Abstract
The sudden failure of a previously healthy and functioning liver is a dramatic and devastating event. Acute liver failure is the common final pathway of a multitude of conditions and insults, all of which result in massive hepatic necrosis or loss of normal hepatic function. The ensuing multiorgan system failure frequently has a fatal outcome, with mortality rates in most series ranging from approximately 55% to 95% [1]. Acute liver failure (ALF, previously often referred to as fulminant hepatic failure (FHF)) knows no age boundaries, with many cases occurring in those younger than 30 years. Short of excellent intensive care unit (ICU) support and liver transplantation in selected cases, few viable treatment options are available. Over the past few decades, however, survival has been improved by anticipation, recognition, and early treatment of associated complications, as well as the application of prognostic criteria for early identification of patients requiring liver transplantation (along with improvement in the techniques and science of transplantation itself). The etiology of ALF varies from country to country and the incidence change over time. Paracetamol (acetaminophen) has now replaced viral hepatitis as the leading cause of ALF [2]. In a study from London including 310 patients with ALF in the period 1994–2004, 42% of the cases were caused by paracetamol [3], whereas this was only the cause in 2% of 267 patients in Spain from 1992 to 2000 [4]. However, less than 10% of all liver transplants are performed in patients with ALF [5, 6].
This is an update of a chapter originally written by Thomas Riley and Amit Sadana for the first edition of this book.
You have full access to this open access chapter, Download reference work entry PDF
Similar content being viewed by others
The sudden failure of a previously healthy and functioning liver is a dramatic and devastating event. Acute liver failure is the common final pathway of a multitude of conditions and insults, all of which result in massive hepatic necrosis or loss of normal hepatic function. The ensuing multiorgan system failure frequently has a fatal outcome, with mortality rates in most series ranging from approximately 55% to 95% [1]. Acute liver failure (ALF, previously often referred to as fulminant hepatic failure (FHF)) knows no age boundaries, with many cases occurring in those younger than 30 years. Short of excellent intensive care unit (ICU) support and liver transplantation in selected cases, few viable treatment options are available. Over the past few decades, however, survival has been improved by anticipation, recognition, and early treatment of associated complications, as well as the application of prognostic criteria for early identification of patients requiring liver transplantation (along with improvement in the techniques and science of transplantation itself). The etiology of ALF varies from country to country and the incidence change over time. Paracetamol (acetaminophen ) has now replaced viral hepatitis as the leading cause of ALF [2]. In a study from London including 310 patients with ALF in the period 1994–2004, 42% of the cases were caused by paracetamol [3], whereas this was only the cause in 2% of 267 patients in Spain from 1992 to 2000 [4]. However, less than 10% of all liver transplants are performed in patients with ALF [5, 6].
The aim of this chapter is to help clinicians recognize the presentation and clinical features of drug- or chemical-induced ALF or liver injury, anticipate and appropriately manage the complications of ALF, and recognize the indications for timely referral for orthotopic liver transplantation (OLT). The pathophysiology, differential diagnosis, appropriate laboratory testing in the evaluation and treatment of ALF, and specific therapies available for certain etiologies of ALF will also be discussed. Current and future trends in liver transplantation will be described.
Definitions
In 1986, Bernuau and colleagues [7] suggested that the term “fulminant hepatic failure ” (FHF) should be applied to patients in whom encephalopathy developed within 2 weeks of the onset of jaundice and that subfulminant hepatic failure be applied to those in whom this interval was 2–12 weeks. In 1993, O’Grady and associates [8] proposed the terms hyperacute, acute, and subacute liver failure based on whether the interval between the appearance of encephalopathy and jaundice was 0–7 days, 8–28 days, or 29 days to 12 weeks, respectively. Both Bernuau and O’Grady included cases of preexisting asymptomatic chronic liver conditions. In Japan, patients with fulminant hepatitis are classified into two types according to the onset of encephalopathy (before or after 10 days). Encephalopathy occurring after 8 weeks is defined as late-onset hepatic failure (LOHF) [9].
These classification systems reflect important differences in the clinical course and prognosis observed between patient subgroups, thus facilitating earlier diagnosis and timely referral for OLT. For example, both the hyperacute and acute liver failure groups have a high incidence of cerebral edema. However, whereas patients in the hyperacute group are more likely to survive with medical management, patients in the acute liver failure group tend to die without liver transplantation [8]. The subacute failure group has a lower incidence of cerebral edema and a higher incidence of portal hypertension manifestations, including ascites and renal failure [8]. Mortality in this group remains high. O’Grady and colleagues found that the hyperacute failure group had a 36% survival rate, as opposed to 7% and 14% in the acute and subacute failure cohorts, respectively [8]. Bernuau and coworkers also noted that those with the most rapid onset of encephalopathy had the best chance of survival [7]. Similar observations have been made in Japan [9]. However, it is important to note that although the interval between the onset of encephalopathy and jaundice was of prognostic significance in O’Grady’s cohort [1], it was not an independent prognostic factor in Bernuau’s cohort [10], thus raising doubts about its universal applicability. Application of the O’Grady classification to 423 prospectively studied patients from a tertiary care referral center in northern India failed to yield any prognostic differences between the groups [11].
Although these classifications may be useful in highlighting differences in clinical course and prognosis among patient subgroups, the contribution of other independent prognostic indicators (etiology of ALF, patient age, prothrombin time, factor V level, renal function, mental status) should not be overlooked. Table 1 provides a summary of the various definitions of liver failure.
Pathogenesis
Measuring about 1500 mL in volume, the liver is the second largest organ in the body and plays a critical role in its homeostasis. At no time is this role more apparent than during an episode of acute injury. Derangements in synthetic function (hypoalbuminemia, decreased levels of clotting factors), gluconeogenesis (hypoglycemia), drug and toxicant metabolism (sensitivity to narcotics and benzodiazepines, hyperammonemia), excretory function (hyperbilirubinemia), temperature regulation (hypothermia), and central nervous system function (encephalopathy) are the result of liver failure. Some of these parameters are used as prognostic factors and markers of severity of injury.
The exact mechanisms of injury and impairment in hepatocellular function that lead to ALF are poorly understood. Loss of integrity of the hepatocyte plasma membrane secondary to chemical, immunologic, or a wide variety of other insults is thought to represent the final common pathway that leads to cell necrosis and ALF [13, 14]. Damage to the cell membrane permits leakage of enzymes, coenzymes, and electrolytes from the cytosol, followed by an influx of calcium ions, which eventually results in cell death. The importance of calcium is underscored by the finding that normally vulnerable hepatocytes in vitro do not succumb to the cytotoxic effects of membrane-active toxins when calcium ions are not included in the culture medium [15].
New information is emerging on the role of growth factors and the inflammatory cascade in ALF. Transforming growth factor-β1 (TGF-β1) has been identified as exerting an inhibitory effect on hepatic regeneration, with its effects being counteracted by hepatocyte growth factor (HGF). ALF patients with viral hepatitis have demonstrated an increase in total TGF-β1 with a less elevated HGF level, thus suggesting an imbalance in growth factor interplay as a cause of impaired hepatic regeneration [16]. This mechanism has also been suggested by research performed in posttransplant patients [17]. Studies suggest that activation of the cytokine network may represent the common final pathway for the development of ALF [18]. Although multiple inflammatory cascades come into play, interleukin-1 , interleukin-6 , and tumor necrosis factor-α have been identified as the more important mediators, along with endotoxin and nitric oxide. In response to the initial hepatic insult, interplay among these mediators sets into motion a vicious self-perpetuating cycle resulting in continued hepatic injury and multiorgan failure. Furthermore, higher levels of circulating interleukin-8 and interferon-γ have been demonstrated in patients with ALF than in healthy volunteers and those with chronic liver disease, thus suggesting a pathogenic role in acute hepatic injury. Although no relationship was found between the levels of these two markers and the clinical course, elevated levels of interleukin-10 were found to be predictive of improved outcome [19].
Etiology and Differential Diagnosis
Careful diagnostic evaluation is important because the etiology can have prognostic implications (e.g., the prognosis is worse with Wilson’s disease and idiosyncratic drug reactions, better with viral- and acetaminophen-induced ALF), influence treatment options (e.g., N-acetylcysteine [NAC] for ALF induced by acetaminophen [acetyl-para-aminophenol or paracetamol]), and indicate the need for genetic testing of family members (e.g., Wilson’s disease) [20]. Etiologies of ALF can be divided into toxic and nontoxic. Toxic causes include pharmaceuticals, drugs of abuse, chemicals, and biologic agents. Nontoxic causes include, but are not limited to, infections, ischemia, metabolic derangements, malignancy, autoimmune problems, and primary graft failure after liver transplantation . Because ALF represents the common final pathway of injury, it is difficult to differentiate between the aforementioned causes based solely on clinical presentation and disease progression. A detailed patient history is invaluable, and a multitude of helpful diagnostic testing tools are available to help uncover the etiology of ALF in the majority of cases (Table 2).
Frequency of Causes
Although the frequency varies geographically, the most common causes of ALF remain viral and drug-induced hepatitis. In the USA, drug-induced liver injury is responsible for almost 50% of ALF [21, 22] most often caused by APAP. In London, UK, APAP poisoning was responsible for 57% of ALF cases seen at King’s College Hospital between 1973 and 1991, whereas in France, APAP was identified as the etiology in only 2% of ALF cases between 1972 and 1990 [23, 24]. A multicenter study from the USA of 295 patients in whom ALF was diagnosed between 1994 and 1996 found that the most common etiologies were APAP (20%), viral hepatitis (10% hepatitis B, 7% hepatitis A), cryptogenic (15%), and drug reactions (12%) [25]. Outside of the USA and Europe, drugs are less likely to cause ALF. In a Japanese study [26], the percentage of drug allergy-induced ALF in 432 patients collected in the period 1998–2006 was 2% in contrast to viral infection which was diagnosed as the cause in 16% of the patients (13% with hepatitis B). Even though APAP overdose was found to represent one-sixth of all causes of ALF leading to registration for liver t ransplantation in Europe, there was a 50-fold difference in the relative risk of ALF leading to registration for liver transplantation between countries with a low incident rate (e.g., Italy with 0.03 ALF per million inhabitants per year) and high incident rate (e.g., Ireland with 7.13 ALF per million inhabitants per year). The reasons for these differences remain unclear, but may be related to national differences in pack size restriction of APAP or antidote treatment regimens [27].
Toxic Causes
Pharmaceuticals
Hepatotoxicity can result from therapeutic or toxic doses of many medications by a multitude of mechanisms. It can be manifested as asymptomatic elevations of liver enzymes, but some cases can progress to ALF. Hepatocyte injury can occur directly from disruption of intracellular function or membrane integrity or indirectly from immune-mediated membrane disruption. Drugs can also cause cholestasis, steatosis, idiosyncratic reactions, fibrosis, veno-occlusive disease, vasculitis, and granulomatous reactions. Categorization of these toxic reactions suggests the type and duration of exposure.
Acute APAP overdose (both deliberate and unintentional/supratherapeutic ingestion) remains one of the most common causes of ALF in the USA and UK (see Chap. 59, “Acetaminophen/ Paracetamol ”). The maximum daily approved dose may vary depending on the country, but is generally in the range of 80 mg/kg APAP for children and 3–4 g for adults. The minimum dose for toxicity from a single ingestion is generally 150 mg/kg for children and 7.5–10 g for adults [28]. Doses greater than 350 mg/kg almost always result in severe hepatotoxicity without antidotal treatment [23]. However, APAP toxicity is increasingly being recognized as a cause of ALF even when used in supratherapeutic doses, and such “therapeutic misadventures” may represent the most common cause of ALF in the USA [29]. These cases usually occur when APAP is misused in the setting of chronic pain and alcohol use or less commonly with medications that induce the cytochrome P-450 system (e.g., isoniazid [INH], rifampin, phenytoin) or in the setting of starvation (depleted glutathione [GSH] stores) [30, 31]. High aminotransferase levels are typical of such cases, with values usually peaking above 4000 U/L and sometimes above 10,000 U/L.
The metabolic activation of certain drugs by the liver into hepatotoxic intermediates is an important phenomenon in drug-induced ALF. The resultant toxic metabolites covalently bind to important macromolecular constituents of the cell and prevent normal functioning or cause necrosis of the cell. Acetaminophen metabolism (Fig. 1) serves as a pertinent example. Most of the ingested APAP is conjugated with glucuronide or sulfate and excreted as a harmless metabolite [32, 33]. In therapeutic doses, approximately 5% of APAP is oxidized by the P-450 system to N-acetyl-p-benzoquinoneimine (NAPQI), a toxic intermediate that is readily detoxified by reaction with GSH [32, 33]. An APAP overdose overwhelms the sulfation and glucuronidation pathways and drives the formation of NAPQI, detoxification of which depletes GSH stores [32, 33]. Once the binding capacity of GSH is exceeded, NAPQI covalently binds to key hepatocyte membrane and cellular proteins and causes necrosis [22, 23].
Concurrent use of certain medications can further amplify the production of hepatotoxic intermediates by induction of the cytochrome family responsible for metabolism of the parent drug. For example, alcohol [34], INH [35], and possibly phenytoin [36] cause induction of the P-450 system, which enhances the conversion of APAP to NAPQI. In addition, alcohol inhibits the synthesis of GSH, thereby decreasing clearance of NAPQI [37]. Chronic alcohol abusers are also more likely to be malnourished and have an antecedent fasting period, which also depletes GSH stores. Thus, supratherapeutic doses of APAP in conjunction with regular alcohol use can result in elevated NAPQI levels and subsequent hepatic injury – the so-called therapeutic misadventure [38]. It is important to note that starvation, a GSH-depleted state, is an independent risk factor for a therapeutic misadventure with APAP, regardless of concurrent alcohol use. Another example of synergistic toxicity is noted in patients treated with INH and rifampin, where rifampin-induced cytochrome induction can potentiate INH hepatotoxicity [39].
Whereas APAP-induced injury is predictable and dose dependent, other drugs (e.g., valproic acid , troglitazone, amiodarone) can cause rare idiosyncratic and unpredictable hepatotoxic effects. Hypersensitivity reactions can occur with the use of phenytoin , para-aminosalicylate, chlorpromazine, and sulfonamides, with catastrophic results. Idiosyncratic reactions do not exhibit dose-related toxicity, and some can result in ALF with a single dose. They occur in a small fraction of susceptible individuals and are unpredictable. Patients with chronic liver disease may be at increased risk for such reactions. The formation of immunologically stimulating drug-protein complexes (neoantigens) with a resultant “innocent bystander” effect is thought to be one of the pathogenic mechanisms of injury [40].
The halogenated anesthetics enflurane, methoxyflurane, and isoflurane have uncommonly been associated with the development of toxic hepatitis, but hepatic failure is rare. They usually develop after multiple exposures to these agents and are thought to be of combined toxic and allergic origin. Nonsteroidal anti-inflammatory drugs, especially sulindac and diclofenac, have also been known to cause liver disease, with an incidence of 1.1–3.7 cases per 100,000 prescriptions [41]. The macrolide antibiotics erythromycin and clarithromycin are rare causes of hepatic failure that exhibit primarily cholestasis on biopsy and, uncommonly, hepatic necrosis [42].
In a nationwide prospective study [43], the incidence of drug-induced liver injury (DILI) was investigated in a population-based cohort in Iceland. The most commonly implicated agent over the 2-year study period was amoxicillin-clavulanate with a rate of 43 DILI cases per 100,000 inhabitants. The highest risk of hepatotoxicity was associated with the use of azathioprin (752 DILI cases per 100,000 inhabitants) and infliximab (675 DILI cases per 100,000 inhabitants).
Tetracycline demonstrates yet another mechanism of hepatotoxicity. It is known to bind hepatocyte tRNA and impair apoprotein synthesis, thereby causing triglyceride buildup in the liver. It may also cause concurrent derangements in fatty acid uptake, formation, and oxidation by hepatocytes, which can culminate in the loss of hepatic function secondary to acute microvesicular fatty infiltration [44]. Aspirin, valproic acid , amiodarone, and zidovudine are also known to cause microvesicular steatosis .
Herbal Medications
Widespread use of herbal remedies in Europe and their ever-growing popularity in the USA have brought to light many case reports of associated hepatotoxicity . Herbals and alternative medications implicated include chaparral , gentian, germander , and senna, but they rarely result in liver failure [45]. However, in 2001 and 2002 two case reports suggesting a causal relationship between kava (a herbal supplement used for the treatment of anxiety) and ALF requiring transplantation were published [46, 47]. Twenty-four other reports of kava-related hepatotoxicity have led to a ban on kava in Switzerland and Germany. The US Food and Drug Administration (FDA) currently has the supplement on so-called MedWatch alert status. Although virtually any drug can cause acute liver injury, more common examples are listed in Table 3.
Drugs of Abuse
Severe liver injury and even hepatic failure can result from recreational drug use, including abuse of cocaine, 3,4-methylenedioxymethamphetamine (MDMA or Ecstasy), and phencyclidine, or from recreational inhalation of solvents containing toluene or trichloroethylene [48]. Hepatic failure in these cases may be the result of liver ischemia, hypoxemia, severe hyperpyrexia, rhabdomyolysis, and/or direct hepatotoxic effect.
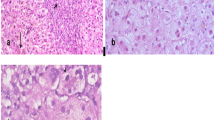
In addition to these effects, cocaine’s hepatotoxicity is thought to be due primarily to ischemia from systemic arterial vasospasm and congestive heart failure, complicated by the occurrence of disseminated intravascular coagulation (DIC) and renal failure . The histologic pattern is both centrilobular necrosis and microvesicular steatosis . MDMA causes a syndrome similar to that of cocaine: hyperthermia, DIC, and rhabdomyolysis, complicated further by dehydration and acute renal failure. Toxic hepatitis may be immediate or delayed, and the histopathology is characterized by central and midzonal necrosis or by steatosis and eosinophilic infiltration [48]. The latter suggests an immune mechanism of MDMA hepatotoxicity , and liver transplantation has been required in some cases [49].
Chemicals
Industrial exposure to cleaning solvents containing fluorinated or halogenated hydrocarbons is a well-documented cause of hepatic necrosis, fatty infiltration, and, ultimately, ALF. Carbon tetrachloride ’s hepatotoxic effects, noted in the 1920s–1940s, led to its abandonment as an anesthetic and anthelmintic by the FDA, but it is still used in the production of solvents, refrigerants, and aerosol propellants. The fluorinated hydrocarbon chloroform, a potent central nervous system depressant once used as an anesthetic, has also been banned by the FDA because of its hepatotoxicity, but it is still found in industrial use.
Biologic Agents
Hepatotoxicity secondary to accidental ingestion of poisonous mushrooms has been on the rise because of popular interest in gathering and eating uncultivated mushrooms [50]. An increase in the incidence of mushroom poisoning is usually seen after periods of heavy rainfall or during the fall, when the conditions for growth are optimal. Ingestion of cyclopeptide-containing mushrooms accounts for up to 90% of mushroom-related deaths worldwide [50–54]. The genus Amanita is the source of most of these poisonings, especially A. phalloides (death cap), A. verna (death angel), and A. virosa (destroying angel). Galerina and Lepiota species can also be hepatotoxic (see Table 2). Amanita species are found primarily in the temperate coastal regions of the west coast of the USA, but they have also adapted to the mid-Atlantic coast and the northeast. A. phalloides is the predominant hepatotoxic European mushroom. The mushroom itself has no distinct taste, smell, or appearance. Ingestion is usually followed 6–12 h later by fever, nausea, vomiting, and severe diarrhea. Renal and hepatic impairment may become evident by 24–48 h while the patient appears to be recovering clinically. However, renal failure and hepatic failure progress and tend to become severe by day 3–5, with the development of jaundice, encephalopathy, and possibly death. Liver transplantation has been carried out successfully for cases of severe Amanita poisoning [53]. Some Amanita mushrooms such as A. muscaria and A. pantherina do not contain hepatotoxins.
The cyclopeptide mushrooms contain two cyclic oligopeptide hepatotoxins: phallotoxins and amatoxins . Both are heat stable and resistant to drying [52, 54]. Phallotoxins are not absorbed from the gastrointestinal (GI) tract and therefore are not thought to play a role in the symptoms associated with human poisoning [55]. α-Amanitin is a dialyzable octapeptide that inhibits RNA polymerase II, thus interfering with mRNA synthesis [56]. The cell is robbed of its ability to produce vital structural proteins and undergoes necrosis. Tissues with a high rate of protein synthesis (liver, kidneys, brain) suffer the most damage [56]. α-Amanitin is easily absorbed from the intestinal epithelium and enters the hepatocyte via bile transport carriers [57]. It demonstrates low plasma protein binding and is cleared from plasma in 36 h [56, 57]. Sixty percent is excreted into bile and undergoes enterohepatic circulation, whereas the rest is cleared renally [55, 56] (see Chap. 108, “Ccms: The Deadly Amanitas” for a more detailed discussion).
Case reports of ALF caused by other noninfectious biologic agents include one published in 1994 describing ALF secondary to a sea anemone sting [58].
Nontoxic Causes
Infections
Viral hepatitis remains one of the most common causes of ALF worldwide. The majority of cases are related to hepatitis A and E infections globally with death rates of more than 50% reported from the developing world [59, 60]. Also hepatitis B infection may lead to ALF [61]. It is unclear why ALF develops in a select proportion of the infected population, but historical review of previous epidemics reveals that this number remains surprisingly constant at approximately 0.4% [62]. The hepatocellular necrosis seen in cases of ALF caused by hepatitis A and B is thought to be due in part to a direct cytopathic effect of the virus. This mechanism is supported by the relative lack of inflammation seen in the livers of patients with viral ALF. However, the normal humoral and cell-mediated response to a massively infected liver also plays a role. One study found that the amount of hepatitis A virus (HAV) isolated from the livers of patients with HAV-associated ALF was higher than titers from patients with nonfulminant HAV hepatitis [63]. In addition, CD8+ T lymphocytes isolated from the livers of two patients with acute HAV infection demonstrated the ability to kill HAV-infected fibroblasts in culture, thus implying that the liver damage seen in virally induced ALF is in part cell mediated [64].
ALF secondary to HAV infection is a rare event: 0.35% of HAV infections will progress to ALF [58]. Patients have a comparatively low mortality rate (<40%) and usually recover without liver transplantation . Acute hepatitis B infection progresses to ALF in approximately 1% of infected patients, thus making hepatitis B virus (HBV) the most common viral cause of ALF [58]. Its role may be underestimated when the impact of infection with a pre-core mutant (HBV viral infection that does not produce the surface [HBsAg] or e antigen) is taken into account, as demonstrated by a study in which it was found that 35% of patients who underwent transplantation for non-A, non-B hepatitis had evidence of HBV infection by polymerase chain reaction [65]. One half to one third of patients with ALF secondary to HBV will clear HBsAg within a few days [66]; such rapid clearance is thought to be the result of a substantial immunologic response to HBV-laden hepatocytes. Interestingly, those who clear HBsAg rapidly have a more favorable prognosis (47% survival rate) than those with continued HBsAg positivity (17% survival rate) [13]. Despite being an increasingly common cause of chronic liver disease, isolated infection with hepatitis C virus has yet to be definitively implicated in ALF [10]. Though rarely encountered in the USA, infection with hepatitis E virus in pregnant women carries a 40% mortality rate [67]. Infection with hepatitis delta virus has been implicated in about 30% of HBV-related ALF cases. In fact, the risk of ALF increases dramatically with any hepatitis virus coinfection [68, 69].
Infection with the viruses herpes simplex, Epstein–Barr, varicella zoster, cytomegalovirus, or parvoviruses occasionally causes ALF, though usually in an immunocompromised setting. Pediatric ALF in association with parvovirus B19 infection has been noted.
Case reports detailing other (rare) infectious causes of ALF have implicated Coxiella burnetii, Plasmodium falciparum, amebic abscesses, disseminated tuberculosis, and Bacillus cereus emetic toxin as causative agents.
Vascular Events
The liver has a unique blood supply, with the portal vein supplying 70% of total blood flow and the hepatic artery making up the remaining 30%. Disruption of either the inflow or outflow of blood can lead to ischemia, hypoxia, and ultimately ALF. Examples include prolonged hypotension (intraoperative circulatory collapse, acute myocardial infarction, acute pulmonary embolism), gram-negative sepsis and shock, congestive heart failure, veno-occlusive disease (chemotherapy- or bone marrow transplant related), Budd–Chiari syndrome, and hepatic artery thrombosis after OLT. Prolonged hypotension after an overdose of opiates or cardioactive drugs (e.g., β-receptor or calcium channel antagonists) or cardiac arrest from any agent may also produce hepatic failure. It is important to note that almost all cases of hepatic ischemia secondary to systemic hypotension are associated with very high aminotransferase levels and accompanying renal dysfunction. In contrast, patients with Budd–Chiari syndrome have aminotransferase levels between 100 and 600 U/L, although higher values are possible. Serum alkaline phosphatase is around 300–400 U/L, whereas bilirubin is usually less than 7 mg/dL (120 μmol/L) at onset. The disease commonly affects women and causes severe right upper quadrant pain and hepatomegaly.
Exertional heatstroke is also an important cause of ischemic ALF and is usually seen in young unconditioned patients pursuing a new exercise program in high ambient temperature and humidity. Classic (nonexertional) heatstroke occurs in patients with multiple chronic medical problems or those taking anticholinergic medications, which leaves them susceptible to disruption of temperature regulatory mechanisms or incapable of escaping the heat. Heatstroke is usually manifested by hyperthermia (core body temperature >40.5 °C [104.9 °F]), mental status changes (including seizures), peripheral vasodilation, and a host of metabolic derangements. Leukocytosis may also be a prominent initial feature. Acute mortality was 21% in one series [70]. Adverse drug effects (e.g., neuroleptic malignant syndrome, veno-occlusive disease) can play a role in ischemic ALF . Disruption of sinusoidal blood flow by metastatic cancer has also been described as a cause of ALF. Gastric, breast, and oat cell carcinomas have been implicated, as have leukemia, carcinoid syndrome, and amyloidosis.
Metabolic and Other Causes
ALF can occur even without large-scale hepatic necrosis, as demonstrated by patients who suffer from liver failure secondary to acute fatty liver of pregnancy (AFLP), Reye’s syndrome, or a fulminant manifestation of Wilson’s disease . ALF as an initial feature of Wilson’s disease is rare but carries a very high mortality rate without liver transplantation. A relatively low serum alkaline phosphatase level and a disproportionately elevated bilirubin level (up to 30 mg/dL [513 μmol/L]) characterize such a manifestation. The serum copper level is usually elevated.
Whereas loss of hepatocyte function in Wilson’s disease is secondary to hepatic copper overload, AFLP results in ALF from an inherited defect in mitochondrial beta oxidation of long-chain fatty acids [71]. AFLP usually occurs in the third trimester and may be associated with preeclampsia. Serum aminotransferase levels usually stay below 1000 U/L unless the HELLP syndrome (hemolytic anemia, elevated liver function tests [LFTs], and low platelet count) is present. Infant mortality is high in either case.
Reye’s syndrome has a similar pathogenesis and can be seen in pediatric cases with an antecedent viral illness treated with aspirin. Other rare metabolic anomalies that can cause ALF are listed in Table 2. Rarely, autoimmune hepatitis and primary graft failure after liver transplantation will be manifested as ALF.
Diagnosis and Complications
ALF is the common final pathway of a variety of insults, and thus the features remain remarkably similar regardless of the etiology. Nonspecific flu-like symptoms, including fatigue, nausea, loss of appetite, and malaise, are the initial symptoms in previously healthy patients. These symptoms are followed by jaundice and then alteration of mental status with rapid progression to coma. Other helpful signs on physical examination include decreased or absent dullness to percussion in the right upper quadrant, indicative of reduced hepatic mass secondary to necrosis. Fetor hepaticus is usually present, but recognition of this condition is somewhat subjective. Ascites is more common with subfulminant hepatic failure. Stigmata of chronic liver disease do not support a diagnosis of ALF as per the classic definition. Low blood pressure (decreased systemic vascular resistance) and hypothermia may also be evident. Laboratory derangements include high serum aminotransferase levels, low blood glucose levels, and a prolonged prothrombin time . Metabolic acidosis with respiratory compensation may be evident on arterial blood gas measurement. Complications seen in the course of the illness include cerebral edema ; renal failure ; cardiovascular, pulmonary, and metabolic derangements; and problems with infection, GI bleeding, and malnutrition. Multiorgan failure is commonly encountered. There is an inverse relationship between the presence and number of complications and patient survival. The diagnosis is often delayed without an appropriate index of suspicion, and such delay can have catastrophic implications in as much as early diagnosis and appropriate management are important to preserve the ability of these patients to receive a transplant should it become necessary. Overall, the presence of coagulopathy in a jaundiced patient with an altered mental status remains the hallmark of ALF .
Coagulopathy
Coagulopathy is universally present and can be the first sign of impending liver failure. It is due mainly to decreased hepatic synthesis of clotting factors [72]. Therefore, serial measurements of prothrombin time and factor V levels have prognostic significance and provide the best measure of whether hepatic function is improving or deteriorating. DIC and local fibrinolysis do occur in ALF, and though not usually severe, they can be exacerbated by infection or by the infusion of activated clotting factors [73]. Administration of fresh frozen plasma in the absence of bleeding is not recommended because it has not been shown to be of value [72] and will alter the prothrombin time, thus hindering patient assessment. Platelet function is altered (prolonged capillary bleeding time), and thrombocytopenia secondary to bone marrow suppression, hypersplenism, and intravascular consumption is present in up to two thirds of patients [74]. If invasive procedures are necessary, correction of coagulation abnormalities may be relevant and needed.
Encephalopathy
Unlike the conditions observed in chronic hepatic disease, the encephalopathy associated with ALF can be manifested as agitated delirium, paranoid behavior, or even a psychotic state. Seizures may occur. The initial stages of encephalopathy are secondary to bilateral forebrain dysfunction, with the latter being secondary to brainstem impairment. Table 4 delineates the grading system used for acute hepatic encephalopathy; the presence of stupor or coma portends a poorer prognosis. Although the exact pathogenesis remains elusive, the encephalopathy is reversible and thought to be metabolic. Structural changes such as those seen with Alzheimer’s disease are not part of the syndrome. It is postulated that elevated levels of neuroactive humoral substances secondary to decreased hepatic clearance cause the observed mental status changes. It is important to note that the blood–brain barrier is disrupted in ALF, and this increased permeability makes it unnecessary for a substance to be present in greater than normal concentration in plasma to affect cerebral function. In addition, with the blood–brain barrier demonstrating marked regional differences in permeability, the concentration of potentially encephalopathic agents at critical subcellular sites may be more important than their concentration in cerebrospinal fluid or plasma [75]. Studies have implicated increased GABAergic (transmitting or secreting γ-aminobutyric acid) tone, mediated by an endogenous benzodiazepine-like ligand, as a cause of the hepatic encephalopathy seen in ALF [76]. Treatment with flumazenil (a benzodiazepine receptor antagonist) has been shown to temporarily improve the coma grade of patients suffering from this syndrome.
Cerebral Edema
Cerebral edema with resultant increased intracranial pressure (ICP) is a common complication of ALF, with up to 81% of patients demonstrating signs of increased ICP during the course of the illness [77]. Although it is a distinct entity, its signs and symptoms may be missed because of the presence of concurrent encephalopathy – often with deadly consequences. Herniation of the cerebellar tonsils or the uncinate process of the temporal lobe is a significant cause of death, and evidence of herniation is present in up to 25–30% of patients with cerebral edema [78].
The causative metabolic and pathophysiologic derangements that lead to cerebral edema have yet to be fully elucidated. Research indicates a complex interplay among vasogenic (alterations in blood flow), cytotoxic (loss of osmoregulation), and hydrocephalic (extracellular expansion) factors. Even though earlier histologic studies of the brain revealed no abnormalities [79], more recent data have found alterations in cell membrane integrity and blood–brain barrier permeability [80, 81], changes probably responsible for the increased water content and weight of the brain. Although patients with cirrhosis rarely have cerebral edema, a marked decrease in intracranial blood flow has been noted in those with acute or chronic encephalopathy [82]. This decreased blood flow, along with the systemic hypotension commonly found in ALF (see the next section) and the increased ICP secondary to cerebral edema, predisposes the brain to ischemic injury. Cerebral perfusion pressure (CPP = mean arterial pressure [MAP] – ICP) below 40–50 mmHg is associated with ischemic brain injury and can have permanent consequences, even if the liver recovers fully. A persistent and refractory perfusion pressure of less than 40 mmHg precludes transplantation [83]. Signs of increased ICP are noted in Table 5. Because they are manifested only late in the course of events (i.e., only if ICP is greater than 30 mmHg), these signs cannot be used to gauge the need for therapeutic intervention.
Although computed tomography (CT) scans are often used to exclude intracerebral hemorrhage as a cause of a sudden change in mental state, their static nature in this rapidly evolving syndrome makes them unsuitable as a management guide. ICP monitoring provides reliable data on which treatment decisions can be made, and placement of a subdural or epidural transducer is indicated in patients being considered for transplantation. Patients should be transferred to a transplant center early in the course of the disease; transportation after the onset of cerebral edema and coma is fraught with danger because even positional changes can raise ICP with disastrous consequences. Factors that tend to increase ICP are noted in Table 6. Even without herniation, cerebral edema remains the most common cause of death in ALF .
Cardiovascular Derangements
Systemic hypotension occurs in most patients with ALF and is mediated in part by decreased systemic vascular resistance (resembling septic shock), bacteremia, hemorrhage, hypovolemia, and increased interstitial edema (increased capillary permeability) and ICP. An etiology is not found in up to 60% of cases [84]. Nearly all patients with stage IV encephalopathy suffer from arrhythmias. Although sinus tachycardia is most common, the spectrum includes heart block and cardiac arrest. ST segment and T wave changes may occur. Exacerbating factors include hypoxemia, acidosis, hyperkalemia, and cerebral edema [85].
Renal Failure
Renal impairment is present in up to 75% of patients with ALF [86] more frequent in the elderly and in patients with APAP-induced ALF [87] and includes prerenal azotemia, hepatorenal syndrome, and acute tubular necrosis. Hepatorenal syndrome is a diagnosis of exclusion and is characterized by a serum creatinine concentration greater than 1.5 mg/dL (133 μmol/L), a urinary sodium concentration less than 10 mEq/L (without taking diuretics), lack of improvement with volume expansion, and a bland urinary sediment [88]. Systemic hypotension and splanchnic vasodilation (probably nitric oxide driven) activate the renin-angiotensin axis, with resultant renal vasoconstriction. Renal vasoconstriction leads to a drop in renal perfusion pressure, which is reflected by a decreased glomerular filtration rate and increased sodium retention (causing ascites and edema). The presence of oliguric renal failure portends a poorer prognosis [89]. Renal impairment may also occur secondary to the toxic effects of substances that caused the ALF, such as APAP, hepatotoxic mushrooms, hydrocarbons, and MDMA .
Pulmonary and Ventilatory Derangements
Up to 30% of patients will have evidence of pulmonary edema during the course of their illness, especially those with cerebral edema [90, 91]. Accurate determination of volume status by pulmonary artery pressure monitoring has been shown to improve survival [92]. Intrapulmonary arteriovenous shunting, peripheral capillary blockage with cellular debris from necrotic hepatocytes, or low-grade DIC, interstitial edema, and increased vasomotor tone ultimately lead to lactic acidosis secondary to anaerobic metabolism, which can exacerbate cerebral ischemia [93, 94]. The use of NAC and prostacyclin to improve tissue oxygenation remains experimental and controversial [94–96].
Infection
Metabolic inhibition of polymorphonuclear leukocytes, decreased opsonization, and impaired cell-mediated and humoral immunity greatly predispose patients with ALF to bacteremia and fungemia [58, 97]. Patients have increased risk of infection secondary to multiple indwelling catheters, antacid therapy, artificial ventilation, coma, and treatment with broad-spectrum antibiotics. Skin flora organisms (Staphylococcus and Streptococcus spp.) are most commonly isolated in patients with ALF [98]. In a prospective study of 50 patients with acute liver failure, infection was suspected in 45 patients and proved by positive cultures in 40 [99]. However, prophylactic antibiotic treatment has not been shown to improve survival [100].
Gastrointestinal Bleeding
The severe coagulopathy seen with ALF predisposes patients to hemorrhage from the GI tract, with the upper GI tract being the most frequent site of bleeding [101]. Diffusely hemorrhagic gastritis, esophagitis, and nasogastric tube trauma are common etiologies. Exacerbating factors include tissue hypoxia from hypotension, microcirculatory disruption, and hypoxemia, along with DIC, bacteremia, and ventilator-associated platelet dysfunction. Large episodes of bleeding lead to further hypotension and tissue (including cerebral) hypoxia and can cause worsening renal failure as a result of prerenal azotemia, as well as exacerbating hepatic encephalopathy. Despite the numerous risk factors for hemorrhage, infusion of fresh frozen plasma or platelets for correction of coagulopathy or thrombocytopenia is not indicated in the absence of bleeding.
Metabolic Derangements
Electrolyte and acid–base disturbances are common in ALF and can exacerbate encephalopathy and cause arrhythmias. Despite renal retention of sodium, hyponatremia occurs frequently and is due to impaired renal free water excretion. Hypokalemia is present and can be profound; etiologies are multiple and include renal losses (secondary to hyperaldosteronism and sodium retention, as well as secondary to hydrogen ion resorption to compensate for respiratory alkalosis), GI losses (decreased intake, vomiting), and iatrogenic causes (e.g., diuretics, nasogastric tube suctioning, lactulose use). Hypophosphatemia, hypomagnesemia, and hypocalcemia can also occur. Complex acid–base disturbances with multiple processes at play are seen – respiratory alkalosis as a result of spontaneous hyperventilation is commonly present early in the course of the disease. However, with disease progression and depression of the central respiratory drive secondary to edema or circulating toxins, respiratory acidosis can develop. Hypokalemia is associated with metabolic alkalosis, whereas tissue hypoxia and massive hepatic necrosis give rise to metabolic acidosis with elevated levels of lactic acid, free fatty acid, and other organic acids. The presence of lactic acidosis is a poor prognostic indicator. Impaired glucose release, loss of glycogen reserves, and decreased gluconeogenesis are in combination responsible for severe hypoglycemia (blood glucose <40 mg/dL [2.2 mmol/L]) in up to 40% of patients. Decreased hepatic metabolism of insulin resulting in inappropriately elevated plasma insulin levels also plays a pathogenic role. If unrecognized and untreated, the fall in blood glucose can be rapid and may lead to irreversible brain injury .
Diagnostic Studies
Laboratory and radiographic testing should be performed to confirm the diagnosis, elucidate the etiology of ALF , evaluate for the presence of complications, and obtain data necessary for management, prognostication, and preparation of the patient for possible liver t ransplantation. See Table 7 for a list of recommended initial diagnostic tests for ALF. Serum glucose should be monitored frequently (every 2 h), and other parameters such as electrolytes, hematocrit, and arterial blood gas should be monitored at least three times daily. Coagulation parameters and LFTs are usually checked twice a day. Further testing, such as tomographic studies of the head to rule out intracerebral hemorrhage or cerebral edema as a cause of acute worsening of mental status, is performed as clinically indicated.
Treatment
Because of the unpredictable nature of the disease, the risk of acute decompensation, and the severity of the illness/complications, patients with ALF should be managed in an ICU setting, preferably at a liver transplant center. Hospitals without liver transplant programs should transfer patients with ALF to such transplant centers as soon as possible because increased ICP and severe coagulopathy make transfer later in the course of the disease much more hazardous. Uncompromised ICU support is necessary to give these patients the best chance for survival. Specific treatment strategies for commonly encountered complications are discussed in the following sections.
Coagulopathy
Decreased synthesis of coagulation factors is a direct reflection of hepatic dysfunction and can be used as a prognostic indicator. Therefore, prophylactic correction of coagulopathy in a non-bleeding patient is not recommended because it does not influence mortality, can interfere with assessment of disease severity, and may predispose the patient to volume overload and worsening cerebral edema [24, 102]. Blood products (fresh frozen plasma or, rarely, recombinant human factor VIIa) may be used to correct coagulopathy in cases of active hemorrhage/GI bleeding and for invasive procedures [103].
Encephalopathy
Encephalopathy is part of the definition of ALF and as such plays a major role in the patient’s clinical findings and course. Patients with grade 4 encephalopathy should be intubated for airway protection. Standard treatment with lactulose enemas or lactulose via a nasogastric tube, 30 mL three to four times a day, is instituted in an attempt to decrease the amount of nitrogenous waste (in the form of ammonia) absorbed from the gut lumen. However, new evidence suggest that the use of polyethylene glycol (PEG) may be superior to lactulose in the treatment of encephalopathy in cirrhotic patients [104] (Grade I recommendation). Oral neomycin has traditionally been added if the encephalopathy is difficult to control, but it has possible nephrotoxic and ototoxic side effects. Modern drugs of choice instead are metronidazole, 250–500 mg two to three times a day, aminopenicillins, 2–4 g/day, or vancomycin, 1–2 g/day. More recently it has been shown that the minimally absorbed oral antibiotic rifaximin maintains remission from hepatic encephalopathy more effectively than placebo [105] (Grade I recommendation).
Cerebral Edema
Cerebral edema (leading to elevated ICP, ischemic/hypoxic brain injury, and brainstem herniation) is the most common cause of death in ALF and is present in up to 80% of patients with grade 4 encephalopathy [106]. Given the deadly consequences of unrecognized cerebral edema and the difficulty in diagnosing it clinically, an epidural ICP monitor should be placed in all patients with grade 4 encephalopathy. This procedure has a 4% morbidity (infection, bleeding) rate and a 1% mortality rate and is thus safer than placement of a subdural, parenchymal, or intraventricular catheter [107]. Coagulopathy should be addressed before placement of an ICP monitor, and head CT should be considered to rule out other causes of acute mental status changes such as intracranial hemorrhage. The aim is to keep ICP lower than 20 mmHg and CPP (MAP – ICP = CPP) higher than 50 mmHg [2] (Grade III recommendation).
Elevated ICP can be treated with mannitol boluses (0.5–1 g/kg to achieve a plasma osmolality between 310 and 325 mOsm/kg) [108]. Clinicians should be vigilant for signs of volume overload with mannitol use; concurrent ultrafiltration or other dialysis methods may be needed to avoid hypervolemia. In addition, patients should be stimulated as little as possible because agitation can increase ICP. Sedatives should be used in the lowest dose possible so that the degree of encephalopathy can continue to be monitored. Short-acting drugs such as propofol should be used [109]. Elevating the head of the bed can decrease ICP, but it also causes CPP to fall and leads to paradoxical increases in ICP when elevation is above 30° [102]. In the absence of ICP monitoring, the head of the bed should be elevated 10–20° (Grade III recommendation). The use of positive end-expiratory pressure during ventilation can also worsen cerebral edema [110]. Dexamethasone has been proved to be ineffective as treatment of cerebral edema and should therefore not be used [111]. Hyperventilation to lower PCO2 has not been shown to be beneficial [102].
Renal Failure
Most patients with ALF have evidence of acute kidney injury (AKI) , the presence of which carries a grave prognosis. Treatment is centered on prevention: the use of nephrotoxic drugs (e.g., aminoglycosides) is avoided, intravascular volume is optimized with judicious use of colloid supplementation in the form of packed red cells or salt-poor albumin, and MAP is maintained as close to normal as possible. A high index of suspicion should be entertained for AKI secondary to the direct toxic effects of substances such as APAP or hepatotoxic mushrooms. Although urinary sodium values can be used to guide therapy, the blood urea nitrogen concentration may underestimate the renal dysfunction because of decreased hepatic urea production.
Infection
A decline in renal function or worsening/recalcitrant encephalopathy may be the first clues to an untreated infection in patients with ALF . Thus, a high index of suspicion must be maintained, with a low threshold for diagnostic testing (including blood, urine, and sputum cultures, chest x-ray, paracentesis) and empirical broad-spectrum antibiotic/antifungal coverage. The most common sites of infection include the respiratory system, the urinary tract, and blood [112]. Although prophylactic antibiotic use has not been shown to be helpful, a surveillance culture regimen with aggressive directed therapy if an infection is suspected is recommended.
Gastrointestinal Bleeding
All ALF patients deserve stress ulcer prophylaxis with oral/IV proton pump inhibitors. Sucralfate may also be used. Coagulopathy and thrombocytopenia should be corrected in patients with bleeding from the GI tract, but not prophylactically. Large GI bleeds are investigated and treated endoscopically. If variceal bleeding is suspected, treatment with an octreotide IV drip should be initiated without delay for endoscopic confirmation.
Metabolic Derangements
The various metabolic derangements seen in ALF have been detailed earlier. As part of supportive ICU care, electrolytes should be checked and corrected at least twice a day. Hypoglycemia is common in ALF and needs closer attention. Hypertonic glucose solutions should be administered as an IV drip to keep blood glucose levels above 65 mg/dL (3.6 mmol/L). Restriction of free water may be needed to treat hyponatremia, but hypertonic saline is rarely required. Acetaminophen -induced ALF without renal impairment is commonly associated with hypophosphatemia, which may require therapy [113].
Nutrition
A diet low in protein is advocated for patients with ALF who are able to tolerate oral intake (grade 1–2 encephalopathy). Enteral low-protein tube feeding should be considered early in the course of the disease for the rest of the patients to prevent unnecessary catabolism to preserve muscle bulk and immune function [114] and to optimize management before possible liver transplantation . Tube feeding should be administered into the distal duodenum/jejunum if possible to decrease the risk of aspiration.
Specific Antidotes
Two of the most common conditions for which specific treatment of ALF is available are APAP overdose and Amanita mushroom poisoning. Other rare treatable etiologies include AFLP (treated by delivery), shock liver (treated by optimizing hemodynamic status), acute Budd–Chiari syndrome (treatment considerations include transjugular intrahepatic portosystemic stent shunt versus surgical decompression versus thrombolysis), herpesvirus infection (treated with acyclovir), and autoimmune hepatitis (treated with steroids).
Chapter 59, “Acetaminophen/ Paracetamol” provides detailed discussion on the treatment of APAP overdose, but in general, if severe acetaminophen toxicity is suspected, intravenous NAC should be administered without delay. Activated charcoal (1 g/kg) may decrease APAP absorption if administered within 1 or 2 h of ingestion. In most countries, the plasma APAP concentrations are determined in all suspected cases and values plotted against the established nomogram to determine whether NAC administration is indicated. However, in Denmark the use of a nomogram is not recommended. All patients suspected of APAP poisoning are treated with NAC immediately after hospital admission. Information from patients with suicidal behavior about time of ingestion are often unreliable which may lead to a wrong decision about NAC treatment if a nomogram is used [115]. However, those with liver injury and suspected acetaminophen toxicity, even in the absence of detectable APAP, should receive NAC treatment.
Mushroom poisoning can be established by isolating α-amanitin in serum or urine by radioimmunoassay. Its enterohepatic circulation can be interrupted by using repeated doses of activated charcoal, and possibly forced diuresis can increase the rate of renal clearance of the toxin (see Chap. 108, “Cyclopeptide-Containing Mushrooms: The Deadly Amanitas”). Silibinin and IV penicillin G have been used as specific therapies for Amanita poisoning. Silibinin is thought to impede the uptake of α-amanitin by hepatocytes and may be efficacious up to 48 h after the ingestion of toxin [57].
Prognosis
Patients with ALF can be broadly divided into two categories – those who have enough hepatic reserve left to survive and recover with optimal medical care and those who have sustained an irreversible hepatic insult and will die despite supportive care. OLT is the best available option for the second cohort; it is not appropriate therapy for the first group. The difficulty lies in accurately categorizing patients into one of these two groups and doing so in a timely manner, before the complications associated with ALF preclude OLT as a therapeutic option. Overall, current estimates reveal that only about 10% of patients with ALF receive a transplant [106]. Posttransplant survival rates have been estimated at 55% to 75% [116], although rates may improve to over 90% with stringent selection criteria [108]. As noted earlier, ALF without OLT is associated with very high mortality rates, and survival remains dismal for those who are listed for transplantation but do not receive an organ in time. In general, transplantation is recommended if the patient’s survival rate is estimated to be below 20%.
**A number of prognostic indicators have been identified to help clinicians predict the severity of ALF and identify patients who would benefit from transplantation. It is well known that the etiology and the presence/number of associated complications can influence the survival rate. Time from the onset of jaundice/symptoms to the development of hepatic encephalopathy can also predict a survival difference in certain cohorts, as mentioned in the discussion in the “Definitions” section of this chapter. The severity of encephalopathy at admission is inversely related to survival in patients with acetaminophen toxicity and acute liver failure [25]. Although age younger than 10 or older than 40 years has been shown to be a poor prognostic indicator in older studies, it did not play a role in survival rates from a more recent US series [25]. Liver histology is not routinely used because it has not been proved to accurately predict outcome [117].
The aforementioned variables (age, etiology, degree of encephalopathy, time to onset of symptoms, etc.), though identifying survival trends, do not allow for an accurate prediction of the need for transplantation. To better identify high-risk patients who would require liver transplantation for survival, a statistical model was developed by investigators at King’s College in London. From a cohort of 588 patients managed medically between 1973 and 1985, a multivariate analysis was performed on a number of biochemical and clinical variables and their relationship to mortality, and recommendations for transplantation were based on the results. The negative prognostic indicators (also known as King’s College Criteria) for which transplantation is recommended are noted in Table 8 [1].
The King’s College Criteria have been validated at other centers and in a prospective manner. Patients with ALF but without APAP toxicity demonstrated a mortality rate of 80% with the presence of any one of the negative prognostic indicators; mortality rose to 95% with the association of three negative prognostic factors. Severe acidosis (pH <7.3) in patients with APAP toxicity was associated with a mortality rate of 95%. Excluding acidosis, the presence of any other adverse characteristic in this population resulted in a mortality rate of at least 55%. These mortality rates are much higher than those associated with liver transplantation ; thus, patients with even one negative prognostic indicator should be considered for listing [1]. A subsequent meta-analysis confirmed that the King’s College Criteria have clinically acceptable specificity but more limited sensitivity [118].
Other predictive models have been developed to assess the degree of liver injury and identify patients who need liver transplantation for survival. Acute Physiology and Chronic Health Evaluation (APACHE) II scores were similar to the King’s College Criteria in identifying those needing transplantation, but patients were recognized earlier in a few cases [119]. Serum Gc-globulin and plasma factor V levels have been used independently to predict outcome; however, they are specialized laboratory tests that may not always be available and have not been shown to be any better than the King’s College Criteria [120]. Factor V levels vary by age; transplantation is recommended for a factor V level less than 20% in ALF patients younger than 30 years or for a factor V level less than 30% for those older than 30 years [121]. However, patients have recovered without transplantation with factor V levels less than 10%, in our experience. Also measurement of arterial blood lactate may improve the speed and accuracy of selection of appropriate candidates for OLT. In a single-center study, the prediction of non-surviving APAP-induced ALF patients using lactate was similar to KCH criteria but identified them earlier [122]. Although early recognition of patients most likely to benefit from transplantation is important, it is equally important to recognize those in whom liver transplantation is contraindicated (Table 9).
Future Trends
The scarcity of donor livers has led to investigation of alternatives to transplantation not only for patients who need temporary support while their native liver recovers from the acute insult but also for those who need a “bridge” to transplantation. A number of novel and promising approaches have been tried, including auxiliary liver transplantation , liver dialysis systems, artificial hepatic assist devices, and xenotransplantation. All are in the research phase and need further study with controlled clinical trials to delineate their safety and efficacy. Liver dialysis systems have not met with great success. Hemodialysis, charcoal hemoperfusion, and blood and plasma exchange have been tried without any demonstrated alteration in outcome [102].
Auxiliary liver transplantation involves placement of a partial liver graft in either a heterotopic location or a space provided by partial hepatectomy. Although the graft is not large enough to sustain the patient independently, it provides enough support to allow the native liver to recover. No indications for auxiliary transplantation have been established, and it still requires a donor source in the presence of the current organ shortage. However, a number of patients have recovered when auxiliary grafting is used as a bridge, thus obviating the need for whole-organ transplantation and lifelong immunosuppression [123].
Early experiments of extracorporeal perfusion with animal organs led to the idea of hybrid artificial devices that would combine the efficacy and compatibility of a human liver with the ease of hemodialysis. These hybrids, known as extracorporeal liver assist devices (ELADs) and bioartificial livers, incorporate living human hepatocytes embedded around a nest of hollow fiber capillaries housed in a cartridge through which the patient’s blood is transfused [124]. The device functions as an extracorporeal artificial liver, with the living hepatocytes performing all the functions of the native liver across the semipermeable capillary membrane. Recent research has focused on trying to reproduce the hepatic architecture in the ELAD cartridge, identifying the optimal hepatocyte mass needed to provide the best results, and determining the ideal perfusion time necessary for a favorable outcome. The most extensively studied nonbiological device is the molecular adsorbent recirculating system which has shown some evidence in case series to improve biochemical parameters [125].
References
O’Grady JG, Alexander GJM, Hayllar KM, et al. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology. 1989;97:439–45.
Ichai P, Samuel D. Epidemiology of liver failure. Clinics Res Hepatol Gastroenterol. 2011;35:610–7.
Bernal W, Cross TJ, Auzinger G, et al. Outcome after wait-listing for emergency liver transplantation in acute liver failure: a single centre experience. J Hepatol. 2009;50:306–13.
Escorsell A, Mas A, de la Mata M. Acute liver failure in Spain: analysis of 267 cases. Liver Transpl. 2007;13:1389–95.
Simpson KJ, Bates CM, Henderson NC, et al. The utilization of liver transplantation in the management of acute liver failure: comparison between acetaminophen and non-acetaminophen etiologies. Liver Transpl. 2009;15:600–9.
Germani G, Theocharidou E, Adam R, et al. Liver transplantation for acute liver failure in Europe: outcomes over 20 years from the ELTR database. J Hepatol. 2012;57:288–96.
Bernuau J, Rueff B, Benhamou JP. Fulminant and subfulminant liver failure: definitions and causes. Semin Liver Dis. 1986;6:97–106.
O’Grady JG, Schalm SW, Williams R, et al. Acute liver failure: redefining the syndromes. Lancet. 1993;342:273–5.
Takahashi Y, Shimizu M. Aetiology and prognosis of fulminant viral hepatitis in Japan: a multicenter study. J Gastroenterol Hepatol. 1991;6:159–64.
Bernuau J, Goudeau A, Poynard T, et al. Multivariate analysis of prognostic factors in fulminant hepatitis B. Hepatology. 1986;6:648–51.
Acharya SK, Dasarathy S, Tandon BN. Should we redefine acute liver failure? [letter]. Lancet. 1993;342:1421–2.
Tandon BN, Bernauau J, O'Grady J, et al. Recommendations of the International Association for the Study of the Liver Subcommittee on nomenclature of acute and subacute liver failure. J Gastroenterol Hepatol. 1999;14:403–4.
Keppler D, Popper H, Bianchi L, et al., editors. Mechanisms of hepatocellular injury and death. Lancaster, UK: MTP Press; 1984.
Schanne FAX, Kane AB, Young EE, et al. Calcium dependence of toxic cell death: a final common pathway. Science. 1979;206:700.
Popper H, Keppler D. Networks of interacting mechanisms of hepatocellular degeneration and death. Prog Liver Dis. 1986;8:209.
Miwa Y, Harrison PM, Farzaneh F, et al. Plasma levels and hepatic mRNA expression of transforming growth factor-beta1 in patients with fulminant hepatic failure. J Hepatol. 1997;27:780–8.
Eguchi S, Okudaira S, Azuma T, et al. Changes in liver regenerative factors in a case of living-related liver transplantation. Clin Transplant. 1999;13:536–44.
Andus T, Bauer J, Gerok W. Effects of cytokines on the liver. Hepatology. 1991;13:364–75.
Yumoto E, Higashi T, Nouso K, et al. Serum gamma-interferon–inducing factor (IL-18) and IL-10 levels in patients with acute hepatitis and fulminant hepatic failure. J Gastroenterol Hepatol. 2002;17:285–94.
White HM. Evaluation and management of liver failure. In: Rippe JM, editor. Intensive care medicine. 3rd ed. Boston: Little, Brown; 1996.
Ostapowicz G, Fontana RJ, Schiodt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:947–54.
Reuben A, Koch DG, Lee WM. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76.
Prescott LF. Paracetamol overdosage: pharmacological considerations and clinical management. Drugs. 1983;25:290.
O'Grady JG, Portmann B, Williams R. Fulminant hepatic failure. In: Schiff L, Schiff R, editors. Diseases of the liver. Philadelphia: JB Lippincott; 1993.
Schiodt FV, Atillasoy E, Shakil AO, et al. Etiology and outcome for 295 patients with acute liver failure in the United States. Liver Transpl Surg. 1999;5:29.
Oketani M, Ido A, Tsubouchi H. Changing etiologies and outcomes of acute liver failure: a perspective from Japan. J Gastroenterol Hepatol. 2011;26:65–71.
Gulmez SE, Larrey D, Pageaux G-P, et al. Liver transplant associated with paracetamol overdose: results from the seven-country SALT study. Br J Clin Pharmacol. 2015;80:599–606.
Lewis RK, Paloucek FP. Assessment and treatment of acetaminophen overdose. Clin Pharm. 1991;10:765.
Craig DGN, Bates CM, Davidson JS, et al. Staggered overdose pattern and delay to hospital presentation are associated with adverse outcomes following paracetamol-induced hepatotoxicity. Br J Clin Pharmacol. 2012;73:285–94.
Whitcomb DC, Block GD. Association of acetaminophen toxicity with fasting and ethanol use. JAMA. 1994;272:1845–18504.
Schmidt LE, Dalhoff K. Serum phosphate is an early predictor of outcome in severe acetaminophen-induced hepatotoxicity. Hepatology. 2002;36:659–65.
Mitchell JR, Jollow JD, Potter WZ, et al. Acetaminophen-induced hepatic necrosis: I. Role of drug metabolism. J Pharmacol Exp Ther. 1973;187:185.
Mitchell JR, Jollow JD, Potter WZ, et al. Acetaminophen-induced hepatic necrosis: IV. Protective role of glutathione. J Pharmacol Exp Ther. 1973;187:211.
Slattery JT, Nelson SD, Thummel KE. The complex interaction between ethanol and acetaminophen. Clin Pharmacol Ther. 1996;60:241.
Murphy R, Swartz R, Watkins PB. Severe acetaminophen toxicity in a patient receiving isoniazid. Ann Intern Med. 1980;113:399.
Bray GP, Harrison PM, O’Grady JG, et al. Long term anticonvulsant therapy worsens outcome in paracetamol induced hepatic failure. Hum Exp Toxicol. 1992;11:265.
Lauterburg BH, Velez ME. Glutathione deficiency in alcoholics: risk factor for paracetamol. Hepatology. 1988;29:1153.
Zimmerman HJ, Maddrey WC. Acetaminophen (paracetamol) hepatotoxicity with regular intake of alcohol: analysis of instances of therapeutic misadventure. Hepatology. 1995;22:767.
Pessayre D, Bentata M, Degott C, et al. Isoniazid-rifampin fulminant hepatitis. A possible consequence of the enhancement of isoniazid hepatotoxicity by enzyme induction. Gastroenterology. 1977;72:284.
Riley 3rd TR, Smith JP. Ibuprofen-induced hepatotoxicity in patients with chronic hepatitis C: a case series. Am J Gastroenterol. 1998;93:1563–5.
Garcia-Rodriguez LA, Williams R, Derby LE, et al. Acute liver injury associated with NSAIDs and the role of risk factors. Arch Intern Med. 1994;154:311–6.
Shaheen N, Grimm IS. Fulminant hepatic failure associated with clarithromycin. Am J Gastroenterol. 1996;91:394–5.
Björnsson ES, Bergman OM, Björnsson HK, et al. Incidence, presentation, and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25.
Zimmerman HJ. Hepatotoxicity. The adverse effects of drugs and other chemicals on the liver. New York: Appleton; 1978.
Pratt DS, Kaplan MM. Evaluation of abnormal liver enzyme results in asymptomatic patients. N Engl J Med. 2000;342:1266–71.
Escher, et al. Hepatitis associated with Kava, a herbal remedy for anxiety. BMJ. 2001;322:1097.
Kraft, et al. Fulminant liver failure after administration of the herbal antidepressant Kava-Kava. Dtsch Med Wochenschr. 2001;126(36):970–2.
Scully RE, Mark EJ, McNeely WF, et al. Case records of the Massachusetts General Hospital. N Engl J Med. 2001;344:591–9.
Brauer RB, Heidecke CD, Nathrath W, et al. Liver transplantation for the treatment of fulminant hepatic failure induced by the ingestion of ecstasy. Transpl Int. 1997;10:229–33.
Bryson PD. Mushrooms. In: Bryson PD, editor. Comprehensive Review in Toxicology for Emergency Clinicians. 3rd ed. DC, Taylor & Francis: Washington; 1996. p. 685–93.
Klein AS, Hart J, Brems JJ, et al. Amanita poisoning: Treatment and the role of liver transplantation. Am J Med. 1989;86:187–93.
Lampe KF, McCann MA. AMA Handbook of Poisonous and Injurious Plants. Chicago: American Medical Association; 1985.
Pinson CW, Daya MR, Benner KG, et al. Liver transplantation for severe Amanita phalloides mushroom poisoning. Am J Surg. 1990;159:493–9.
Kopple C. Clinical symptomatology and management of mushroom poisoning. Toxicon. 1993;31:1513–40.
O’Brien B, Khuu L. A fatal Sunday brunch: Amanita mushroom poisoning in a Gulf Coast family. Am J Gastroenterol. 1996;91:581–3.
Faulstich H. New aspects of Amanita poisoning. Klin Wochenschr. 1979;57:1143–52.
Wieland T, Faulstich H. Fifty years of Amanita review. Experientia. 1991;47:1186–93.
Fagan EA, Williams R. Fulminant viral hepatitis. Br Med Bull. 1990;46:462–80.
Hoofnagle JH, Nelson KE, Purcell RH. Hepatitis E. N Engl J Med. 2012;367:1237–44.
Wasley a, Fiore A, Bell BP: Hepatitis A in the era of vaccination. Epidemiol Rev 2006;28: 101–111.
Khuroo MS, Kamili S. Aetiology and prognostic factors in acute liver failure in India. J Viral Hepat. 2003;10:224–31.
Lucke B. The fulminant form of epidemic hepatitis. Am J Pathol. 1946;22:867.
Mathieson LR, Linglof T, Moller AM, et al. Fulminant hepatitis A. J Infect Dis. 1979;11:303.
Vallbracht A, Maier K, Stierhof Y, et al. Liver-derived cytotoxic T cells in hepatitis A virus infection. J Infect Dis. 1989;160:209.
Wright TL, Mamish D, Combs C, et al. Hepatitis B and apparent non-A, non-B hepatitis. Lancet. 1992;339:952.
Saracco G, Macagno S, Rosina F, et al. Serologic markers with fulminant hepatitis in persons positive for hepatitis B surface antigen: A worldwide epidemiologic and clinical survey. Ann Intern Med. 1988;108:380–3.
Christie AB, Allam AA, Aref MK, et al. Pregnancy hepatitis in Libya. Lancet. 1976;2:827–9.
Chu CM, Yeh CT, Liaw YF. Fulminant hepatic failure in acute hepatitis C: Increased risk in chronic carriers of hepatitis B virus. Gut. 1999;45:613.
Smedile A, Verme G, Cargnel A, et al. Influence of delta infection on severity of hepatitis B. Lancet. 1982;2:945–7.
Dematte JE, O’Mara K, Buescher J, et al. Near-fatal heat stroke during the 1995 heat wave in Chicago. Ann Intern Med. 1995;129:173.
Sims HF, Brackett JC, Powell CK. The molecular basis of pediatric long chain 3-hydroxyacyl-CoA dehydrogenase deficiency associated with maternal acute fatty liver of pregnancy. Proc Natl Acad Sci U S A. 1995;92:841–5.
Pereira LMMB, Langley PG, Hayllar KM, et al. Coagulation factor V and VIII/V ratio as predictors of outcome in paracetamol induced fulminant hepatic failure: Relation to other prognostic indicators. Gut. 1992;33:98–102.
Hillenbrand P, Prabhoo SP, Jedrychowski A, et al. Significance of intravascular coagulation and fibrinolysis in acute hepatic failure. Gut. 1974;15:83.
O’Grady JG, Langley PG, Isola LM. Coagulopathy of fulminant hepatic failure. Semin Liver Dis. 1986;6:159–63.
Jones EA, Schafer DF, Ferenci P, et al. The neurobiology of hepatic encephalopathy. Hepatology. 1984;4:1235.
Mullen KD, Martin JV, Mendelson WB, et al. Could an endogenous benzodiazepine ligand contribute to hepatic encephalopathy? Lancet. 1988;1:457–9.
Gimson AES, Braude S, Mellon PJ, et al. Earlier charcoal hemoperfusion in fulminant hepatic failure. Lancet. 1982;2:681.
Ware AJ, D’Agostino A, Combes B. Cerebral edema: A major complication of massive hepatic necrosis. Gastroenterology. 1971;61:877.
Berk PD, Popper H: Fulminant hepatic failure. Annotated abstracts of a workshop held at the National Institutes of Health, 1977. Am J Gastroenterol 1978;69:349.
Traber PG, Dal Canto M, Ganger DR, et al. Electron microscopic evaluation of brain edema in rabbits with galactosamine induced fulminant hepatic failure: Ultrastructure and integrity of the blood–brain barrier. Hepatology. 1987;7:1272–7.
Kato M, Hughes RD, Keays RT, et al. Electron microscopic study of brain capillaries in cerebral edema from fulminant hepatic failure. Hepatology. 1992;15:1060–6.
Almdal T, Schroeder T, Ranek L. Cerebral blood flow and liver function in patients with encephalopathy due to acute and chronic liver diseases. Scand J Gastroenterol. 1989;24:229–303.
Lidofsky SD, Bass NM, Prager MC, et al. Intracranial pressure monitoring and liver transplantation for fulminant hepatic failure. Hepatology. 1992;16:1–7.
Trewby PN, Williams R. Pathophysiology of hypotension in patients with fulminant hepatic failure. Gut. 1977;18:1021.
Weston MJ, Talbot IC, Howorth PJN, et al. Frequency of arrhythmias and other cardiac abnormalities in fulminant hepatic failure. Br Heart J. 1976;38:1179.
O’Grady JG, Williams R. Management of acute liver failure. Schweiz Med Wochenschr. 1986;116:541.
Leithead JA, Ferguson JW, Bates CM, et al. The systemic inflammatory response is predictive of renal dysfunction in patients with non-paracetamol-induced acute liver failure. Gut. 2009;58:443–9.
Arroyo V, Gines P, Gerbes AL, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. International Ascites Club Hepatology. 1996;23:164–76.
Moore K, Taylor G, Ward P, et al. Etiology and management of renal failure in acute liver failure. In: Williams R, Hughes RD, editors. Acute Liver Failure: Improved Understanding and Better Therapy. London: Miter Press; 1991. p. 47–53.
Warren R, Trewby PN, Laws JW, et al. Pulmonary complications in fulminant hepatic failure: Analysis of serial radiographs from 100 consecutive patients. Clin Radiol. 1978;29:346.
Trewby PN, Warren R, Contini S, et al. Incidence and pathophysiology of pulmonary edema in fulminant hepatic failure. Gastroenterology. 1978;74:859.
Wendon J, Alexander GJM, Williams R. Cardiovascular monitoring and local blood flow. In: Williams R, Hughes RD, editors. Acute Liver Failure: Improved Understanding and Better Therapy. London: Miter Press; 1991. p. 39–41.
Bihari D, Gimson AW, Lindridge J, et al. Lactic acidosis in fulminant hepatic failure. Some aspects of pathogenesis and prognosis J Hepatol. 1985;1:405.
Bihari D, Gimson AES, Waterson M, et al. Tissue hypoxia during fulminant hepatic failure. Crit Care Med. 1985;13:1043–9.
Harrison PM, Wendon JA, Gimson AES, et al. Improvement by acetylcysteine of hemodynamic and oxygen transport in fulminant hepatic failure. N Eng J Med. 1991;324:1852–7.
Walsh TS, Hopton P, Philips BJ, et al. The effect of N-acetylcysteine on oxygen transport and uptake in patients with fulminant hepatic failure. Hepatology. 1998;27:1332–40.
Bailey RJ, Woolf IL, Cullens H, et al. Metabolic inhibition of polymorphonuclear leukocytes in fulminant hepatic failure. Lancet. 1976;1:1162–3.
Wyke RJ, Canalese JC, Gimson AES, et al. Bacteremia in patients with fulminant hepatic failure. Liver. 1982;2:45–52.
Rolando N, Harvey F, Brahm J, et al. Prospective study of bacterial infection in acute liver failure: An analysis of fifty patients. Hepatology. 1990;11:49–53.
Rolando N, Gimson A, Wade J, et al. Prospective controlled trial of selective parenteral and enteral antimicrobial regimen in fulminant hepatic failure. Hepatology. 1993;17:196–201.
Gazzard BG, Portmann B, Murray-Lyon IM, et al. Causes of death in fulminant hepatic failure and relationship to quantitative histological assessments of parenchymal damage. Q J Med. 1975;44:615.
Caraceni P, van Thiel DH. Acute liver failure. Lancet. 1995;345:163.
Shami VM, Macik BG, Hespenheide EE, et al: Recombinant activated factor VII is superior to plasma alone in correcting the coagulopathy of fulminant hepatic failure [abstract]. Hepatology 2001;34:327A.
Rahimi RS, Singal AG, Cuthbert JA, et al. Lactulose vs polyethylene glycol 3350-electrolyte solution for treatment of overt hepatic encephalopathy. The HELP randomized clinical study. J Am Med Ass Intern Med. 2014;174:1727–33.
Bass NM, Mullen KD, Sanyal A, et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362:1071–81.
Lee WM. Medical progress: Acute liver failure. N Engl J Med. 1993;329:1862–72.
Blei AT, Olafsson S, Webster S, et al. Complications of intracranial pressure monitoring in fulminant hepatic failure. Lancet. 1993;341:157.
Ascher NL, Lake JR, Emond JC, et al. Liver transplantation for fulminant hepatic failure. Arch Surg. 1993;128:677.
Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Am J Health Syst Pharm 2002;59:150–178.
Munzo SJ. Difficult management problems in fulminant hepatic failure. Semin Liver Dis. 1993;13:395.
Canales J, Gimson AE, Davis C, et al. Controlled trial of dexamethasone and mannitol for cerebral oedema of fulminant hepatic failure. Gut. 1982;23:625.
Mas A, Rodes J. Fulminant hepatic failure. Lancet. 1997;349:1081.
Schmidt LE, Dalhoff K, Poulsen HE. Acute versus chronic alcohol consumption in acetaminophen-induced hepatotoxicity. Hepatology. 2002;35:876–82.
Plauth M, Cabré E, Riggio O, et al. ESPEN guidelines on enteral nutrition: liver disease. Clin Nutr. 2006;25:285–94.
Clemmesen JO, Ott P, Dalhoff K, et al. Recommendations for treatment of paracetamol poisoning. Ugeskr Læger. 1996;158:6892–5.
Riegler JL, Lake JR. Fulminant hepatic failure review. Med North Am. 1993;77:1057–83.
Hanau C, Munoz SJ, Rubin R, et al. Histopathological heterogeneity in fulminant hepatic failure. Hepatology. 1995;21:345.
McPhail MJW, Wendon JA, Bernal W. Meta-analysis of performance of Kings’ College Hospital Criteria in prediction of outcome in non-paracetamol-induced acute liver failure. J Hepatol. 2010;53:492–9.
Mitchell I, Bihari D, Chang R, et al. Earlier identification of patients at risk from acetaminophen-induced acute liver failure. Crit Care Med. 1998;26:279–84.
Pauwels A, Mostefa-Kara N, Floret C, et al. Emergency liver transplantation for acute liver failure. Evaluation of London and Clichy criteria J Hepatol. 1993;17:124.
Schiodt FV, Bondesen S, Petersen I, et al. Admission levels of serum Gc-globulin: Predictive value in fulminant hepatic failure. Hepatology. 1996;23:713–8.
Bernal W, Donaldson N, Wyncoll D, et al. Blood lactate as an early predictor of outcome in paracetamol-induced acute liver failure: a cohort study. Lancet. 2002;359:558–63.
Chenard-Neu MP, Boudjema K, Bernuau J, et al. Auxiliary liver transplantation: Regeneration of the native liver and outcome in 30 patients with fulminant hepatic failure. Hepatology. 1996;23:1119–27.
Nagamori S, Hasumura S, Matsuura T, et al. Developments in bioartificial liver research: Concepts, performance, and applications. J Gastroenterol. 2000;35:493–503.
Tritto G, Davies NA, Jalan R. Liver Replacement Therapy. Semin Respir Crit Care Med. 2012;33:70–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Grading System for Levels of Evidence Supporting Recommendations in Critical Care Toxicology, 2nd Edition
-
I
Evidence obtained from at least one properly randomized controlled trial.
-
II-1
Evidence obtained from well-designed controlled trials without randomization.
-
II-2
Evidence obtained from well-designed cohort or case–control analytic studies, preferably from more than one center or research group.
-
II-3
Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of the introduction of penicillin treatment in the 1940s) could also be regarded as this type of evidence.
-
III
Opinions of respected authorities, based on clinical experience, descriptive studies, and case reports, or reports of expert committees.
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this entry
Cite this entry
Dalhoff, K. (2017). Toxicant-Induced Hepatic Injury. In: Brent, J., et al. Critical Care Toxicology. Springer, Cham. https://doi.org/10.1007/978-3-319-17900-1_75
Download citation
DOI: https://doi.org/10.1007/978-3-319-17900-1_75
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-17899-8
Online ISBN: 978-3-319-17900-1
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences