Abstract
Summary
This study seeks to understand the knowledge/utilisation of osteoporosis guidelines among PCPs in Singapore, their confidence in and barriers to osteoporosis management. Knowledge and usage of guidelines was associated with confidence in management. Effective guideline adoption is therefore crucial. PCPs also need systemic support to overcome barriers to osteoporosis care.
Purpose
Primary care physicians (PCPs) are at the forefront of offering osteoporosis screening and treatment. However, osteoporosis remains under-treated in primary care, despite the existence of osteoporosis clinical practice guidelines for PCPs. This study aims to determine the self-reported knowledge and utilisation of local osteoporosis guidelines and associated sociodemographic factors and to determine the confidence and barriers to osteoporosis screening and management among PCPs in Singapore.
Methods
An anonymous web-based survey was conducted. PCPs in public and private practice were invited to participate in the self-administered survey via e-mail and messaging platforms. Chi-square test was performed for bivariate analysis; multivariable logistic regression models were used for factors with p value < 0.2.
Results
Three hundred thirty-four complete survey datasets were processed for analysis. Two hundred fifty-one PCPs (75.1%) had read the osteoporosis guidelines. 70.5% self-reported good knowledge, and 74.9% use the guidelines. PCPs who self-reported good guideline knowledge (OR = 5.84; 2.96–11.49) and utilisation (OR = 4.54; 2.21–9.34) were more likely to perceive confidence in osteoporosis management. PCPs’ perception that patients had other medical priorities during the consultation (79.3%) was the commonest barrier to screening. Limited anti-osteoporosis medication (54.1%) in the practice was a hindrance to management. Polyclinic-based PCPs frequently cited the lack of consultation time as a barrier; more systemic barriers were faced by PCPs in private practices.
Conclusion
Most PCPs know and use the local osteoporosis guidelines. Knowledge and usage of guidelines was associated with confidence in management. Strategies to address the prevalent barriers to osteoporosis screening and management faced by PCPs are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a disease characterised by low bone mass and microarchitectural deterioration of bone tissue, leading to enhanced bone fragility and increased fracture risk [1, 2]. It results in fragility fractures, such as at the spine, hip, wrist, pelvis, and humerus. Effective management of osteoporosis is crucial, because osteoporosis is expected to be a significant burden to healthcare systems [3]. The incidence of hip fractures in Singapore has increased by 1.5 times in men and 5 times in women since the 1960s. These rates are projected to increase with Singapore’s ageing population [4, 5].
Primary care physicians (PCPs) have the first-touch advantage in screening and management of osteoporosis [6]. Guidance on the screening and management of osteoporosis has been laid out in various clinical practice guidelines for primary care [7, 8]. The current osteoporosis guidelines in Singapore are known as appropriate care guides. They provide concise, evidence-based recommendations tailored to the local context [9]. The guidelines advise PCPs to use screening tools to risk stratify high-risk patients in the primary care setting [10]. The guidelines also advise PCPs to initiate pharmacological treatment for patients with osteoporosis in primary care.
However, despite the existence of guidelines for the screening and management of osteoporosis, it remains largely under-treated in primary care. A survey of PCPs in Malaysia showed that only 63.4% of respondents were aware of their local osteoporosis clinical practice guidelines, and 82.1% of respondents perceived osteoporosis to be under-diagnosed [11]. A database study of a national general practice data program in Australia showed that of the 25,188 patients with an osteoporosis diagnosis, 23.5% were not started on any medication, and PCPs expressed knowledge gaps in managing drug holidays and pharmacotherapy [12]. Mendis et al. found that 63% of patients seen in primary care who had sustained a fragility fracture were not referred for a bone density scan, and 63% did not receive specific osteoporosis pharmacotherapy [13].
One factor contributing to under-treatment of osteoporosis in primary care is a lack of knowledge on osteoporosis among PCPs [12]. Knowledge gaps in osteoporosis diagnosis and treatment have been reported among French and Canadian PCPs [14, 15]. This lack of knowledge may arise from lack of awareness and utilisation of clinical practice guidelines. Despite the potential for clinical practice guidelines to address gaps in osteoporosis care, reported real-world utilisation amongst PCPs remains low [16,17,18].
Improving the utilisation of clinical practice guidelines on osteoporosis has a role in addressing such knowledge gaps. Utilisation of guidelines was associated with competence in osteoporosis management [16]. PCPs in Germany who had knowledge of and who utilised national osteoporosis guidelines were managing more patients with osteoporosis (OR = 2.6; 1.93–3.50). PCPs in South Africa perceived the application of local osteoporosis guidelines to benefit patients and improve their management of osteoporosis [17]. MZ Tan et al. called for the need to evaluate the effectiveness of clinical practice guidelines and to engage PCPs more in their adoption [19].
Apart from knowledge gaps, PCPs face other barriers to osteoporosis care. These barriers include a lack of time to manage osteoporosis and the competing demands of managing other medical conditions; a lack of clarity of the role of PCP in osteoporosis management; and hesitancy to screen and manage yet another chronic disease [14, 15]. PCPs may also be concerned of medication cost, efficacy, side effects, and safety [14, 20, 21]. For patient-related barriers, a lack of patient awareness about osteoporosis may result in failure to initiate discussions on screening [14, 15]. Healthcare system-related barriers include the lack of access to bone mineral density (BMD) testing, lack of a national screening programme, and healthcare financing limitations [11, 14, 16, 22].
The primary objective of this study sets out to understand the self-reported knowledge and utilisation of local osteoporosis guidelines among PCPs in Singapore and to explore if guideline knowledge and utilisation is influenced by sociodemographic and practice characteristics of PCPs. We also aimed to determine the factors that influenced PCPs’ perceived confidence in osteoporosis management. The secondary objective in this study was to identify the prevalence of barriers to osteoporosis screening and management among PCPs and to determine if these barriers were influenced by practice typology. Insights from this study would be useful in addressing knowledge and systemic gaps in osteoporosis care, so that guidelines, education, and healthcare resources can be implemented accordingly.
Methods
A cross-sectional web-based survey using a questionnaire was conducted for this study. An Internet-based platform was used to reach a wider PCP population, as well as to overcome the physical distancing measures imposed by the COVID-19 pandemic.
Development of questionnaire
An original questionnaire was designed with questions in three categories: (a) sociodemographic and practice characteristics of PCPs; (b) determining PCPs self-reported knowledge and utilisation of local osteoporosis guidelines; and (c) determining prevalence of barriers to osteoporosis screening and management. Known barriers to screening and management of osteoporosis in primary care in existing literature, as summarised in the introduction, were grouped into categories such as barriers to knowledge of disease, clinician-related barriers, barriers faced by their patients, and barriers arising from systemic factors [23].
The survey instrument was reviewed by a group of seven PCPs of varying seniorities and one specialist in osteoporosis and bone metabolism, who gave feedback on survey content and ease of understanding of the questions. The questions were further reviewed by the study team and subsequently converted to an Internet-based survey. A total of nine PCPs (seven from polyclinics; two from private sector) participated in a pilot survey, where participants had to complete the Internet-based survey twice over a 1-week period (i.e. a second response was submitted on the same survey 1 week after their first response).
Sampling frame and study population
The study population included all PCPs in Singapore. A PCP is one who provides care to the undifferentiated patient, at the point of first contact, providing holistic and personalised care to patients of different age groups [24]. The local primary healthcare system comprises PCPs in public and private sectors. PCPs in the public sector are mainly based in public primary care clinics called polyclinics, which are multi-doctor practices supported by ancillary services. PCPs include ‘family physicians’ with recognised higher qualifications in family medicine approved by the Family Physicians Accreditation Board and registered with the Ministry of Health. Three separate healthcare clusters operate the polyclinics in Singapore. All PCPs of varying designations were eligible to participate, including family medicine residents (trainees), medical officers, resident physicians, family physicians, general practitioners, and locums.
Inclusion and exclusion criteria
Inclusion criteria were a PCP who was engaged in clinical practice. PCPs were excluded if they were not engaged in clinical practice, or if they were specialists who were dually accredited (holding credentials from both the Specialist Accreditation Board and Family Physicians Accreditation Board). All participants had to read and consent to an online participant information sheet prior to proceeding with the study, and data was collected anonymously.
Sample size calculation
The estimated number of all PCPs in Singapore is 3600 [25,26,27]. Based on R Chenot et al. [17], 51.7% of PCPs have good knowledge of osteoporosis guidelines. Using a population size of 3600 and 52% as the proportion of PCPs with good level of osteoporosis management at 5% precision and 95% confidence level, a sample of 347 PCPs would achieve adequate power for this study.
Recruitment procedure and consent process
Recruitment of PCPs was via invitations sent by e-mail and messaging platforms, which contained a URL link to the web-based survey. Invitations were sent through publicity e-mail blasts (for PCPs based in the polyclinics), and through the primary care networks or personal invitations (for PCPs in the private sector). Deemed consent was given through participants reading an online participation information sheet before being allowed to proceed to survey questions.
Administration of web-based survey
The web-based survey was self-administered, and no identifiers were collected. Participants could fill the survey at their own convenience, and there was no time limit imposed. Submission of responses was online, and a CAPTCHA (Completely Automated Public Turing Test to Tell Computers and Humans Apart) test was required before form submission.
Data extraction, data security, data analysis
The web-based survey was hosted on the FormSG platform, a secure end-to-end encrypted form builder for Singapore public servants to create online forms that capture classified data. Data was downloaded and stored on REDCap, a secure web application for managing online surveys and databases. All analyses were performed using IBM SPSS Statistics version 27.0. Demographic differences for the various groups were assessed using Chi-square test or Fisher’s exact test for cell count lesser than 5. Potential factors with p value < 0.2 level were entered into the multiple logistic regression models to identify factors associated with good knowledge and utilisation of guidelines, and confidence in osteoporosis management, respectively. Adjusted odds ratios (OR) along with 95% CI (95%CI) are presented in Table 1 and Appendix Tables 5 and 6. A p value of less than 0.05 was set as statistical significance.
Self-reported knowledge and utilisation of guidelines were categorised into two groups—respondents who selected ‘strongly disagree’, ‘disagree’, or ‘neutral’ as those not reporting good knowledge or utilisation and respondents who selected ‘strongly agree’ and ‘agree’ as reporting good knowledge or utilisation. Responses for confidence in managing osteoporosis were grouped into high or low confidence, with responses of ‘not confident at all’, ‘slightly confident’, or ‘neutral’ in the low confidence group, and responses of ‘quite confident’ or ‘very confident’ in the high confidence group. Barriers to osteoporosis screening and management, when correlated with practice type, were categorised into ‘Barrier’ (responses with ‘agree’ or ‘strongly agree’) and ‘Not a barrier’ (responses with ‘strongly disagree’, ‘disagree’, or ‘neutral’).
Ethics approval and funding
This study was reviewed by the SingHealth Centralised Institutional Review Board (CIRB Ref: 2020/2225) for ethics review under exemption route (anonymous educational tests, surveys, interviews, or observations). The study was also funded by the SingHealth Family Medicine Academic Clinical Programme Seed Grant (PRACPR175811).
Results
After the pilot survey, a basic analysis of the questionnaire’s internal consistency and reliability showed that removal of the question ‘There is a lack of clarity on who is primarily treating my patient’s osteoporosis’ increased the computed Cronbach’s alpha of questions on barriers to osteoporosis screening and management to 0.716. This question was then removed from the final version of the questionnaire. A simple test–retest reliability analysis on questions pertaining to barriers gave an average Kappa of 0.50. The questionnaire was then finalised for use in the main survey.
Sample characteristics
Data collection for main survey began on 18/11/20 and was conducted over a 16-month period.
Of the estimated 1233 PCPs who received the invitation to participate, a total of 347 responded, with response rate of 28.1%. Two respondents were not currently involved in clinical practice, 3 selected other specialty of medicine besides family medicine, 6 were working in Intermediate and Long-term Care Services (ILTC) sector (e.g. nursing homes), and 2 selected government/restructured hospitals. These responses were excluded from analysis.
Table 2 describes the sociodemographic and practice characteristics of 334 PCPs. More respondents were male (55.1%), with more PCPs (54.5%) aged 40 years and above. More PCPs (63.2%) had 10 or more years of clinical practice. 75.7% of PCPs in the sample had postgraduate family medicine qualifications, and 41.0% of PCPs were involved in clinical teaching. One hundred sixty-nine PCPs (50.6%) were from the private sector, and 165 (49.4%) were in the public sector (polyclinics). Two hundred eighty-four PCPs (85.0%) see less than ten patients with osteoporosis in a month. Nineteen PCPs (5.7%) did not have access to BMD testing services by dual-energy X-ray absorptiometry (DXA). Figure 1 shows the types of anti-osteoporosis medications used among PCPs in Singapore. About 18% of PCPs did not use oral bisphosphonates, and subcutaneous teriparatide was not a commonly used medication.
Knowledge and utilisation of local osteoporosis guidelines
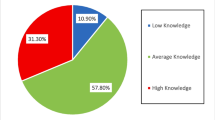
A total of 251 PCPs in the sample (75.1%) reported reading the latest osteoporosis guidelines. Majority of PCPs who had read the guidelines self-reported good knowledge (70.5%) and routinely use or apply the guidelines in practice (74.9%), as seen in Table 2. Majority of PCPs who read the guidelines reported being equipped with knowledge of osteoporosis screening and management.
There were no statistically significant differences between gender, age, duration of practice, highest qualification in family medicine, place of practice, PCP’s number of hours of clinical practice per week, involvement in clinical teaching, and access to BMD testing with self-reported knowledge and utilisation of guidelines (tables shown in Appendix). PCPs who managed 5 to 9 patients with osteoporosis in a month were more likely to self-report good knowledge in osteoporosis guidelines (adjusted OR = 3.67, 95% CI = 1.38–9.80; p = 0.009). The trend is similar for those who saw 10 or more patients with osteoporosis in a month; however, it did not obtain statistical significance.
54.5% of PCPs reported a high degree of confidence in their management of patients with osteoporosis (Table 1). PCPs who were involved in clinical teaching were found to report greater confidence (adjusted OR = 3.40, CI = 1.66–6.94; p = 0.001) in the final model. When compared to the group that managed less than 5 patients with osteoporosis per month, PCPs that managed 5 to 9 patients with osteoporosis per month were 2.5 times more likely to perceive greater confidence in osteoporosis management (adjusted OR = 2.53, 1.39–4.60; p = 0.002). The trend is similar for PCPs who managed 10 or more patients when compared to those who saw less than 5 patients per month (adjusted OR = 2.39, 95% CI = 1.03–5.54; p = 0.042). PCPs who have a place to send patients to perform BMD testing were also more likely to report confidence in osteoporosis management (adjusted OR = 5.30, 95% CI = 1.08–26.12, p = 0.041).
PCPs who read the latest osteoporosis guidelines were more likely to report a higher confidence level in managing osteoporosis when compared with the group that did not (adjusted OR = 8.27, 4.22–16.20; p < 0.001). PCPs who self-reported good knowledge of guidelines (adjusted OR = 5.84, 2.96–11.49; p < 0.001) and good usage of guidelines (adjusted OR = 4.54, 2.21–9.34; p < 0.001) were significantly more confident in managing osteoporosis.
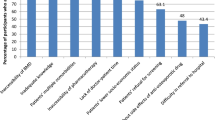
Barriers to osteoporosis screening and management
Figure 2 outlines the prevalence of the barriers to osteoporosis screening among PCPs in Singapore. The top three barriers to screening were (i) their perception that their patients have other medical conditions prioritised (79.3%); (ii) the lack of a national osteoporosis screening programme (68.8%); and (iii) lack of awareness on osteoporosis screening by patients (67%). Figure 3 outlines the barriers to osteoporosis management, with the top three barriers being (i) PCP having limited anti-osteoporosis medications at their place of practice (54.1%); (ii) perception that patients perceive osteoporosis as a condition not requiring treatment (48.5%); and (iii) lack of time to manage osteoporosis (47%). Figures 2 and 3 show the barriers which are ranked in order of prevalence. Barriers related to osteoporosis knowledge did not appear to be common amongst this study population. There was no predominant category of barrier (knowledge of disease, clinician-related, patient-related, or systemic barriers) to osteoporosis screening and management identified.
When compared to PCPs in the polyclinics, more private sector PCPs alluded to the lack of awareness for osteoporosis screening by patients (74% vs 60%; p = 0.007) and cost of BMD testing (53.8% vs 27.3%; p < 0.001) as barriers (Table 3). In contrast, the lack of consultation time to screen osteoporosis was more often cited by polyclinic-based PCPs (70.9% vs 34.3%; p < 0.001).
More polyclinic-based PCPs reported a lack of time in managing osteoporosis compared to those in private practice (66.7% vs 27.8%; p < 0.001). Conversely, more private sector PCPs perceived that patients did not consider osteoporosis as a condition which required treatment (e.g. viewing the disease as a natural part of ageing) (p = 0.016). Other barriers such as cost of BMD testing (p < 0.001) and having financial limitations to prescribe anti-osteoporosis medications (p < 0.001) were more common among PCPs in private practice.
Discussion
Guideline knowledge and utilisation
The proportion of PCPs who had read or used the guidelines appears to be higher than earlier studies conducted in other settings [16,17,18]. Our study showed that 75.1% of PCPs had read or reviewed the latest local osteoporosis guidelines published in 2018. Of those who had read the guidelines, more than 70% self-reported good knowledge and utilisation of it. This could be explained by the ease of access to the guidelines, which are found online. The current easy-to-read format of the clinical practice guidelines, called the appropriate care guides, published by the Ministry of Health, Singapore, are designed to be concise, well-presented, evidence-based recommendations to guide clinical decision-making [9].
Most sociodemographic and practice variables of PCPs did not appear to influence guideline knowledge or utilisation. Nonetheless, the result reveals that those who treated higher numbers of patients with osteoporosis were better acquainted with the guidelines. Chenot et al. reported similar observations among German PCPs [16]. The association could be explained by the need for PCPs to be kept informed of latest guidelines if they encounter many patients with osteoporosis in their practice.
Slightly more than half (54.5%) of respondents rated themselves as quite confident or very confident in the management of patients with osteoporosis. The proportion was similar to a study of PCPs in Israel, where almost half (46%) of respondents self-reported their knowledge of osteoporosis to be adequate or high [28].
The findings in this study highlight the positive influence of clinical guidelines on osteoporosis management by PCPs. The results indicate that having read the clinical practice guidelines and having self-reported good knowledge and utilisation of the guidelines were positively correlated with higher confidence in managing osteoporosis. Guidelines can reach PCPs widely at relatively low cost, imbue them with knowledge and information, and to improve practice and patient health outcomes [29]. A before-and-after study on the implementation of clinical guidelines for other chronic diseases has previously shown improved clinical outcomes in primary care [30]. Furthermore, an epidemiological study in Singapore has postulated that the publication of clinical practice guidelines helped to raise awareness of osteoporosis and was one of the factors accounting for the recent decline in age-standardised incidence of hip fractures rates [5].
More in-depth studies are needed to understand the gaps in guideline knowledge and utilisation, as a quarter of PCPs in the sample had not read or used them. A previous meta-analysis on guideline implementation strategies for chronic diseases in primary care showed that active interventions that go beyond passive distribution of educational material may improve guideline adoption amongst PCPs. These include educational meetings, reminders, or other interactive methods [31]. Interventional studies are needed to assess better dissemination, adoption, and application of osteoporosis guidelines among PCPs.
Barriers to osteoporosis screening and management
The more prevalent barriers to screening, in particular the PCPs’ perception that patients have other conditions prioritised and the lack of awareness of osteoporosis, were similar barriers identified in an Australian study. GPs in Australia perceived a lack of awareness and urgency amongst their patients in treating osteoporosis [12]. Ongoing public education and outreach activities are needed to promote awareness and prevention of the disease. In Singapore, advocacy groups such as the Osteoporosis Society of Singapore, with membership from healthcare professionals and lay members of the public, play a pivotal role in elevating the public awareness of osteoporosis [32].
From an infrastructural perspective, Singapore appeared to be relatively well-resourced, with only 5.7% of PCPs in the sample not having access to BMD (by DXA) services. This is in tandem with earlier statistics in 2013 that DXA is widely available in Singapore, with 16.9 DXA machines available per one million in population [3]. However, despite the relative accessibility to BMD testing, 68.8% of PCPs cited the absence of a national osteoporosis screening programme as a barrier to screening. One large trial in the UK has shown the benefits and cost-effectiveness of a systematic community-based screening programme for osteoporosis in the reduction of incident hip fracture rates [33, 34]. Singapore currently runs two national cancer screening programmes for women, both of which have experienced relative success [35, 36]. It is foreseeable that similar success can be achieved for a national osteoporosis screening programme in Singapore.
Having limited anti-osteoporosis medications in their practice was cited by 54.1% of the PCPs as the most prevalent barrier to osteoporosis management. In our sample, 18% of PCPs did not use oral bisphosphonates, a first-line and widely available anti-osteoporosis medication in Singapore. A total of 39% of PCPs also reported financial limitations in prescribing, higher than the one-fifth of PCPs in the German study [16]. Given the importance of keeping osteoporosis care affordable and accessible to patients in primary care, subventions for anti-osteoporosis medications could be introduced by policymakers.
The time constraints alluded by local PCPs to screen and manage patients with osteoporosis were also reported by French PCPs [14]. Merle et al. suggested that education and empowerment of patients to initiate discussions of osteoporosis with PCPs would facilitate screening amidst time constraints. A possible measure is to adopt a team-based approach and involve other healthcare professionals in osteoporosis screening, as seen in Table 4. It was found that a self‐referral programme for BMD testing and a nurse‐led intervention in the Canadian primary care setting resulted in an increased number of individuals sent for BMD screening [37].
Systemic barriers to osteoporosis management were more commonly highlighted by private sector PCPs. These included barriers such as cost of BMD testing and financial limitations in prescribing anti-osteoporosis medications. In Singapore, a co-payment health financing scheme called MediSave helps to alleviate the out-of-pocket payment burden for chronic diseases like osteoporosis. However, there is a growing prevalence of chronic diseases, and these conditions require long-term management. Patients seeking primary care at polyclinics have the benefit of government subsidies on medications or investigations, resulting in the polyclinics being a cheaper option than private primary care clinics in the long run. In addition, private clinics may not have the scale or resources required for managing complex patients [38].
The primary care network (PCN) scheme was launched in 2017, which allows private sector PCPs to tap on government funding and administrative support. Participating PCPs are able to benefit from a coordinated team-based model of care and experience better economies of scale for ancillary services (e.g. diabetic retinal photography) [39]. The PCN scheme can potentially be extended to osteoporosis care, such as having subvention for BMD testing or medications for PCPs registered to a PCN. One qualitative study exploring the PCN model in chronic disease management demonstrated the PCN’s ability to achieve the key pillars of primary care, such as comprehensiveness, first contact access, coordination, and care continuity [40]. As such, further research is needed to elucidate the benefits of the PCN scheme in terms of chronic disease outcomes and value-based care and evaluate its potential impact on osteoporosis management in primary care.
Strengths and limitations
Our study had several strengths. To our knowledge, it is one of the first studies to focus on osteoporosis management among PCPs in Singapore. Earlier knowledge, attitude, and perception studies on osteoporosis among healthcare professionals in Singapore involved nurses or a wider group of doctors [41, 42]. Our study did not restrict our PCP sample to just one healthcare organisation or practice type and included an almost even mixture of respondents from the public and private sectors. PCPs from all the three polyclinics clusters participated in the study, minimising any sampling bias. The pilot survey also allowed for fine-tuning of the survey instrument.
We recognise several limitations in our study. First, no identifiers were collected in this web-based survey; hence, there is a remote possibility of the same participant filling in the questionnaire more than once. The questionnaire was self-developed, and has not been fully validated in a local setting. A full validation and reliability pilot study of the survey instrument would have strengthened the questionnaire used. The response rate was low at 28.1%, which is not uncommon for Internet-based surveys [43]. Convenience sampling for private sector PCPs was also used, and this may have led to selection bias. The anonymous Internet-based questionnaire platform may introduce response bias. Our study dealt with self-reported knowledge of osteoporosis guidelines. Social desirability bias may occur when PCPs over-estimate their knowledge of osteoporosis guidelines or their confidence in osteoporosis management.
Conclusion
This study has shown that the majority of PCPs in Singapore know and use the local osteoporosis guidelines and demonstrate a positive correlation between their knowledge/usage and their confidence in osteoporosis management. Clinical practice guidelines can be a useful tool to address knowledge gaps and facilitate osteoporosis management amongst PCPs. However, enhanced systemic support and team-based approach in managing patients with osteoporosis can potentially address the current barriers. Strategies are needed by professional bodies and policymakers for effective guidelines adoption and implementation in the local primary healthcare ecosystem.
Change history
21 June 2023
A Correction to this paper has been published: https://doi.org/10.1007/s11657-023-01299-7
References
Consensus development conference (1991) prophylaxis and treatment of osteoporosis. Am J Med 90(1):107–110
World Health Organization (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. WHO technical report series, 843:1–129
Mithal A, Ebeling P, Kyer CS (2013) The Asia-Pacific Regional Audit: Epidemiology, costs & burden of osteoporosis in 2013. International Osteoporosis Foundation. https://www.osteoporosis.foundation/sites/iofbonehealth/files/2019-06/2013_Asia_Pacific_Audit_English.pdf. Accessed 30 August 2022
Koh LK, Saw SM, Lee JJ, Leong KH, Lee J, National Working Committee on Osteoporosis (2001) Hip fracture incidence rates in Singapore 1991–1998. Osteoporos Int 12(4):311–318
Yong EL, Ganesan G, Kramer MS et al (2019) Hip fractures in Singapore: ethnic differences and temporal trends in the new millennium. Osteoporos Int 30(4):879–886
Lau TC (2018) Role of GP in osteoporosis management. Singap Fam Phys 44(3):36–38
Agency for Care Effectiveness (2018) Appropriate care guide – osteoporosis: identification and management in primary care. Ministry of Health, Republic of Singapore. www.ace-hta.gov.sg. Accessed 11 Jan 2019
The Royal Australian College of General Practitioners and Osteoporosis Australia (2017) Osteoporosis prevention, diagnosis and management in postmenopausal women and men over 50 years of age, 2nd edn. RACGP, East Melbourne
https://www.ace-hta.gov.sg/resources/process-methods. Accessed 24 May 2022
Koh LK, Sedrine WB, Torralba TP et al (2001) A simple tool to identify Asian women at increased risk of osteoporosis. Osteoporos Int 12(8):699–705
Gupta ED, Goh EM, Gun SC et al (2013) Osteoporosis awareness among primary care physicians in Malaysia. EXCLI J 12:521–522
Naik-Panvelkar P, Norman S, Elgebaly Z et al (2020) Osteoporosis management in Australian general practice: an analysis of current osteoporosis treatment patterns and gaps in practice. BMC Fam Pract 21(1):32
Mendis AS, Ganda K, Seibel MJ (2017) Barriers to secondary fracture prevention in primary care. Osteoporos Int 28(10):2913–2919
Merle B, Haesebaert J, Bedouet A et al (2019) Osteoporosis prevention: where are the barriers to improvement in French general practitioners? A qualitative study. PLOS ONE 14(7):e0219681
Jaglal SB, Carroll J, Hawker G et al (2003) How are family physicians managing osteoporosis? Qualitative study of their experiences and educational needs. Can Fam Physician 49:462–468
Chenot R, Scheidt-Nave C, Gabler S, Kochen MM, Himmel W (2007) German primary care doctors’ awareness of osteoporosis and knowledge of national guidelines. Exp Clin Endocrinol Diabetes 115:584–589
McKechnie DA, Pather MK (2008) Awareness and perceptions of published osteoporosis clinical guidelines - a survey of primary care practitioners in the Cape Town metropolitan area. SA Fam Pract 50(4):71
Mahdaviazad H, Keshtkar V, Emami MJ (2018) Osteoporosis guideline awareness among Iranian family physicians: results of a knowledge, attitudes, and practices survey. Prim Health Care Res Dev 19(5):485–491
Tan MZ, Bee CS, Chandran M (2012) A review of the 2008 Singapore Ministry of Health Clinical Practice Guidelines on osteoporosis and an update. J ASEAN Fed Endocr Soc 27(2):159–169
Suresh E, Pazianas M, Abrahamsen B (2014) Safety issues with bisphosphonate therapy for osteoporosis. Rheumatology (Oxford) 53(1):19–31
Simonelli C, Killeen K, Mehle S, Swanson L (2002) Barriers to osteoporosis identification and treatment among primary care physicians and orthopedic surgeons. Mayo Clin Proc 77(4):334–338
Blazkova S, Vytrisalova M, Palicka V et al (2010) Osteoporosis risk assessment and management in primary care: focus on quantity and quality. J Eval Clin Pract 16(6):1176–1182
Green LA (2004) The research domain of family medicine. Ann Fam Med 2(Suppl 2):S23–S29
https://www.moh.gov.sg/home/our-healthcare-system/healthcare-services-and-facilities/primary-healthcare-services. Accessed 24 April 2021
Primary Care Survey (2014) Health information division. Ministry of Health, Singapore
https://tablebuilder.singstat.gov.sg/table/TS/M870011. Department of Statistics, Singapore. Accessed 13 June 2020
Singapore Medical Council. Annual Report 2018
Fogelman Y, Goldshtein I, Segal E, Ish-Shalom (2016) Managing osteoporosis: a survey of knowledge, attitudes and practices among primary care physicians in Israel. PLoS ONE 11(8):e0160661
Giguère A, Zomahoun HT, Carmichael P-H et al (2020) Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews 8: CD004398. https://doi.org/10.1002/14651858.CD004398.pub4
Lesho EP, Myers CP, Ott M, Winslow C, Brown JE (2005) Do clinical practice guidelines improve processes or outcomes in primary care? Mil Med 170(3):243–246
Kovacs E, Strobl R, Phillips A et al (2018) Systematic review and meta-analysis of the effectiveness of implementation strategies for non-communicable disease guidelines in primary health care. J Gen Intern Med 33(7):1142–1154
https://themeetinglab.eventsair.com/osteoporosis/membership. Accessed 29 August 2022
Shepstone L, Lenaghan E, Cooper C et al (2018) Screening in the community to reduce fractures in older women (SCOOP): a randomised controlled trial. Lancet 391(10122):741–747
Söreskog E, Borgström F, Shepstone L et al (2020) Long-term cost-effectiveness of screening for fracture risk in a UK primary care setting: the SCOOP study. Osteoporos Int 31(8):1499–1506
Jin AZ, Louange EC, Chow KY, Fock CW (2013) Evaluation of the national cervical cancer screening programme in Singapore. Singap Med J 54(2):96–101
Chootipongchaivat S, Wong XY, ten Haaf K et al (2021) Cost-effectiveness analysis of breast cancer screening using mammography in Singapore: a modelling study. Cancer Epidemiol Biomark Prev 30(4):653–660
MacIntyre J, Drake P, Garland-BairdL, et al (2019) Optimizing osteoporosis care in a rural primary health care center: Findings of a research study aimed to support seniors. Nurs Forum 54(4):611–618
Tan CC, Lam CSP, Matchar DB, Zee YK, Wong JEL (2021) Singapore’s health-care system: key features, challenges, and shifts. Lancet 398(10305):1091–1104
https://www.primarycarepages.sg/practice-management/primary-care-model/primary-care-network-(pcn). Accessed 26 May 2021
Foo CD, Surendran S, Jimenez G et al (2021) Primary care networks and starfield’s 4Cs: a case for enhanced chronic disease management. Int J Environ Res Public Health 18(6):2926
Korthoewer D, Chandran M (2012) Osteoporosis management and the utilization of FRAX®: a survey amongst health care professionals of the Asia-Pacific. Arch Osteoporosis 7(1–2):193–200
Zhang RF, Chandran M (2011) Knowledge of osteoporosis and its related risk factors among nursing professionals. Singap Med J 52(3):158–162
Braithwaite D, Emery J, de Lusignan S, Sutton S (2003) Using the Internet to conduct surveys of health professionals: a valid alternative? Fam Pract 20(5):545–551
Acknowledgements
The authors are grateful to all colleagues who assisted with reviewing the survey instrument and colleagues from SingHealth Polyclinics and Family Medicine Academic Clinical Programme for their support in this study. The authors wish to thank all PCPs who participated in the study.
Funding
This study was funded by SingHealth Family Medicine Academic Clinical Programme Seed Grant (PRACPR175811).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the SingHealth Centralised Institutional Review Board (CIRB Ref: 2020/2225).
Consent to participate
Participants gave their consent to participate by reading and agreeing to an online participation information sheet before proceeding to the survey.
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised:
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Choong, D.S., Tan, N.C., Koh, Y.L.E. et al. Osteoporosis management by primary care physicians in Singapore: a survey on osteoporosis guidelines utilisation and barriers to care. Arch Osteoporos 18, 72 (2023). https://doi.org/10.1007/s11657-023-01283-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-023-01283-1