive conditioning regimens has opened the door to a new era for allogeneic HCT [95–97]. Currently, RIC and non-myeloablative conditioning regimens are widely in use as an alternative to myeloablative conditioning regimens. Such less intensive approaches have contributed greatly to reductions in non-relapse mortality, and consequently have expanded eligibility for allogeneic HCT to older patients and those with significant comorbidities.
Myeloablative conditioning
The combinations of cyclophosphamide and total-body irradiation (CY/TBI) and of busulfan and cyclophosphamide (BU/CY) are the two most common myeloablative conditioning regimens. Several randomized studies were conducted to compare these two regimens for patients with various diseases, including AML, but with conflicting results [98–101]. A meta-analysis of these prospective randomized studies did not show any overall difference in DFS or OS between the two regimens, although there was a trend for a better long-term survival with CY/TBI for patients with AML [102]. Here, it should be noted that all of these published prospective studies used orally administered busulfan, which is known to be subject to considerable inter-patient differences in absorption and metabolism, leading to differences in exposure to this drug. Low plasma busulfan levels are associated with relapse and rejection, and high levels with hepatic sinusoidal obstruction syndrome and other toxicities [103]. However, several studies reported that the strategy combining therapeutic monitoring of plasma busulfan concentrations and individualized adjustment of the oral dose reduced the incidence of non-relapse mortality and improved survival [104, 105]. The development of intravenous (IV) formulation was another advance in ensuring more effective use of busulfan. In contrast to the oral formulation, IV busulfan has the advantage of a higher inter-patient consistency, thus allowing for tighter control of plasma busulfan levels [106, 107]. These advances have rendered the findings of previous randomized studies using oral busulfan at a fixed dose obsolete to some degree. Two more recent studies retrospectively compared CY/TBI and IV-BU/CY [108, 109]. One study, which analyzed patients with AML transplanted from a matched sibling donor during CR1 or CR2, found that LFS and OS for CY/TBI and IV-BU/CY were comparable, but that IV-BU/CY was associated with lower risk of GVHD, higher risk of relapse, and a trend toward lower non-relapse mortality [108]. In another study, which compared CY/TBI and oral or IV-BU/CY for patients with AML who underwent allogeneic HCT from a related or unrelated donor during CR1, non-relapse mortality was lower, and LFS and OS were better for IV-BU/CY than for CY/TBI, but not for oral BU/CY [109]. Despite a lack of randomized studies, these findings indicate that IV-BU/CY is a more appealing option than oral BU/CY, and either comparable to or even better than CY/TBI as a myeloablative conditioning regimen for patients with AML.
Reduced-intensity and non-myeloablative conditioning
Due to concerns about toxicity, the upper age limit for allogeneic HCT has traditionally been considered to be around 50 years. Because AML is a disease that primarily affects older adults, this potentially curative therapy could be used for only a limited number of patients. Since their development in the late 1990s, however, RIC and non-myeloablative conditioning regimens have made it possible to receive allogeneic HCT for patients who might once have been considered ineligible due to advanced age, previous therapies, and comorbidities. Current data show that morbidity and mortality following allogeneic HCT with RIC or non-myeloablative conditioning are generally lower than those associated with myeloablative conditioning, but suggest that the relapse rate may be higher, especially for patients receiving non-myeloablative conditioning [110–115]. The majority of studies comparing outcomes of RIC and/or non-myeloablative conditioning with those of myeloablative conditioning are retrospective, and thus are confounded by selection bias. To reduce such bias, one study retrospectively compared the use of RIC allogeneic HCT with that of chemotherapy alone as part of post-remission therapy in terms of availability of a matched sibling donor for 95 patients with high-risk AML in CR1 [116]. This “donor vs no-donor” analysis showed that LFS was significantly higher for the donor group than for the no-donor group. To date, only one prospective study to address this issue has been reported [117], in which outcomes for fludarabine-based RIC and those for CY/TBI were compared in a randomized fashion for patients with AML in CR1. Although the study was terminated prematurely because of slow accrual, an analysis of 195 enrolled patients showed reduction of early mortality in the first year, the primary endpoint of the study, for patients assigned to the RIC arm. This effect was prominent for patients over 40 years old, but not for younger patients. Both treatments showed similar outcomes in terms of non-relapse mortality, relapse, LFS and OS after 3 years. Although it should be remembered that no studies have ever conclusively shown the superiority of RIC or non-myeloablative conditioning over myeloablative conditioning, accumulated evidence suggests that RIC allogeneic HCT represents a practicable therapeutic option for selected patients with AML in CR1 who are considered ineligible for myeloablative allogeneic HCT.
Conclusions
The past few decades have witnessed significant advances in allogeneic HCT for AML during CR1. These advances have contributed to refinements of indications for allogeneic HCT by taking into account the molecular profiles of leukemia and the degree of comorbidities, more opportunities to find a donor by expanding donor sources beyond matched related donors, and augmentation of transplantation eligibility following the introduction of less intensive conditioning regimens. Thanks to these advances, the role of allogeneic HCT during CR1 has become increasingly more important in the treatment of AML. Despite such improvements, however, non-relapse mortality and post-transplantation relapse remain significant problems, so that further improvements in transplantation outcome need to be pursued. Furthermore, establishment of individualization of allogeneic HCT constitutes another future challenge, with regard to for whom, when and how allogeneic HCT should be integrated into treatment strategies. Such undertakings are sure to enhance our ability to provide a cure for patients with AML.
References
Yanada M, Ohtake S, Miyawaki S, Sakamaki H, Sakura T, Maeda T, et al. The demarcation between younger and older acute myeloid leukemia patients: a pooled analysis of 3 prospective studies. Cancer. 2013;119:3326–33.
Yanada M, Naoe T. Acute myeloid leukemia in older adults. Int J Hematol. 2012;96:186–93.
Cassileth PA, Harrington DP, Hines JD, Oken MM, Mazza JJ, McGlave P, et al. Maintenance chemotherapy prolongs remission duration in adult acute nonlymphocytic leukemia. J Clin Oncol. 1988;6:583–7.
Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A, et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96:4075–83.
Byrd JC, Mrozek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood. 2002;100:4325–36.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–65.
Breems DA, Van Putten WL, De Greef GE, Van Zelderen-Bhola SL, Gerssen-Schoorl KB, Mellink CH, et al. Monosomal karyotype in acute myeloid leukemia: a better indicator of poor prognosis than a complex karyotype. J Clin Oncol. 2008;26:4791–7.
Medeiros BC, Othus M, Fang M, Roulston D, Appelbaum FR. Prognostic impact of monosomal karyotype in young adult and elderly acute myeloid leukemia: the Southwest Oncology Group (SWOG) experience. Blood. 2010;116:2224–8.
Kayser S, Zucknick M, Dohner K, Krauter J, Kohne CH, Horst HA, et al. Monosomal karyotype in adult acute myeloid leukemia: prognostic impact and outcome after different treatment strategies. Blood. 2012;119:551–8.
Yanada M, Kurosawa S, Yamaguchi T, Yamashita T, Moriuchi Y, Ago H, et al. Prognosis of acute myeloid leukemia harboring monosomal karyotype in patients treated with or without allogeneic hematopoietic cell transplantation after achieving complete remission. Haematologica. 2012;97:915–8.
Cornelissen JJ, Breems D, van Putten WL, Gratwohl AA, Passweg JR, Pabst T, et al. Comparative analysis of the value of allogeneic hematopoietic stem-cell transplantation in acute myeloid leukemia with monosomal karyotype versus other cytogenetic risk categories. J Clin Oncol. 2012;30:2140–6.
Mrozek K, Marcucci G, Paschka P, Whitman SP, Bloomfield CD. Clinical relevance of mutations and gene-expression changes in adult acute myeloid leukemia with normal cytogenetics: are we ready for a prognostically prioritized molecular classification? Blood. 2007;109:431–48.
Kiyoi H, Naoe T, Nakano Y, Yokota S, Minami S, Miyawaki S, et al. Prognostic implication of FLT3 and N-RAS gene mutations in acute myeloid leukemia. Blood. 1999;93:3074–80.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA, et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001;98:1752–9.
Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, Platzbecker U, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99:4326–35.
Schnittger S, Schoch C, Dugas M, Kern W, Staib P, Wuchter C, et al. Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease. Blood. 2002;100:59–66.
Boissel N, Cayuela JM, Preudhomme C, Thomas X, Grardel N, Fund X, et al. Prognostic significance of FLT3 internal tandem repeat in patients with de novo acute myeloid leukemia treated with reinforced courses of chemotherapy. Leukemia. 2002;16:1699–704.
Falini B, Mecucci C, Tiacci E, Alcalay M, Rosati R, Pasqualucci L, et al. Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med. 2005;352:254–66.
Schnittger S, Schoch C, Kern W, Mecucci C, Tschulik C, Martelli MF, et al. Nucleophosmin gene mutations are predictors of favorable prognosis in acute myelogenous leukemia with a normal karyotype. Blood. 2005;106:3733–9.
Dohner K, Schlenk RF, Habdank M, Scholl C, Rucker FG, Corbacioglu A, et al. Mutant nucleophosmin (NPM1) predicts favorable prognosis in younger adults with acute myeloid leukemia and normal cytogenetics: interaction with other gene mutations. Blood. 2005;106:3740–6.
Thiede C, Koch S, Creutzig E, Steudel C, Illmer T, Schaich M, et al. Prevalence and prognostic impact of NPM1 mutations in 1485 adult patients with acute myeloid leukemia (AML). Blood. 2006;107:4011–20.
Marcucci G, Maharry K, Radmacher MD, Mrozek K, Vukosavljevic T, Paschka P, et al. Prognostic significance of, and gene and microRNA expression signatures associated with, CEBPA mutations in cytogenetically normal acute myeloid leukemia with high-risk molecular features: a Cancer and Leukemia Group B Study. J Clin Oncol. 2008;26:5078–87.
Wouters BJ, Lowenberg B, Erpelinck-Verschueren CA, van Putten WL, Valk PJ, Delwel R. Double CEBPA mutations, but not single CEBPA mutations, define a subgroup of acute myeloid leukemia with a distinctive gene expression profile that is uniquely associated with a favorable outcome. Blood. 2009;113:3088–91.
Renneville A, Boissel N, Gachard N, Naguib D, Bastard C, de Botton S, et al. The favorable impact of CEBPA mutations in patients with acute myeloid leukemia is only observed in the absence of associated cytogenetic abnormalities and FLT3 internal duplication. Blood. 2009;113:5090–3.
Dohner H, Estey EH, Amadori S, Appelbaum FR, Buchner T, Burnett AK, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115:453–74.
Paschka P, Marcucci G, Ruppert AS, Mrozek K, Chen H, Kittles RA, et al. Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B Study. J Clin Oncol. 2006;24:3904–11.
Green CL, Evans CM, Hills RK, Burnett AK, Linch DC, Gale RE. The prognostic significance of IDH1 mutations in younger adult patients with acute myeloid leukemia is dependent on FLT3/ITD status. Blood. 2010;116:2779–82.
Chou WC, Chou SC, Liu CY, Chen CY, Hou HA, Kuo YY, et al. TET2 mutation is an unfavorable prognostic factor in acute myeloid leukemia patients with intermediate-risk cytogenetics. Blood. 2011;118:3803–10.
Renneville A, Boissel N, Nibourel O, Berthon C, Helevaut N, Gardin C, et al. Prognostic significance of DNA methyltransferase 3A mutations in cytogenetically normal acute myeloid leukemia: a study by the Acute Leukemia French Association. Leukemia. 2012;26:1247–54.
Thol F, Damm F, Ludeking A, Winschel C, Wagner K, Morgan M, et al. Incidence and prognostic influence of DNMT3A mutations in acute myeloid leukemia. J Clin Oncol. 2011;29:2889–96.
Patel JP, Gonen M, Figueroa ME, Fernandez H, Sun Z, Racevskis J, et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med. 2012;366:1079–89.
Grossmann V, Schnittger S, Kohlmann A, Eder C, Roller A, Dicker F, et al. A novel hierarchical prognostic model of AML solely based on molecular mutations. Blood. 2012;120:2963–72.
Kihara R, Nagata Y, Kiyoi H, Kato T, Yamamoto E, Suzuki K, et al. Comprehensive analysis of genetic alterations and their prognostic impacts in adult acute myeloid leukemia patients. Leukemia. 2014;28:1586–95.
Terwijn M, van Putten WL, Kelder A, van der Velden VH, Brooimans RA, Pabst T, et al. High prognostic impact of flow cytometric minimal residual disease detection in acute myeloid leukemia: data from the HOVON/SAKK AML 42A study. J Clin Oncol. 2013;31:3889–97.
Freeman SD, Virgo P, Couzens S, Grimwade D, Russell N, Hills RK, et al. Prognostic relevance of treatment response measured by flow cytometric residual disease detection in older patients with acute myeloid leukemia. J Clin Oncol. 2013;31:4123–31.
Gale RP, Horowitz MM, Weiner RS, Ash RC, Atkinson K, Babu R, et al. Impact of cytogenetic abnormalities on outcome of bone marrow transplants in acute myelogenous leukemia in first remission. Bone Marrow Transplant. 1995;16:203–8.
Ferrant A, Labopin M, Frassoni F, Prentice HG, Cahn JY, Blaise D, et al. Karyotype in acute myeloblastic leukemia: prognostic significance for bone marrow transplantation in first remission: a European Group for Blood and Marrow Transplantation study. Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Blood. 1997;90:2931–8.
Armand P, Kim HT, DeAngelo DJ, Ho VT, Cutler CS, Stone RM, et al. Impact of cytogenetics on outcome of de novo and therapy-related AML and MDS after allogeneic transplantation. Biol Blood Marrow Transplant. 2007;13:655–64.
Oran B, Dolan M, Cao Q, Brunstein C, Warlick E, Weisdorf D. Monosomal karyotype provides better prognostic prediction after allogeneic stem cell transplantation in patients with acute myelogenous leukemia. Biol Blood Marrow Transplant. 2011;17:356–64.
Fang M, Storer B, Estey E, Othus M, Zhang L, Sandmaier BM, et al. Outcome of patients with acute myeloid leukemia with monosomal karyotype who undergo hematopoietic cell transplantation. Blood. 2011;118:1490–4.
Brunet S, Labopin M, Esteve J, Cornelissen J, Socie G, Iori AP, et al. Impact of FLT3 internal tandem duplication on the outcome of related and unrelated hematopoietic transplantation for adult acute myeloid leukemia in first remission: a retrospective analysis. J Clin Oncol. 2012;30:735–41.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Sorror ML, Giralt S, Sandmaier BM, De Lima M, Shahjahan M, Maloney DG, et al. Hematopoietic cell transplantation specific comorbidity index as an outcome predictor for patients with acute myeloid leukemia in first remission: combined FHCRC and MDACC experiences. Blood. 2007;110:4606–13.
Gratwohl A, Hermans J, Goldman JM, Arcese W, Carreras E, Devergie A, et al. Risk assessment for patients with chronic myeloid leukaemia before allogeneic blood or marrow transplantation. Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Lancet. 1998;352:1087–92.
Gratwohl A, Stern M, Brand R, Apperley J, Baldomero H, de Witte T, et al. Risk score for outcome after allogeneic hematopoietic stem cell transplantation: a retrospective analysis. Cancer. 2009;115:4715–26.
Forman SJ, Rowe JM. The myth of the second remission of acute leukemia in the adult. Blood. 2013;121:1077–82.
Kurosawa S, Yamaguchi T, Miyawaki S, Uchida N, Sakura T, Kanamori H, et al. Prognostic factors and outcomes of adult patients with acute myeloid leukemia after first relapse. Haematologica. 2010;95:1857–64.
Burnett AK, Goldstone A, Hills RK, Milligan D, Prentice A, Yin J, et al. Curability of patients with acute myeloid leukemia who did not undergo transplantation in first remission. J Clin Oncol. 2013;31:1293–301.
Cahn JY, Labopin M, Sierra J, Blaise D, Reiffers J, Ferrant A, et al. No impact of high-dose cytarabine on the outcome of patients transplanted for acute myeloblastic leukaemia in first remission. Acute Leukaemia Working Party of the European Group for Blood and Marrow Transplantation (EBMT). Br J Haematol. 2000;110:308–14.
Tallman MS, Rowlings PA, Milone G, Zhang MJ, Perez WS, Weisdorf D, et al. Effect of postremission chemotherapy before human leukocyte antigen-identical sibling transplantation for acute myelogenous leukemia in first complete remission. Blood. 2000;96:1254–8.
Sproat L, Bolwell B, Rybicki L, Tench S, Chan J, Kalaycio M, et al. Effect of post-remission chemotherapy preceding allogeneic hematopoietic cell transplant in patients with acute myeloid leukemia in first remission. Leuk Lymphoma. 2010;51:1699–704.
Warlick ED, Paulson K, Brazauskas R, Zhong X, Miller AM, Camitta BM, et al. Effect of postremission therapy before reduced-intensity conditioning allogeneic transplantation for acute myeloid leukemia in first complete remission. Biol Blood Marrow Transplant. 2014;20:202–8.
Yeshurun M, Labopin M, Blaise D, Cornelissen JJ, Sengeloev H, Vindelov L, et al. Impact of postremission consolidation chemotherapy on outcome after reduced-intensity conditioning allogeneic stem cell transplantation for patients with acute myeloid leukemia in first complete remission: a report from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Cancer. 2014;120:855–63.
Mawad R, Gooley TA, Sandhu V, Lionberger J, Scott B, Sandmaier BM, et al. Frequency of allogeneic hematopoietic cell transplantation among patients with high- or intermediate-risk acute myeloid leukemia in first complete remission. J Clin Oncol. 2013;31:3883–8.
Labopin M, Gorin NC, Polge E, Socie G, Gurman G, Gluckman E, et al. A prospective registration study to determine feasibility of hematopoietic SCT in adults with acute leukemia: planning, expectations and reality. Bone Marrow Transplant. 2014;49:376–81.
Yanada M, Kurosawa S, Yamaguchi T, Uchida N, Miyawaki S, Kanamori H, et al. Effect of related donor availability on outcome of AML in the context of related and unrelated hematopoietic cell transplantation. Bone Marrow Transplant. 2013;48:390–5.
Reiffers J, Stoppa AM, Attal M, Michallet M, Marit G, Blaise D, et al. Allogeneic vs autologous stem cell transplantation vs chemotherapy in patients with acute myeloid leukemia in first remission: the BGMT 87 study. Leukemia. 1996;10:1874–82.
Keating S, de Witte T, Suciu S, Willemze R, Hayat M, Labar B, et al. The influence of HLA-matched sibling donor availability on treatment outcome for patients with AML: an analysis of the AML 8A study of the EORTC Leukaemia Cooperative Group and GIMEMA. European Organization for Research and Treatment of Cancer. Gruppo Italiano Malattie Ematologiche Maligne dell’Adulto. Br J Haematol. 1998;102:1344–53.
Burnett AK, Wheatley K, Goldstone AH, Stevens RF, Hann IM, Rees JH, et al. The value of allogeneic bone marrow transplant in patients with acute myeloid leukaemia at differing risk of relapse: results of the UK MRC AML 10 trial. Br J Haematol. 2002;118:385–400.
Suciu S, Mandelli F, de Witte T, Zittoun R, Gallo E, Labar B, et al. Allogeneic compared with autologous stem cell transplantation in the treatment of patients younger than 46 years with acute myeloid leukemia (AML) in first complete remission (CR1): an intention-to-treat analysis of the EORTC/GIMEMAAML-10 trial. Blood. 2003;102:1232–40.
Jourdan E, Boiron JM, Dastugue N, Vey N, Marit G, Rigal-Huguet F, et al. Early allogeneic stem-cell transplantation for young adults with acute myeloblastic leukemia in first complete remission: an intent-to-treat long-term analysis of the BGMT experience. J Clin Oncol. 2005;23:7676–84.
Cornelissen JJ, van Putten WL, Verdonck LF, Theobald M, Jacky E, Daenen SM, et al. Results of a HOVON/SAKK donor versus no-donor analysis of myeloablative HLA-identical sibling stem cell transplantation in first remission acute myeloid leukemia in young and middle-aged adults: benefits for whom? Blood. 2007;109:3658–66.
Basara N, Schulze A, Wedding U, Mohren M, Gerhardt A, Junghanss C, et al. Early related or unrelated haematopoietic cell transplantation results in higher overall survival and leukaemia-free survival compared with conventional chemotherapy in high-risk acute myeloid leukaemia patients in first complete remission. Leukemia. 2009;23:635–40.
Sakamaki H, Miyawaki S, Ohtake S, Emi N, Yagasaki F, Mitani K, et al. Allogeneic stem cell transplantation versus chemotherapy as post-remission therapy for intermediate or poor risk adult acute myeloid leukemia: results of the JALSG AML97 study. Int J Hematol. 2010;91:284–92.
Yanada M, Matsuo K, Emi N, Naoe T. Efficacy of allogeneic hematopoietic stem cell transplantation depends on cytogenetic risk for acute myeloid leukemia in first disease remission: a metaanalysis. Cancer. 2005;103:1652–8.
Koreth J, Schlenk R, Kopecky KJ, Honda S, Sierra J, Djulbegovic BJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA. 2009;301:2349–61.
Schlenk RF, Dohner K, Krauter J, Frohling S, Corbacioglu A, Bullinger L, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008;358:1909–18.
Anasetti C, Beatty PG, Storb R, Martin PJ, Mori M, Sanders JE, et al. Effect of HLA incompatibility on graft-versus-host disease, relapse, and survival after marrow transplantation for patients with leukemia or lymphoma. Hum Immunol. 1990;29:79–91.
Kanda Y, Chiba S, Hirai H, Sakamaki H, Iseki T, Kodera Y, et al. Allogeneic hematopoietic stem cell transplantation from family members other than HLA-identical siblings over the last decade (1991–2000). Blood. 2003;102:1541–7.
Kanda J, Saji H, Fukuda T, Kobayashi T, Miyamura K, Eto T, et al. Related transplantation with HLA-1 Ag mismatch in the GVH direction and HLA-8/8 allele-matched unrelated transplantation: a nationwide retrospective study. Blood. 2012;119:2409–16.
Szydlo R, Goldman JM, Klein JP, Gale RP, Ash RC, Bach FH, et al. Results of allogeneic bone marrow transplants for leukemia using donors other than HLA-identical siblings. J Clin Oncol. 1997;15:1767–77.
Lazarus HM, Perez WS, Klein JP, Kollman C, Bate-Boyle B, Bredeson CN, et al. Autotransplantation versus HLA-matched unrelated donor transplantation for acute myeloid leukaemia: a retrospective analysis from the Center for International Blood and Marrow Transplant Research. Br J Haematol. 2006;132:755–69.
Schetelig J, Bornhauser M, Schmid C, Hertenstein B, Schwerdtfeger R, Martin H, et al. Matched unrelated or matched sibling donors result in comparable survival after allogeneic stem-cell transplantation in elderly patients with acute myeloid leukemia: a report from the cooperative German Transplant Study Group. J Clin Oncol. 2008;26:5183–91.
Gupta V, Tallman MS, He W, Logan BR, Copelan E, Gale RP, et al. Comparable survival after HLA-well-matched unrelated or matched sibling donor transplantation for acute myeloid leukemia in first remission with unfavorable cytogenetics at diagnosis. Blood. 2010;116:1839–48.
Walter RB, Pagel JM, Gooley TA, Petersdorf EW, Sorror ML, Woolfrey AE, et al. Comparison of matched unrelated and matched related donor myeloablative hematopoietic cell transplantation for adults with acute myeloid leukemia in first remission. Leukemia. 2010;24:1276–82.
Schlenk RF, Dohner K, Mack S, Stoppel M, Kiraly F, Gotze K, et al. Prospective evaluation of allogeneic hematopoietic stem-cell transplantation from matched related and matched unrelated donors in younger adults with high-risk acute myeloid leukemia: German–Austrian trial AMLHD98A. J Clin Oncol. 2010;28:4642–8.
Stelljes M, Beelen DW, Braess J, Sauerland MC, Heinecke A, Berning B, et al. Allogeneic transplantation as post-remission therapy for cytogenetically high-risk acute myeloid leukemia: landmark analysis from a single prospective multicenter trial. Haematologica. 2011;96:972–9.
Lee SJ, Klein J, Haagenson M, Baxter-Lowe LA, Confer DL, Eapen M, et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood. 2007;110:4576–83.
Kanda Y, Kanda J, Atsuta Y, Maeda Y, Ichinohe T, Ohashi K, et al. Impact of a single human leucocyte antigen (HLA) allele mismatch on the outcome of unrelated bone marrow transplantation over two time periods. A retrospective analysis of 3003 patients from the HLA Working Group of the Japan Society for Blood and Marrow Transplantation. Br J Haematol. 2013;161:566–77.
Laughlin MJ, Eapen M, Rubinstein P, Wagner JE, Zhang MJ, Champlin RE, et al. Outcomes after transplantation of cord blood or bone marrow from unrelated donors in adults with leukemia. N Engl J Med. 2004;351:2265–75.
Rocha V, Labopin M, Sanz G, Arcese W, Schwerdtfeger R, Bosi A, et al. Transplants of umbilical-cord blood or bone marrow from unrelated donors in adults with acute leukemia. N Engl J Med. 2004;351:2276–85.
Atsuta Y, Suzuki R, Nagamura-Inoue T, Taniguchi S, Takahashi S, Kai S, et al. Disease-specific analyses of unrelated cord blood transplantation compared with unrelated bone marrow transplantation in adult patients with acute leukemia. Blood. 2009;113:1631–8.
Eapen M, Rocha V, Sanz G, Scaradavou A, Zhang MJ, Arcese W, et al. Effect of graft source on unrelated donor haemopoietic stem-cell transplantation in adults with acute leukaemia: a retrospective analysis. Lancet Oncol. 2010;11:653–60.
Barker JN, Weisdorf DJ, DeFor TE, Blazar BR, McGlave PB, Miller JS, et al. Transplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy. Blood. 2005;105:1343–7.
Frassoni F, Gualandi F, Podesta M, Raiola AM, Ibatici A, Piaggio G, et al. Direct intrabone transplant of unrelated cord-blood cells in acute leukaemia: a phase I/II study. Lancet Oncol. 2008;9:831–9.
de Lima M, McNiece I, Robinson SN, Munsell M, Eapen M, Horowitz M, et al. Cord-blood engraftment with ex vivo mesenchymal-cell coculture. N Engl J Med. 2012;367:2305–15.
Powles RL, Morgenstern GR, Kay HE, McElwain TJ, Clink HM, Dady PJ, et al. Mismatched family donors for bone-marrow transplantation as treatment for acute leukaemia. Lancet. 1983;1:612–5.
Beatty PG, Clift RA, Mickelson EM, Nisperos BB, Flournoy N, Martin PJ, et al. Marrow transplantation from related donors other than HLA-identical siblings. N Engl J Med. 1985;313:765–71.
Ash RC, Horowitz MM, Gale RP, van Bekkum DW, Casper JT, Gordon-Smith EC, et al. Bone marrow transplantation from related donors other than HLA-identical siblings: effect of T cell depletion. Bone Marrow Transplant. 1991;7:443–52.
Mehta J, Singhal S, Gee AP, Chiang KY, Godder K, Rhee Fv F, et al. Bone marrow transplantation from partially HLA-mismatched family donors for acute leukemia: single-center experience of 201 patients. Bone Marrow Transplant. 2004;33:389–96.
Aversa F, Terenzi A, Tabilio A, Falzetti F, Carotti A, Ballanti S, et al. Full haplotype-mismatched hematopoietic stem-cell transplantation: a phase II study in patients with acute leukemia at high risk of relapse. J Clin Oncol. 2005;23:3447–54.
Huang XJ, Zhu HH, Chang YJ, Xu LP, Liu DH, Zhang XH, et al. The superiority of haploidentical related stem cell transplantation over chemotherapy alone as postremission treatment for patients with intermediate- or high-risk acute myeloid leukemia in first complete remission. Blood. 2012;119:5584–90.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50.
Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK, et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol. 2013;31:1310–6.
Giralt S, Estey E, Albitar M, van Besien K, Rondon G, Anderlini P, et al. Engraftment of allogeneic hematopoietic progenitor cells with purine analog-containing chemotherapy: harnessing graft-versus-leukemia without myeloablative therapy. Blood. 1997;89:4531–6.
Slavin S, Nagler A, Naparstek E, Kapelushnik Y, Aker M, Cividalli G, et al. Nonmyeloablative stem cell transplantation and cell therapy as an alternative to conventional bone marrow transplantation with lethal cytoreduction for the treatment of malignant and nonmalignant hematologic diseases. Blood. 1998;91:756–63.
McSweeney PA, Niederwieser D, Shizuru JA, Sandmaier BM, Molina AJ, Maloney DG, et al. Hematopoietic cell transplantation in older patients with hematologic malignancies: replacing high-dose cytotoxic therapy with graft-versus-tumor effects. Blood. 2001;97:3390–400.
Blaise D, Maraninchi D, Archimbaud E, Reiffers J, Devergie A, Jouet JP, et al. Allogeneic bone marrow transplantation for acute myeloid leukemia in first remission: a randomized trial of a busulfan-cytoxan versus cytoxan-total body irradiation as preparative regimen: a report from the Group d’Etudes de la Greffe de Moelle Osseuse. Blood. 1992;79:2578–82.
Ringden O, Ruutu T, Remberger M, Nikoskelainen J, Volin L, Vindelov L, et al. A randomized trial comparing busulfan with total body irradiation as conditioning in allogeneic marrow transplant recipients with leukemia: a report from the Nordic Bone Marrow Transplantation Group. Blood. 1994;83:2723–30.
Clift RA, Buckner CD, Thomas ED, Bensinger WI, Bowden R, Bryant E, et al. Marrow transplantation for chronic myeloid leukemia: a randomized study comparing cyclophosphamide and total body irradiation with busulfan and cyclophosphamide. Blood. 1994;84:2036–43.
Devergie A, Blaise D, Attal M, Tigaud JD, Jouet JP, Vernant JP, et al. Allogeneic bone marrow transplantation for chronic myeloid leukemia in first chronic phase: a randomized trial of busulfan-cytoxan versus cytoxan-total body irradiation as preparative regimen: a report from the French Society of Bone Marrow Graft (SFGM). Blood. 1995;85:2263–8.
Socie G, Clift RA, Blaise D, Devergie A, Ringden O, Martin PJ, et al. Busulfan plus cyclophosphamide compared with total-body irradiation plus cyclophosphamide before marrow transplantation for myeloid leukemia: long-term follow-up of 4 randomized studies. Blood. 2001;98:3569–74.
Slattery JT, Sanders JE, Buckner CD, Schaffer RL, Lambert KW, Langer FP, et al. Graft-rejection and toxicity following bone marrow transplantation in relation to busulfan pharmacokinetics. Bone Marrow Transplant. 1995;16:31–42.
Deeg HJ, Storer B, Slattery JT, Anasetti C, Doney KC, Hansen JA, et al. Conditioning with targeted busulfan and cyclophosphamide for hemopoietic stem cell transplantation from related and unrelated donors in patients with myelodysplastic syndrome. Blood. 2002;100:1201–7.
Radich JP, Gooley T, Bensinger W, Chauncey T, Clift R, Flowers M, et al. HLA-matched related hematopoietic cell transplantation for chronic-phase CML using a targeted busulfan and cyclophosphamide preparative regimen. Blood. 2003;102:31–5.
Andersson BS, Kashyap A, Gian V, Wingard JR, Fernandez H, Cagnoni PJ, et al. Conditioning therapy with intravenous busulfan and cyclophosphamide (IV BuCy2) for hematologic malignancies prior to allogeneic stem cell transplantation: a phase II study. Biol Blood Marrow Transplant. 2002;8:145–54.
Sobecks RM, Rybicki L, Yurch M, Kalaycio M, Dean R, Andresen S, et al. Intravenous compared with oral busulfan as preparation for allogeneic hematopoietic progenitor cell transplantation for AML and MDS. Bone Marrow Transplant. 2012;47:633–8.
Nagler A, Rocha V, Labopin M, Unal A, Ben Othman T, Campos A, et al. Allogeneic hematopoietic stem-cell transplantation for acute myeloid leukemia in remission: comparison of intravenous busulfan plus cyclophosphamide (Cy) versus total-body irradiation plus Cy as conditioning regimen—a report from the acute leukemia working party of the European group for blood and marrow transplantation. J Clin Oncol. 2013;31:3549–56.
Copelan EA, Hamilton BK, Avalos B, Ahn KW, Bolwell BJ, Zhu X, et al. Better leukemia-free and overall survival in AML in first remission following cyclophosphamide in combination with busulfan compared with TBI. Blood. 2013;122:3863–70.
Aoudjhane M, Labopin M, Gorin NC, Shimoni A, Ruutu T, Kolb HJ, et al. Comparative outcome of reduced intensity and myeloablative conditioning regimen in HLA identical sibling allogeneic haematopoietic stem cell transplantation for patients older than 50 years of age with acute myeloblastic leukaemia: a retrospective survey from the Acute Leukemia Working Party (ALWP) of the European group for Blood and Marrow Transplantation (EBMT). Leukemia. 2005;19:2304–12.
Hegenbart U, Niederwieser D, Sandmaier BM, Maris MB, Shizuru JA, Greinix H, et al. Treatment for acute myelogenous leukemia by low-dose, total-body, irradiation-based conditioning and hematopoietic cell transplantation from related and unrelated donors. J Clin Oncol. 2006;24:444–53.
Valcarcel D, Martino R, Caballero D, Martin J, Ferra C, Nieto JB, et al. Sustained remissions of high-risk acute myeloid leukemia and myelodysplastic syndrome after reduced-intensity conditioning allogeneic hematopoietic transplantation: chronic graft-versus-host disease is the strongest factor improving survival. J Clin Oncol. 2008;26:577–84.
Farag SS, Maharry K, Zhang MJ, Perez WS, George SL, Mrozek K, et al. Comparison of reduced-intensity hematopoietic cell transplantation with chemotherapy in patients age 60–70 years with acute myelogenous leukemia in first remission. Biol Blood Marrow Transplant. 2011;17:1796–803.
Luger SM, Ringden O, Zhang MJ, Perez WS, Bishop MR, Bornhauser M, et al. Similar outcomes using myeloablative vs reduced-intensity allogeneic transplant preparative regimens for AML or MDS. Bone Marrow Transplant. 2012;47:203–11.
Martino R, de Wreede L, Fiocco M, van Biezen A, von dem Borne PA, Hamladji RM, et al. Comparison of conditioning regimens of various intensities for allogeneic hematopoietic SCT using HLA-identical sibling donors in AML and MDS with <10 % BM blasts: a report from EBMT. Bone Marrow Transplant. 2013;48:761–70.
Mohty M, de Lavallade H, Ladaique P, Faucher C, Vey N, Coso D, et al. The role of reduced intensity conditioning allogeneic stem cell transplantation in patients with acute myeloid leukemia: a donor vs no donor comparison. Leukemia. 2005;19:916–20.
Bornhauser M, Kienast J, Trenschel R, Burchert A, Hegenbart U, Stadler M, et al. Reduced-intensity conditioning versus standard conditioning before allogeneic haemopoietic cell transplantation in patients with acute myeloid leukaemia in first complete remission: a prospective, open-label randomised phase 3 trial. Lancet Oncol. 2012;13:1035–44.
Conflict of interest
The author declares no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Yanada, M. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia during first complete remission: a clinical perspective. Int J Hematol 101, 243–254 (2015). https://doi.org/10.1007/s12185-014-1657-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-014-1657-0