Abstract
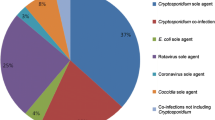
Cryptosporidiosis, caused by the apicomplexan parasite Cryptosporidium parvum, is a moderate-to-severe diarrheal disease now recognized as one of the leading causes of morbidity and mortality in livestock globally, and in humans living in resource-limited parts of the world, particularly those with AIDS or malnourished individuals. This recognition has fueled efforts for the discovery of effective therapeutics. While recent progress in drug discovery has been encouraging, there are presently no acceptably effective parasite-specific drugs for the disease. The urgent need for new drug discovery or drug repurposing has also increased the need for refined animal models of clinical disease for therapeutic efficacy evaluation. Here, we describe an acute model of cryptosporidiosis using newborn calves to evaluate well-defined clinical and parasitological parameter outcomes, including the effect on diarrhea severity and duration, oocyst numbers produced, and multiple measures of clinical health. The model is highly reproducible and provides unequivocal direct measures of treatment efficacy on diarrhea severity and parasite replication.
You have full access to this open access chapter, Download protocol PDF
Similar content being viewed by others
Keywords
- Cryptosporidium
- Cryptosporidiosis
- Bovine model
- Therapeutic evaluation
- Oocyst quantitation
- Diarrhea quantitation
- Clinical evaluation
1 Introduction
Cryptosporidium species are among the leading causative agents of diarrhea in humans and agriculturally important livestock species throughout the world, namely calves [1,2,3]. Despite this, there are currently no approved vaccines and no parasite-specific drugs to treat the disease in either humans or livestock in the US. The only Food and Drug Administration-approved drug for treating cryptosporidiosis in humans is nitazoxanide [4]. However, the efficacy of nitazoxanide against Cryptosporidium in immunocompetent humans is marginal and the drug has no treatment benefit against the parasite in AIDS patients [5,6,7]. The clear need for more effective parasite-specific drugs has increased the need for refined, reliable animal models of cryptosporidiosis for therapeutic efficacy evaluation.
Neonatal calves can provide an excellent acute clinical model for both human and bovine cryptosporidiosis. During the 10–14-day-old age period most often used, neonatal calves are functional monogastrics and remain so up to 4 weeks of age [8, 9]. Clinical symptoms and diarrhea severity and duration following experimental infection in calves closely mirror what is observed in humans [8, 10]. Further, the anatomic distribution of infection in the GI tract and lesions are essentially the same as those observed in humans [8, 10]. Given these observations supporting the validity of calves as a useful clinical model most closely approximating human cryptosporidiosis, multiple methodologies and experimental designs for evaluation of therapeutics in the model have been published. The most commonly used calf models differ mainly in (1) frequency of fecal collection, (2) type of calf housing used (elevated stalls, or box stalls/pens), (3) whether total daily fecal volume excreted is collected, or a ~10–15 mL fecal sample is obtained per rectum once or twice daily, (4) methods used for determining diarrhea severity (quantitative or semi-quantitative), (5) methods used for evaluating oocyst shedding (quantitative, e.g., qPCR or hemocytometer enumeration of the total number of oocysts shed in total daily fecal collections, or various semi-quantitative measures, e.g., acid-fast stain or immunofluorescence assay on fecal sample smears and microscopic scoring, or qPCR on fecal samples collected every 12–24 h), (6) trial duration and (7) C. parvum isolate used (field vs characterized) [11,12,13,14,15,16]. Total daily fecal collection is required to unequivocally determine diarrhea severity and total number of oocysts produced and requires housing in elevated stalls [11,12,13]; these measurements are not possible with box stall or pen housing in which a ~10–15 mL fecal sample is collected daily per rectum [14,15,16]. Model designs vary between investigator and institutional factors (e.g., housing facilities and equipment availability, investigator preferences, staffing resources and abilities, budgetary constraints) and can influence the accuracy of results for efficacy parameters. Therefore, the experimental design used in a particular calf model study should be considered when interpreting efficacy results of a given therapeutic and when making comparisons between studies. For example, in one calf model of cryptosporidiosis, treating calves with nitazoxanide reduced the duration of C. parvum oocyst shedding and diarrhea severity [14], while in another calf model, nitazoxanide had no therapeutic or prophylactic efficacy against clinical disease caused by C. parvum, and in some C. parvum-infected calves nitazoxanide treatment actually prolonged and exacerbated diarrhea [15]. In a calf model similar to the preceding, paromomycin demonstrated prophylactic efficacy against C. parvum challenge and proof of concept, but the drug dosage required was determined to be cost prohibitive for veterinary use [16]. While there is no universally applicable design for the calf model given geographic, institutional, and laboratory constraints, we have used the acute model described here to consistently replicate data demonstrating therapeutic efficacy for multiple bumped kinase inhibitor (BKI) drugs for further study, as well as to consistently replicate data demonstrating lower, clinically less satisfactory efficacy for other BKIs to eliminate from further study [11, 17] (M.W. Riggs and D.A. Schaefer, unpublished).
The model described here is quite labor-intensive and demanding on personnel compared to some other calf models for evaluation of therapeutics and requires housing calves in elevated stalls for total fecal collection. However, the increased labor and demands are justified because the method yields the most accurate efficacy data using defined, quantitative outcome parameters. Determining total daily fecal volume and consistency for each calf provides an objective and unequivocal direct measure of diarrhea severity. Total daily fecal collection is also the preferred practice in human challenge studies to evaluate the efficacy of candidate anti-cryptosporidial preparations [18]. In addition, total daily fecal collection allows accurate determination of total number of oocysts produced per day as an unequivocal measure of treatment effect on parasite replication, and also avoids potential error resulting from diurnal variations in oocyst shedding we have observed in this model [11] (see Note 1). Reduction of oocyst shedding is an important treatment outcome when considering the epidemiologic importance of the environmental parasite burden and exposure risk to both humans and livestock [19]. By 8 or 9 days post infection (DPI), most untreated control calves are beginning to resolve diarrhea in this model [11, 17]. Therefore, we end the experiment at 10 DPI to conclude initial efficacy determinations.
We previously attempted total fecal collection from calves using strap-on commercial fecal collection bags designed for small ruminant metabolic studies [20]. This allowed individual calves to be housed in larger box stalls. However, fecal collection bags invariably leaked or became detached and failed completely, despite emptying up to three times daily. Emptying the bags also required manual restraint of calves and resulted in visible distress. Given all of the above, housing of calves in elevated stalls in this acute model design is thus scientifically and ethically justified and is approved by the Institutional Animal Care and Use Committee. The method presented here is completed in the following major sequential steps or procedures to evaluate therapeutics in this calf model of cryptosporidiosis: (1) procure isolated Cryptosporidium parvum oocysts and age-matched (within 12 h) newborn pathogen-free Holstein bull calves for therapeutic efficacy evaluation, (2) manage husbandry of calves housed in elevated stalls, modified to accurately evaluate clinical health parameters, diarrhea severity, parasite production and urine production, (3) infect calves with C. parvum at 36–48 h of age and administer candidate therapeutic agents per the appropriate dosage and treatment regimen commencing at 2 DPI, (4) collect and process feces to determine total daily fecal volumes and total daily oocyst counts, (5) complete terminal procedures and euthanize calves at 10 DPI, and (6) analyze data for significant treatment effects on clinical health, total fecal volume (diarrhea severity), total oocysts produced (parasite replication), total urine volume (an additional index of hydration), and body weight gain or loss.
2 Materials
2.1 Preparation of Cryptosporidium parvum Oocysts
-
1.
Fully equipped BSL-2 laboratory.
-
2.
Peracetic acid.
-
3.
Taurocholic acid.
-
4.
Trypsin.
-
5.
Phosphate-buffered saline (PBS).
-
6.
Phase-contrast and immunofluorescence microscopes.
-
7.
Hemocytometer.
2.2 Newborn Calves for Therapeutic Efficacy Evaluation
-
1.
Cargo van with climate control for heating and cooling.
-
2.
Rubber boots and coveralls.
-
3.
Roll of 10 mil plastic sheeting, ~185 cm wide.
-
4.
Disinfectant (quaternary ammonium-based for animal facilities).
-
5.
Weight scale for calves.
-
6.
Wheelbarrow.
-
7.
Clostridium perfringens Type C antitoxin and anti-Escherichia coli passive antibody for calves (Ecolizer®, Novartis, Larchwood, IA).
-
8.
Attenuated bovine rotavirus and coronavirus vaccine (CalfGuard®, Zoetis, Kalamazoo, MI).
-
9.
Clean blankets and thick terry cloth cotton towels.
-
10.
Newborn calf record sheets.
-
11.
Surgical scissors to trim umbilical cords.
-
12.
Ear tags and applicator.
-
13.
7% iodine scrub.
-
14.
10% iodine solution.
-
15.
Colostrum replacer (bovine IgG colostrum replacer, Land O’ Lakes, Shoreview, MN).
-
16.
Disinfected 6 L buckets.
-
17.
Whisk.
-
18.
Plastic feeding bottles with rubber nipples (2 L).
-
19.
Esophageal tube feeder.
-
20.
Hand soap and disposable disinfectant wipes.
-
21.
Calf transport crates (crates designed for 90–125 pound dogs work well-one calf per crate).
-
22.
Autoclaved straw.
2.3 Modified Elevated Calf Stalls, Calf Husbandry
Coordinate with local Institutional Animal Care and Use Committee (IACUC, or equivalent) on stall requirements for calves.
-
1.
Elevated calf stalls (~152 cm L × ~122 cm H × ~53.5 cm W; Wenke Mfg, Pender NE).
-
2.
Large rectangular plastic bins (~58.5 cm × ~43 cm × ~15 cm; ~26 L) (4 per calf stall—3 for fecal collection and 1 for urine collection).
-
3.
Reinforced waterproof industrial strength adhesive tape.
-
4.
Roll of 6 mil plastic sheeting, ~122 cm wide.
-
5.
Large clamp binder clips to hold fecal collection bins together.
-
6.
Wall mirrors (~100 cm × 100 cm).
-
7.
Serum refractometer.
2.4 Calf Infection and Treatment
-
1.
Isolated peracetic acid-disinfected C. parvum oocysts.
-
2.
Candidate therapeutic in vehicle and vehicle alone.
-
3.
C. parvum-specific monoclonal antibody(ies) and fluoresceinated secondary antibody for indirect immunofluorescence assay.
-
4.
Disposable 50 cc blunt ended catheter tip dosing syringes.
-
5.
Disposable Tyvek® suits (various sizes) with elastic-cinched ankles and wrists.
-
6.
Disposable plastic booties and plastic boot covers (all to be worn over shoes); alternatively rubber boots.
-
7.
N95 respirators.
-
8.
Goggles and protective glasses.
-
9.
Assorted disposable nitrile gloves.
-
10.
Hair net bonnets.
-
11.
Fecal specimen cups (150 mL urinalysis cups) with lids.
-
12.
Labels for fecal specimen cups.
-
13.
Rectal thermometer.
-
14.
Disinfectant (quaternary ammonium-based for animal facilities).
-
15.
Mop bucket and mop.
-
16.
Plastic scraper.
-
17.
Assorted syringes and needles.
-
18.
Appropriate blood collection tubes.
-
19.
Flunixin meglamine.
-
20.
Injectable selenium and vitamin E supplement (~1 mg selenium, 50 mg (68 USP units) vitamin E per mL).
-
21.
Oral electrolytes for calves (or equivalent).
-
22.
Milk replacer (crude protein ~22%, crude fat ~20%).
2.5 Fecal Processing
-
1.
Personal protective equipment listed in Subheading 2.4.
-
2.
Assorted size graduated cylinders (4, 2, 1 L, and 500 mL)
-
3.
Buckets (4 L)
-
4.
Commercial blender (4 L capacity)
-
5.
Paper towels
-
6.
Plastic ladle and spatula
-
7.
Disinfectant (quaternary ammonium-based for animal facilities)
-
8.
Pressure washer for cleaning post-trial
2.6 Fecal Oocyst Quantitation
-
1.
Real-time PCR (qPCR) System (ABI StepOne Plus®; Applied Biosystems, Grand Island, NY).
-
2.
Real-time PCR (qPCR) reagents.
-
3.
Fecal oocyst DNA extraction reagents and buffers (QIAamp® Fast DNA stool mini kit; Qiagen, Gaithersburg, MD).
-
4.
DNA quantification method (Nanodrop®; Nanodrop Technologies, Wilmington, DE).
-
5.
Primers (we use the C. parvum oocyst wall protein gene (COWP) (Genbank no. AF248743) as the target for primers and selected a 151-bp sequence from the COWP gene).
-
6.
SYBR-green (or equivalent nucleic acid stain).
-
7.
Bovine serum albumin.
2.7 Terminal Procedures and Calf Euthanasia
-
1.
Xylazine.
-
2.
Ketamine.
-
3.
Appropriate blood collection tubes.
-
4.
Euthanasia solution (390 mg pentobarbital sodium/mL, 50 mg phenytoin sodium/mL, or equivalent).
-
5.
Weight scale.
3 Methods
For use in the following methods for evaluation of therapeutics in a bovine clinical model of cryptosporidiosis, calves must be maintained in climate-controlled Animal Biosafety Level 2 (ABSL-2) biocontainment facilities in accordance with the Biosafety in Microbiological and Biomedical Laboratories guidelines and Guide for the Care and Use of Laboratory Animals. Approval by The Institutional Animal Care and Use Committee (IACUC) is required and the methods must be performed in compliance with guidelines in the Animal Welfare Act and Guide for the Care and Use of Agricultural Animals in Research and Teaching (Federation of Animal Science Societies), preferably in facilities fully accredited by the American Association for Laboratory Animal Care. The model described here has been established and operative in the authors’ laboratory for almost two decades [11,12,13]. Based on the large number of unsolicited outside requests we receive for testing of candidate anti-cryptosporidials in this model from industry and established Cryptosporidium investigators at other institutions, we presume that the model is a preferred practice. However, the model should only be used for further evaluation of lead candidate therapeutics or prophylactics which have demonstrated highly significant anti-cryptosporidial activity in vitro and in at least one less sentient species rodent model such as neonatal mice. While neonatal mice are the lowest species suitable for initial in vivo evaluation of therapeutics against Cryptosporidium parvum, the infection is asymptomatic. However, reduction of infection levels in the neonatal mouse model has positive predictive value for therapeutic efficacy against C. parvum in clinical models of disease including calves [11, 13, 21, 22].
3.1 Procurement and Preparation of Cryptosporidium parvum Oocysts for Calf Infection
-
1.
Decide on the C. parvum isolate to be used and obtain purified oocysts from a source production laboratory. We routinely use the Iowa C. parvum isolate [23, 24] because it is well characterized and is maintained by monthly propagation in newborn Cryptosporidium-free Holstein bull calves in our laboratory [25, 26] (Cryptosporidium Production Laboratory; https://acbs.cals.arizona.edu/crypto). Other established laboratories and commercial sources exist for obtaining purified C. parvum oocysts in the numbers required for calf trials including Bunch Grass Farm (Deary, ID; bunchgrassfarm@gmail.com). Alternatively, use the method described here to propagate C. parvum oocysts in calves and isolate oocysts from feces using published methods. Store oocysts in the saline/antibiotic solution the source laboratory ships them in (4 °C) for up to 60 days, but ideally use oocysts within 30 days of isolation for calf infection. All procedures involving C. parvum must be performed at Biosafety Level-2 (BSL-2) in an approved BSL-2 laboratory.
-
2.
Immediately prior to administration to calves, disinfect oocysts with 0.5% peracetic acid (4 °C) to inactivate any possible contaminant bacterial or viral pathogens [23, 27] (see Note 2). Peracetic acid is the preferred disinfectant as treatment of oocysts with diluted sodium hypochlorite (bleach) has been shown to promote spontaneous excystation at 37 °C [25, 27]. Use of hypochlorite-disinfected oocysts could potentially result in excystation in the abomasum of experimental calves and sporozoite killing by acidic conditions, effectively reducing the intended infectious dose [25]. In contrast, peracetic acid disinfection does not promote spontaneous excystation. All disinfection steps are performed at 4 °C. Centrifuge oocysts previously stored in saline/antibiotic solution (8000 × g, 7 min, 4 °C), remove saline/antibiotic solution, resuspend the oocyst pellet in PBS (4 °C) and wash oocysts with PBS twice. Then resuspend the pelleted oocysts thoroughly in 1–10 mL 0.5% peracetic acid (stock peracetic acid diluted in DI water to 0.5% vol/vol). Incubate resuspended oocysts at 4 °C for 3 min, inverting once each min. The 3 min timing period starts immediately upon addition of peracetic acid. After 3 min treatment, immediately pellet oocysts (8000 × g, 7 min, 4 °C), remove peracetic acid and wash 4× with PBS as described above. Keep oocysts at 4 °C at all times post-peracetic acid treatment until immediately prior to inoculation of calves.
-
3.
Following disinfection, determine percent oocyst excystation as a viability index and adjust the challenge dose if necessary (see Note 3). To determine percent excystation, resuspend a disinfected oocyst aliquot (~106 oocysts) in 250 μL excystation medium (1.5% taurocholic acid, 0.5% trypsin in PBS, pH 7.2–7.4) and place in a shaking water bath (1.5 h, 37 °C). At the end of the incubation, count the number of intact unexcysted oocysts and oocyst shells (fully/partially excysted oocysts) using a hemocytometer and phase microscopy. Divide the number of oocyst shells by the total number of oocyst shells plus intact oocysts and multiply by 100 to determine % excystation. Excystation is typically >95% for oocysts stored properly for up to 30 days following isolation and disinfection.
3.2 Procurement and Enrollment of Neonatal Calves for Therapeutic Efficacy Evaluation
-
1.
Trained veterinary staff obtain age-matched (born within a 12 h period) Holstein bull calves from a closed herd USDA-licensed dairy production unit, preferably the same source unit for all studies. Cohort size will vary depending on the investigator’s facility capacity for ABSL-2 calf isolation and source dairy average daily calving numbers. The minimum cohort size desired is six calves (three treated, three control) (see Note 4). With two such cohorts completed, data for six treated and six control calves are obtained, allowing potential exclusion of up to one calf per group without compromising statistical analyses in most cases. Occasionally such exclusions are required because of inadvertent coinfection with one or more other enteropathogens, need for euthanasia because of disease severity before completion of the study or other confounding variables. Trained laboratory staff manually assist birthing of calves for delivery onto a 10 mil plastic sheet barrier to minimize possible exposure to other enteropathogens or Cryptosporidium isolates or species (see Note 5). Because newborn calves are wet and difficult to securely hold, use clean thick cotton terrycloth towels to grasp calves during delivery. Calves from cows which experience dystocia or prolonged calving, or twin calves are not accepted. Weigh and perform a physical exam on each calf, including careful examination for congenital anomalies such as imperforate anus, cleft palate, and limb abnormalities. Calves weighing ≥38 kg and having normal physical exam findings are the most suitable for use in the method described here; calves weighing <38 kg are excluded (see Note 6). Place acceptable calves into a previously disinfected wheelbarrow for transport to a pre-disinfected designated concrete area. Disinfect the wheelbarrow between use for each calf. Wash any body parts, especially the muzzle and head region, with 7% iodine scrub and warm water if necessary to remove any exogenous material, then dry with a clean towel. Clean both sides of one ear with 7% iodine scrub and rinse, then apply a numbered ear tag to enrolled calves to serve as the calf’s identifying number. Record date and time of birth. Dip the navel in 10% iodine solution (not scrub), again after colostrum replacer is fed, again on arrival at the ABSL-2 facility and again 24 h after arrival. Orally administer to each calf Ecolizer (Clostridium perfringens Type C antitoxin and anti-Escherichia coli antibody, Novartis, Larchwood, IA) and CalfGuard vaccine (attenuated bovine rotavirus and coronavirus, Zoetis, Kalamazoo, MI) within 20 min of birth, and 1 h prior to feeding colostrum replacer per manufacturer’s instructions. Commencing 1 h after administration of the preceding antibodies and vaccine, feed enrolled calves commercial colostrum replacer from a single lot by nipple bottle (see Note 7), continuing until 6 h after birth at twice the manufacturer’s recommended calf dose reconstituted in 2 L of water (see Notes 8 and 9). Record actual time and volume of colostrum replacer intake hourly to confirm optimal full dosing is achieved within 6 h after birth. If a calf will not voluntarily consume the full amount of colostrum replacer within 6 h of birth, attempt to nipple bottle-feed the remainder within 9 h of birth (see Note 10). If a calf will not voluntarily consume the full amount of colostrum replacer within 9 h of birth, carefully feed the remainder using an esophageal tube feeder [28] (see Note 11).
-
2.
Place calves into disinfected transport crates (crates for 90–125 pound dogs) with autoclaved straw bedding for transport by cargo van to ABSL-2 Facilities. Disinfect calf rooms and allow them to air dry for at least 3 days prior to and after each experiment to inactivate any residual Cryptosporidium or other microbial agents. Upon arrival, assign calves to either treatment or control groups using a randomization method such as Microsoft Excel Random Number Generation Tool, then place calves into individual elevated calf stalls (Wenke Manufacturing, Pender, NE), equipped with coated slat flooring material (9 gauge flat expanded metal with rubberized coating and diamond-shaped openings) (see Note 12). House treatment and control groups in separate ABSL-2 rooms. Facilities will vary between institutions but we house two to three calves per room (~3 m wide by ~5 m long), allowing placement of elevated stalls such that the calves face each other for environmental enrichment but at distances that do not allow direct contact between calves. In instances when only a single calf is housed per room, place a mirror at eye level on the wall in front of the calf for environmental enrichment.
-
3.
Using a nipple bottle, feed calves non-medicated milk replacer (crude protein ~22% [bovine whey and milk-derived], crude fat ~20%) twice daily commencing at 12 h of age (volume equivalent to 10% of birth weight total per day divided into 2 feedings, 12 h apart through 5 days of age, increased by 25% at 6 days of age and increased again by 25% at 8 days of age) until the end of the experiment at 10 DPI (see Note 13). Allow 25–30 min per feeding for calves to consume the entire volume of milk replacer. Record the actual quantity of milk replacer consumed at each feeding. If a calf does not voluntarily consume any milk replacer, carefully feed the calculated volume of replacer using an esophageal tube feeder [28] (see Note 14). Clean and disinfect all nipple bottles, buckets, and utensils used for replacer reconstitution and feeding after each use.
-
4.
At 24 h of age administer vitamin E/selenium supplement (3 mL/45 kg) subcutaneously. Collect a blood sample by venipuncture (~10 mL), isolate the serum fraction, and test serum to verify adequate passive transfer of colostral IgG using a rapid method such as serum refractometry to semi-quantitatively assess serum IgG levels [29, 30] (see Note 15).
-
5.
At 36 h of age, perform another physical examination on each calf prior to final clearance and admittance into the study. Remove any unhealthy calves from the study (exclusion criteria: fever >103.0 °F, diarrhea, respiratory distress, inappetence, or inability to rise on own). Prior to experimental infection, examine fecal smears from each calf for the potential presence of Cryptosporidium oocysts by immunofluorescence assay (IFA) [31]. Remove any calves from the study that are positive for inadvertent field acquired Cryptosporidium infection.
3.3 Infection of Calves with C. parvum and Administration of Candidate Therapeutic Agents
-
1.
Choose an optimal time for personnel to infect calves such that at the time of inoculation no calves in the cohort are younger than 36 h of age and no calves are older than 48 h of age. Following acclimation, at the chosen time between 36 and 48 h of age (defined as DPI 0), orally administer disinfected oocysts (see Subheading 3.1) to calves as follows. While the calf is standing, allow each calf to suckle milk replacer (250 mL) from a nipple bottle to close the esophageal (gastric) groove and thus bypass the rumen for delivery of the inoculum directly into the abomasum [28]. Immediately thereafter, orally administer to each calf 5 × 107 viable, peracetic acid-disinfected C. parvum oocysts previously enumerated using a hemocytometer and prepared as follows. Prior to use, keep the oocyst inoculum for each calf in ~5 mL PBS at 4 °C in a 15-mL centrifuge tube. Immediately prior to inoculation, allow the inoculum to gradually reach room temperature over a ~10 min period to avoid thermal shock, then vortex the tube to resuspend oocysts. Immediately draw up the inoculum into a 50 cc blunt-ended catheter tip dosing syringe, equipped with a 15 cm Nalgene tube (~2 mm inside diameter) to facilitate recovery of the entire inoculum. Rinse/vortex the oocyst tube once with 5 mL PBS and draw up the rinse into the same 50 cc syringe. Finally, draw up ~20 mL milk replacer (at room temperature) into the syringe and mix by inversion immediately prior to calf inoculation. For clarity, this is the final inoculum for one calf. For each additional calf, the inoculum is identically prepared using a new disposable dosing syringe. Administer the inoculum immediately following the closure of the esophageal (gastric) groove as described above by orally inserting the dosing syringe so that the tip is at the base of the tongue, while the calf is still in the suckling response. With the head elevated to optimize the delivery of the entire inoculum, allow natural suckling of the syringe contents, facilitated by gradual manual expulsion. Administer the inoculum at a rate that does not allow any dripping from the calf’s mouth (see Note 16). Reload the syringe once with ~25 mL milk replacer as a rinse and repeat the administration procedure. Immediately thereafter, feed each calf the calculated volume of milk replacer to meet daily dietary requirements as described above (Subheading 3.2, step 3) and to ensure that the full inoculum reaches the abomasum. Examine fecal samples for oocysts by IFA daily following infection to determine pre-patent and patent periods.
-
2.
Initial administration of a given therapeutic candidate begins on DPI 2, at which time untreated C. parvum infection is established and nearing completion of one round of the life cycle at the infection dose used [19]. The candidate therapeutic must be prepared according to the institution’s Standard Operating Procedures for Preparation of Compounds for Use in Animals and be approved by the IACUC prior to administration. The dosage and frequency of dosing for most candidate therapeutics in the calf model can be initially based on mg/kg extrapolation from the most efficacious dosage regimens identified in C. parvum-infected mice, allometric modeling in mice and rats, and ultimately pharmacokinetic/pharmacodynamic studies in uninfected and infected newborn calves [11]. Preliminary Pharmacokinetics/Absorption-Distribution-Metabolism-Elimination studies may be performed on treated calves in a given trial to evaluate a candidate therapeutic, if additional stress can be minimized, and control (vehicle only) calves are identically sampled. Of potential relevance to desirable pharmacokinetic/pharmacodynamic properties of candidate chemotherapeutics, it was recently shown that intestinal (vs systemic) exposure is essential for the efficacy of bumped kinase inhibitor drugs against C. parvum in mouse models [32]. Treat control calves identically for the regimen selected with vehicle alone. Code by label the therapeutic (in vehicle) being evaluated, and vehicle alone, to blind the treatment and control preparations. Just prior to each treatment, allow each calf to suckle milk replacer (~475 mL) from a nipple bottle to close the esophageal (gastric) groove. Then feed each calf by nipple bottle the candidate therapeutic in vehicle, or vehicle alone, mixed well with milk replacer in a final volume of ~475 mL. Following each treatment, feed each calf the calculated volume of milk replacer to meet daily dietary requirements as described above (Subheading 3.2, step 3). Record all treatments with the therapeutic or vehicle alone. Make potable water available to all calves by bucket ad libitum for the entire experiment. At the earliest onset of diarrhea, make an oral electrolyte solution available to each calf by bucket for the remainder of the experiment. At each feeding, record the quantity of water and oral electrolytes consumed from buckets since the previous feeding, clean both buckets, and fill each with fresh water or electrolytes.
3.4 Stall Modifications for Accurate Evaluation of Diarrhea Severity, Parasite Shedding, and Urine Production in Infected Calves
-
1.
To ensure collection of all feces from individual calves for accurate total daily fecal volume quantitation and daily fecal oocyst count determinations, place three plastic fecal collection bins beneath the rear of each stall, held together by binder clips. Position fecal bins between the room wall and rear part of stall such that broad coverage is provided for all likely directions diarrhea may project (Fig. 1).
-
2.
Prevent contamination of feces with urine by using only bull calves (birth weight ≥38 kg); and a downward angled 6 mil plastic sheet spanning the underside of the full width of the stall floor, extending forward from the front of fecal collection bins, to divert urine into a separate bin positioned beneath the front of each stall (Fig. 1). Adjust the position of the plastic sheet if needed based on calf size so that urine is diverted but feces are allowed to pass into fecal collection bins. Tightly secure the plastic sheet to avoid leakage with reinforced water-proof industrial strength adhesive tape (Fig. 1) (see Notes 6 and 17). All collection bins and urine diversion shields are most conveniently set up the day prior to calf arrival.
-
3.
Loose stools or diarrhea typically commence between 48 and 72 h PI in this model. Determine total fecal volume and fecal oocyst counts daily for each calf from 3 DPI until the end of the experiment as described in Subheading 3.6. Use extreme care and adequate personal protective equipment to prevent zoonotic infection (see Notes 18 and 19).
(a) Elevated calf stall depicting urine collection bin and plastic urine diversion sheet placement, viewed from front. (b) Stall depicting fecal collection bins and plastic urine diversion sheet placement, viewed from rear. (c, d) Newborn 41 kg Holstein bull calf in stall ~1 h following arrival at ABSL-2 facility, prior to infection
3.5 Evaluation of Clinical Health, Diarrhea, and Oocyst Shedding in Infected Calves
-
1.
Once the study has commenced, collect diarrheic fecal samples from each calf (~30 mL/calf) and have them examined for the presence of enteropathogenic bacteria (K99+ E. coli, Clostridium spp. and Salmonella spp.). Perform these tests on fecal samples collected after two consecutive episodes of diarrhea. Immediately remove from the study and exclude from analyses any calves found positive for other enteropathogens which would confound interpretation of the experimental results. Collect additional fecal samples from all calves at the completion of the experiment and reexamine for presence of the enteropathogens above. Exclude any positive calves from analyses (see Note 20).
-
2.
Commencing 3 DPI, for the duration of the experiment, have trained veterinary clinical staff assess clinical health parameters on each calf twice daily (every 12 h) and assign an objective numerical score for each parameter. Blind personnel involved in the study as to the identity (treatment or control) of calves (single-blind study). Assign and record individual scores to each calf for (1) fecal consistency, (2) willingness to rise, (3) stance when up in stall, (4) appetite, (5) attitude, and (6) hydration status [11, 12, 33] (see Note 21). Determine the mean daily clinical health score using individual parameter scores for each calf. Determine rectal temperature once daily. Contact the attending veterinarian on call if any of the following are observed: (1) pain and/or distress (grinding teeth, grunting, kicking at abdomen, abnormal vocalizations), (2) severe watery profuse diarrhea or bloody diarrhea, (3) moderate or severe dehydration, (4) high fever (>103.5 °F) or hypothermia (<96 °F), (5) weight loss exceeding 10%, (6) depressed mental state, minimally responsive or otherwise appearing in extremis, (7) inability to stand, or (8) inability to suckle. In such cases, the attending veterinarian makes all decisions on appropriate supportive treatment(s) or whether euthanasia is required. Treat fever (≥103.5 °F) and/or symptoms of pain with palliative therapy such as injectable flunixin meglumine under direction of the attending veterinarian (see Note 22). Treat moderate dehydration at its very earliest onset with parenteral rehydration under direction of the attending veterinarian to prevent progression to severe dehydration (Table 1). Record the use of any concomitant medications and parenteral fluid therapy in the records for each calf.
-
3.
As an additional index of hydration status, measure total daily urine output by each calf 3–10 DPI. Based on estimated volume in the urine collection bin for each calf, pour all urine into the appropriate size graduated cylinder to determine the actual volume of both AM and PM collections separately. Combine the volumes to determine the total daily urine volume for each calf and record the values. Disinfect and rinse the urine collection bin, then dry and place the bin back under the stall, positioned as previously.
-
4.
On 3–10 DPI, measure and evaluate total daily fecal volume (mL) and consistency for each calf to accurately determine diarrhea severity and oocyst numbers produced daily (see Note 23). When caring for calves at AM and PM time points, complete fecal collection and assessment of clinical health parameters prior to feeding (see Note 24). Calves typically rise and stand prior to feeding, which facilitates fecal collection and clinical assessment (see Note 25). Measure the total daily fecal volume (combined AM and PM collections) just prior to the PM feeding as described in Subheading 3.6. Thoroughly clean and mop calf room floors with quaternary ammonium-based disinfectant after procedures are completed each AM and PM.
-
5.
Accurately quantify the total number of oocysts shed per day (3–10 DPI) from each calf as follows. Using a commercial grade blender, thoroughly blend the total daily fecal collection from each calf to homogeneity and to ensure the release of oocysts trapped in any clumps of excess mucus (detailed in Subheading 3.6, step 3). Once homogenized, collect a 50 mL sample, representative of the total volume, and store at 4 °C for oocyst quantitation as described below (Subheading 3.8). Transport fecal samples from the ABSL-2 facility to the BSL-2 laboratory for analyses in a closed container labeled with a biohazard sticker.
3.6 Collection and Processing of Feces
-
1.
Using a scraper, collect any feces on the floor that may have missed the collection bins and place into the corresponding calf fecal bins. Use a plastic spatula to gently scrape any feces on the plastic urine diversion sheets taking care that no tears are created.
-
2.
Based on estimated volume in the three collection pans for each calf, pour all feces into the appropriate size graduated cylinder to determine the actual volume of both AM and PM collections, separately. Just prior to the PM feeding, combine the AM and PM fecal collections to determine the total daily fecal volume for each calf and record this value. Disinfect and rinse out fecal collection bins. Dry the bins and place them back under the stall, positioned as previously, or adjusted if needed.
-
3.
Blend to homogeneity all feces collected over successive 24 h periods from each calf in a commercial blender. Blend on the low speed setting for 5 min with the blender lid locked on securely. Place the blender on the floor undisturbed for ~5 min before unlocking and removing the lid to reduce aerosol risks. If the total daily fecal volume for any calf is near or greater than the 4 L blender capacity, split the volume in two and blend each separately as described above. After blending, then thoroughly mix the two using two 4 L size buckets and pouring back and forth at least five times. Immediately following completion of blending/mixing steps, collect a representative ~50 mL fecal sample from the mid-point of the container using a ladle, and place the sample into a fecal specimen container (urinalysis cup) pre-labeled with date and calf #. The blending and mixing processes create aerosols. Take extreme precautions to avoid zoonotic infection.
-
4.
Wash the blender thoroughly with hot water and dish detergent followed by disinfection and rinse well between processing feces from each calf.
3.7 Terminal Procedures and Euthanasia (see Note 26)
-
1.
At 10 DPI, following the AM clinical health, diarrhea and oocyst shedding evaluations described above (Subheading 3.5), sedate each calf by intramuscular injection of xylazine (3 mg/kg) combined with ketamine (100 mg/calf). Following sedation, collect blood samples from each calf into appropriate tubes for performance of CBCs and serum chemistry panels to evaluate clinical pathology and screen for potential toxicity of the test therapeutic.
-
2.
Euthanize each sedated calf by intracardiac injection of euthanasia solution (1 mL/10 lb; 1 mL/4.5 kg). This method (Subheading 3.7, steps 1 and 2) is in accordance with the AVMA Guidelines on Euthanasia and euthanasia recommendations approved by the local IACUC. If clinically indicated before 10 DPI, as determined by the attending veterinarian, use the same euthanasia procedure.
-
3.
Following euthanasia, weigh each calf for comparison to birth weight to compute average body weight gain or loss.
3.8 Determination of Daily Fecal Oocyst Counts from Infected Calves
Determine total daily fecal oocyst counts by real-time PCR (qPCR) as described previously [11, 34]. This step is typically performed following completion of a calf trial.
-
1.
For each fecal sample, extract oocyst DNA using the QIAamp® Fast DNA stool mini kit (Qiagen, Gaithersburg, MD). Add InhibitEx buffer, incubate at 95 °C (5 min), then perform 5 freeze-thaw cycles. Quantify total DNA in the sample by Nanodrop® (Nanodrop Technologies, Wilmington, DE). We use the C. parvum oocyst wall protein gene (COWP) (Genbank no. AF248743) as the target for primers (COWPF, 5′-CAAATTGATACCGTTTGTCCTTCTG-3′; COWPR, 5′-AGCTGAATTAGAATCGACATGCC-3′) and selected a 151 bp sequence from the COWP gene. For each qPCR, prepare a 25 μL reaction containing 400 nM (final concentration) for each primer, 12.5 μL SYBR-green or similar nucleic acid stain and 0.1 ng/μL bovine serum albumin. Add genomic DNA (2 μL) and perform the PCR in a Real-Time PCR System. Use cycling conditions of 10 min incubation at 95 °C followed by 50 cycles at 95 °C for 15 s and 60 °C for 1 min and a final extension at 72 °C for 1 min. Run each sample in triplicate. Concurrently run a control with no template and verify it to be negative. To determine the total number of oocysts shed per day, multiply the oocyst count/mL derived by comparison to standards run concurrently during the qPCR, times the total daily fecal volume (mL).
3.9 Statistical Analyses
For statistical analyses, examine all calves given the same treatment (therapeutic candidate or vehicle alone control) as one group for evaluation of all outcome parameter means. Examine clinical health scores, total fecal volumes, total oocyst counts, total urine production, and body weight gain/loss for statistically significant differences using Student’s t test or another preferred statistically valid method. Additional or more powerful statistical analyses are usually not necessary to validate clinically acceptable efficacy of candidate therapeutics.
4 Notes
-
1.
Diurnal variations were observed in ten neonatal Holstein bull calves we used previously for oocyst propagation/isolation, obtained, maintained, and housed as described above and identically infected with 5 × 107 C. parvum oocysts (Iowa) at 36–48 h of age [11]. In these propagation calves, total AM and total PM feces excreted by each calf were collected separately each day, to prioritize and exclude any potential low count collections from laborious oocyst purification procedures. Using the oocyst quantitation methods described in Subheading 3, but before we adopted the use of a blender to homogenize feces, we observed that oocyst counts per gram of feces in AM and PM collections from an individual calf could vary by ten-fold or more on some days, up to 46-fold in one calf (Fig. 2a, b). We also observed grossly that calves produced highly variable amounts of mucus in feces. We observed microscopically that large numbers (wall to wall sheets) of oocysts were entrapped in mucus in such cases, while more watery fecal components were often only sparsely populated with oocysts. Whether the observed oocyst count variations in AM vs PM collections represent true diurnal variation or skewing of oocyst counts by entrapment of oocysts in fecal mucus produced by some calves is unclear. Nevertheless, based on these observations, we have since used uniformly blended total daily fecal collections (AM and PM combined) to obtain a representative sample for accurate oocyst quantitation. An industrial grade blender is used to ensure that oocysts trapped in clumps of mucus are released and that daily fecal collections from each calf are thoroughly blended to homogeneity before taking a representative sample for oocyst quantitation (# oocysts/mL) and back calculation using total fecal volume (mL) to determine the total number of oocysts shed per day.
-
2.
Peracetic acid is highly toxic and explosive. Follow all precautions stated in the MSDS.
-
3.
Use % excystation to adjust the number of oocysts in the inoculum to deliver 5 × 107 viable oocysts/calf. For example, if percent excystation is 94%, adjust the oocyst inoculum dose/calf from 5 × 107 to 5.3 × 107.
-
4.
Occasionally, the desired number of age-matched calves for a cohort cannot be obtained (such as six calves total to provide three calves each for the treatment and control groups). If only 3–5 age-matched calves are obtained, the cohort can proceed, as long as one calf is a control (vehicle alone).
-
5.
Dairy facilities vary in their willingness to allow laboratory personnel to manually assist delivery of calves on-site because of biosecurity and/or liability concerns for potential personal injury. In such cases, accept only calves for which dairy personnel have manually assisted delivery onto the plastic sheet barrier, then placed into a disinfected wheelbarrow for transport to the designated disinfected concrete area where laboratory personnel can determine acceptability and process acceptable calves further. If there is any inadvertent minimal soiling of otherwise acceptable calves, calves are thoroughly cleaned with 7% iodine scrub and towel dried.
-
6.
Calves have room to rise/lie down and move/maneuver within the stall and may be able to turn completely around and reverse their position in the stall. This is most likely to occur if smaller calves <32 kg are used, during the first few days acclimating to stalls, prior to infection and onset of diarrhea. If calves turn themselves around in the stall such that their posterior is at the front of the stall, reposition them properly. However, in such cases, most of the feces excreted during the previous 12-h period will have ended up in the urine collection bin. If the feces are normal or loose but not diarrheic, urine tends to float on top of the feces. In such cases, carefully pour or aspirate off urine to allow fecal collection. If the feces are diarrheic, there is mixing with urine and the collection is essentially lost for evaluation and noted in the record as such. However, we have rarely (~1 in 50 calves) observed calves turning around in the stall when larger calves ≥38 kg are used, and this is the primary reason calves <38 kg are excluded. Needless to say but stated to ensure absolute clarity, never use the headlock between 12-h periods to prevent calves from turning around in the stall. This would be grossly inhumane and constitute animal abuse, prevent the calf from laying down, and result in death from asphyxiation if the calf is unable to stand. Also never use the front head gate bars to headlock a calf for more than ~5 min, if at all. The headlock is intended strictly to facilitate brief restraint for blood draws, etc.
-
7.
Some calves suckle so intensely that a vacuum may form in the bottle during nursing, eventually precluding additional ingestion. Only use nipple bottles that incorporate a ~1 mm diameter air release valve port at the nipple base to allow air to enter the bottle as the calf is nursing, thus precluding vacuum formation. If necessary, massage or press next to the valve port to release any vacuum. After feeding is completed verify that the valve is not plugged due to inadequate cleaning and is working properly.
-
8.
Colostrum replacer powder does not go into solution easily. To thoroughly reconstitute and solubilize colostrum replacer, gradually add the specified amount of powder per calf (twice the manufacturer’s recommended dose, or 2 packets totaling 940 g powder) to a 6-L bucket containing 2 L of clean tap water at 110–120 °F using a manual whisk. It is critical to whisk the preparation during reconstitution until no visible clumps remain. Following consumption of the full dose of colostrum replacer, add ~250 mL clean warm water to the same nipple bottle, swirl vigorously to rinse residual colostrum replacer, and feed this to the calf to ensure complete dosing.
-
9.
Bovine colostrum contains variable titers of antibody reactive with C. parvum, acquired from natural exposure or previous infection. However, no significant neutralizing antibody is present following previous infection as normal colostrum-fed calves are readily infected with C. parvum. Nevertheless, while expensive, commercial colostrum replacer is used to eliminate this variable in entirety. A commercial colostrum replacer such as the one we use has been formulated to replace maternal colostrum and negate lot to lot and inherent variability found in source dairy-acquired colostrum (bovine IgG colostrum replacer, Land O’Lakes, Shoreview, MN). Frozen whole colostrum acquired from most source dairies varies substantially in antibody content, quality, and microbial contamination load, and should be avoided.
-
10.
Calves are born agammaglobulinemic. They require colostral antibodies following birth for passive transfer of immunity against the major enteropathogenic bacteria and viruses responsible for neonatal diarrhea and mortality for which commercially available maternal vaccines exist (there is presently no commercially available maternal vaccine for Cryptosporidium). The newborn calf’s ability to absorb ingested colostral antibody decreases linearly over the first 24 h of age during the process of gut closure. By 12 h of age, the reduction is substantial and by 24 h of age, the gut is essentially closed to absorption of colostral antibody and other macromolecules. For this reason, ensure that calves suckle the majority of the recommended colostrum replacer dose, preferably within 6 h after birth but no later than 9 h after birth. Feed any colostrum replacer remaining at 9 h after birth by esophageal intubation.
-
11.
Feeding colostrum replacer by esophageal tube should be used as a last resort due to the fact that intubating (unlike suckling) does not stimulate the esophageal (gastric) groove closure reflex and thus delivers replacer into the rumen instead of the abomasum [28].
-
12.
Adjust the width of the stall’s front head gate bars to allow only the head to have free access through the bars. This will allow calves to easily access water and/or electrolyte buckets, while also preventing a calf from jumping through the front of the stall and potentially getting trapped or injured. This potential problem is uncommon and typically occurs only if smaller calves <32 kg are used and the head gate bars are improperly positioned. We have never observed this problem using calves ≥38 kg with head gate bars positioned properly. Other than bruising acquired by two small 30–32 kg calves jumping through the front of the stall, we have also never had a calf acquire any injury being housed in elevated stalls. Nevertheless, it is important after assembling newly purchased stalls to file down any sharp or jagged edges on the framing or exposed hardware. Periodically inspect stalls for the same and to ensure that all hardware fasteners are securely tightened to maintain stall stability. Periodically inspect the rubberized flooring for wear and deterioration from use of harsh disinfectants and replace when necessary.
-
13.
Similar to colostrum replacer, milk replacer powder does not go into solution easily. Use warm (110–120 °F) water and a whisk to thoroughly reconstitute replacer until all clumps are fully dissolved.
-
14.
Feed milk replacer via esophageal tube as a last resort measure for calves which will not consume any of the calculated volume of replacer in a ~25–30-min feeding period. The suckle response resulting in esophageal (gastric) groove closure is voided by tube feeding, delivering milk replacer into the rumen. Additionally, in our experience, calves which are tube fed more than ~3–4 times are reluctant to feed from a nipple bottle subsequently.
-
15.
Failure of passive transfer (FPT) of maternal immunoglobulins is rare if commercial colostrum replacer (at twice the label dose) is suckled within 6-9 h of birth. However, if FPT occurs, but the calf is otherwise healthy at 24 h of age, treat it by intravenous transfusion of commercially available adult bovine plasma (Lake Immunogenics, Ontario, NY) administered under supervision by a veterinarian.
-
16.
We have never experienced a calf not receiving the entire oocyst inoculum using the method described, but it could potentially happen (leakage, expectoration). If this occurs, note in the records the estimated volume of inoculum not received and that data from the calf may not be suitable for use in final analyses.
-
17.
It is potentially possible that some urine may enter the fecal collection bins, voiding accurate fecal volume determination. This possibility is largely eliminated if the plastic diversion sheet is stretched tightly against the bottom at the rear third of the stall and properly secured with reinforced waterproof industrial strength adhesive tape. This ensures that urine flows only in one direction, toward the front of the stall and into the urine collection bin. This is also a secondary reason calves <38 kg are excluded, as smaller calves can move back and forth in the stall to a greater extent and make accurate placement of the plastic diversion sheet difficult, especially for calves <32 kg.
-
18.
Calves infected with C. parvum in this model shed extremely large numbers of oocysts, especially the untreated controls. A single experimentally infected newborn calf may shed >1012 oocysts in feces during the peak days of diarrhea [11, 13]. Thus, personnel caring for calves are at high risk of zoonotic infection unless appropriate precautions are taken and adequate personal protective equipment is used while in calf rooms, minimally (1) disposable double gloves, (2) mid-calf high plastic or rubber boots over disposable plastic shoe covers, (3) Tyvek coveralls with elastic cinched ankle and wrist cuffs, (4) N95 respirators, (5) disposable hair bonnets, completely covering all hair (long hair must be tied back into a bun), and (6) goggles, safety glasses, or full face shields.
-
19.
An institutional protocol should be in place for evaluation of any calf personnel which develop nausea, vomiting, or diarrhea during or after a trial to determine the etiology and appropriate treatment. We use the University’s Occupational Health Division for independent assessment of ill personnel and compliance with HIPPA. If C. parvum is identified as the etiologic agent the experimental protocol should be carefully reviewed to determine where the breach leading to zoonotic transmission likely occurred so that it can be addressed. Despite the precautions described here, we have had at least one documented case of zoonotic transmission.
-
20.
Adhering closely to the methods described here for calf procurement, we have never had a calf inadvertently infected with a field isolate of C. parvum, and have had only four calves in the last ~100 used inadvertently infected with field acquired enteropathogenic bacteria.
-
21.
We use a standardized daily AM/PM form for each calf that has all health evaluation parameters listed along with the scoring scale for each to record consensus scores; rectal temperature; amount of milk replacer, water and/or oral electrolytes consumed; date and actual AM/PM times (h, min) data were recorded, and calf ear tag #, with a signature box for each of the two attending staff involved (Daily Health Observation Record). Standardized forms are also used for all other information described in methods for which it is stated that records are made (Newborn Calf Record, Cryptosporidium Infection Record, Daily Fecal Volume Record, Test-Therapeutic Dosing Record, Concomitant Treatment Record, and Condition(s) Requiring Examination by the Attending Veterinarian Record).
-
22.
The nonsteroidal anti-inflammatory drug flunixin meglumine should be used sparingly, and only when absolutely needed. No more than three doses total during a trial period should be administered to a given experimental calf to avoid nephrotoxicity and gastrointestinal toxicity. Toxicity is of greatest concern when administered to dehydrated calves.
-
23.
Fecal dry matter percentages may optionally be determined on total daily fecal collections as an additional index of diarrhea severity. However, in the model presented here, we found previously that fecal dry matter percentages added little to fecal consistency scores and total daily fecal volumes in determining diarrhea severity and have since discontinued percent dry matter determinations.
-
24.
Calves with diarrhea are prone to cutaneous scalding in the perianal and tail base regions. Use human infant sanitary wipes or warm wet paper towels to gently clean these regions as needed. If indicated, apply generic human infant diaper rash ointment liberally after cleaning the region. In such cases, this should be done prior to feeding or taking rectal temperature, both of which stimulate defecation.
-
25.
When calves are reluctant but able to stand for evaluation and feeding, rapidly and repeatedly stroke the hair coat from the hip region toward the shoulders. This is usually effective in getting the calf to stand. Alternatively, grasp the hip region and gently rock the calf back and forth laterally to stimulate initiation of the standing motion.
-
26.
The drugs used for sedation and euthanasia are controlled (scheduled) substances. A DEA license is required to obtain these. If the investigator does not have a DEA license, obtain the drugs through the attending veterinarian and comply with all record keeping and other requirements.
Diurnal variation in oocyst shedding in C. parvum-infected calves. (a) Total AM and total PM feces excreted by each calf were collected separately each day for oocyst quantitation. (b) AM and PM oocyst counts per gram of feces from individual calves varied by 10-fold or more on some days, up to 46-fold in one calf. Reproduced in part (data for calves 1–5) from [11] by permission of Oxford University Press. Additional calf data demonstrating diurnal variation in oocyst shedding in identically infected calves used for C. parvum oocyst propagation (calves 6–10) are newly reported here
References
Tzipori S, Widmer G (2008) A hundred-year retrospective on cryptosporidiosis. Trends Parasitol 24:184–189. https://doi.org/10.1016/j.pt.2008.01.002
Kotloff KL, Nataro JP, Blackwelder WC, Nasrin D, Farag TH, Panchalingam S, Wu Y, Sow SO, Sur D, Breiman RF, Faruque AS, Zaidi AK, Saha D, Alonso PL, Tamboura B, Sanogo D, Onwuchekwa U, Manna B, Ramamurthy T, Kanungo S, Ochieng JB, Omore R, Oundo JO, Hossain A, Das SK, Ahmed S, Qureshi S, Quadri F, Adegbola RA, Antonio M, Hossain MJ, Akinsola A, Mandomando I, Nhampossa T, Acacio S, Biswas K, O’Reilly CE, Mintz ED, Berkeley LY, Muhsen K, Sommerfelt H, Robins-Browne RM, Levine MM (2013) Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study. Lancet 382:209–222. https://doi.org/10.1016/S0140-6736(13)60844-2
Wyatt CR, Riggs MW, Fayer R (2010) Cryptosporidiosis in neonatal calves. Vet Clin North Am Food Anim Pract 26:89–103
Stockdale HD, Spencer JA, Blagburn BL (2008) Prophylaxis and chemotherapy. In: Fayer R, Xiao L (eds) Cryptosporidium and cryptosporidiosis, 2nd edn. CRC Press, Boca Raton, FL
Cabada MM, White AC (2010) Treatment of cryptosporidiosis: do we know what we think we know? Curr Opin Infect Dis 23:494–499
Amadi B, Mwiya M, Sianongo S, Payne L, Watuka A, Katubulushi M, Kelly P (2009) High dose prolonged treatment with nitazoxanide is not effective for cryptosporidiosis in HIV positive Zambian children: a randomised controlled trial. BMC Infect Dis 9:195. https://doi.org/10.1186/1471-2334-9-195
Amadi B, Mwiya M, Musuku J, Watuka A, Sianongo S, Ayoub A, Kelly P (2002) Effect of nitazoxanide on morbidity and mortality in Zambian children with cryptosporidiosis: a randomised controlled trial. Lancet 360:1375–1380. https://doi.org/10.1016/S0140-6736(02)11401-2
Santin M, Trout JM (2008) Livestock. In: Fayer R, Xiao L (eds) Cryptosporidium and cryptosporidiosis, 2nd edn. CRC Press, Boca Raton, FL
Heinrichs AJ (2005) Rumen development in the dairy calf. Adv Dairy Technol 17:179–188
Cirle A, Guerrant RL (2008) Clinical disease and pathology. In: Fayer R, Xiao L (eds) Cryptosporidium and cryptosporidiosis, 2nd edn. CRC Press, Boca Raton, FL
Schaefer DA, Betzer DP, Smith KD, Millman ZG, Michalski HC, Menchaca SE, Zambriski JA, Ojo KK, Hulverson MA, Arnold SL, Rivas KL, Vidadala RS, Huang W, Barrett LK, Maly DJ, Fan E, Van Voorhis WC, Riggs MW (2016) Novel bumped kinase inhibitors are safe and effective therapeutics in the calf clinical model for cryptosporidiosis. J Infect Dis 15(214):1856–1864. https://doi.org/10.1093/infdis/jiw488
Imboden M, Schaefer DA, Bremel RD, Homan EJ, Riggs MW (2012) Antibody fusions reduce onset of experimental Cryptosporidium parvum infection in calves. Vet Parasitol 188(1–2):41–47. https://doi.org/10.1016/j.vetpar.2012.02.014
Perryman LE, Kapil SJ, Jones ML, Hunt EL (1999) Protection of calves against cryptosporidiosis with immune bovine colostrum induced by a Cryptosporidium parvum recombinant protein. Vaccine 17:2142–2149
Ollivett TL, Nydam DV, Bowman DD, Zambriski JA, Bellosa ML, Linden TC, Divers TJ (2009) Effect of nitazoxanide on cryptosporidiosis in experimentally infected neonatal dairy calves. J Dairy Sci 92:1643–1648. https://doi.org/10.3168/jds.2008-1474
Schnyder ML, Kohler L, Hemphill A, Deplazes P (2009) Prophylactic and therapeutic efficacy of nitazoxanide against Cryptosporidium parvum in experimentally challenged neonatal calves. Vet Parasitol 160:149–154. https://doi.org/10.1016/j.vetpar.2008.10.094
Fayer R, Ellis W (1993) Paromomycin is effective as prophylaxis for cryptosporidiosis in dairy calves. J Parasitol 79:771–774
Hulverson MA, Choi R, Arnold SLM, Schaefer DA, Hemphill A, McCloskey MC, Betzer DP, Muller J, Vidadala RSR, Whitman GR, Rivas KL, Barrett LK, Hackman RC, Love MS, McNamara CW, Shaughnessy TK, Kondratiuk A, Kurnick M, Banfor PN, Lynch JJ, Freiberg GM, Kempf DJ, Maly DJ, Riggs MW, Ojo KK, Van Voorhis WC (2017) Advances in bumped kinase inhibitors for human and animal therapy for cryptosporidiosis. Int J Parasitol 47:753–763. https://doi.org/10.1016/j.ijpara.2017.08.006
Okhuysen PC, Chappell CL, Crabb J, Valdez LM, Douglass ET, DuPont HL (1998) Prophylactic effect of bovine anti-Cryptosporidium hyperimmune colostrum immunoglobulin in healthy volunteers challenged with Cryptosporidium parvum. Clin Infect Dis 26:1324–1329
Fayer R (2008) The general biology of Cryptosporidium. In: Fayer R, Xiao L (eds) Cryptosporidium and cryptosporidiosis, 2nd edn. CRC Press, Boca Raton, FL
Riggs MW (1987) Dissertation, Washington State University, Pullman, WA
Schaefer DA, Auerbach-Dixon BA, Riggs MW (2000) Characterization and formulation of multiple epitope-specific neutralizing monoclonal antibodies for passive immunization against cryptosporidiosis. Infect Immun 68:2608–2616. https://doi.org/10.1128/IAI.68.5.2608-2616.2000
Perryman LE, Jasmer DP, Riggs MW, Bohnet SG, McGuire TC, Arrowood MJ (1996) A cloned gene of Cryptosporidium parvum encodes neutralization-sensitive epitopes. Mol Biochem Parasitol 80:137–147
Heine J, Pohlenz JF, Moon HW, Woode GN (1984) Enteric lesions and diarrhea in gnotobiotic calves monoinfected with Cryptosporidium species. J Infect Dis 150:768–775
Abrahamsen MS, Templeton TJ, Enomoto S, Abrahante JE, Zhu G, Lancto CA, Deng M, Liu C, Widmer G, Tzipori S, Buck GA, Xu P, Bankier AT, Dear PH, Konfortov BA, Spriggs HF, Iyer L, Anantharaman V, Aravind L, Kapur V (2004) Complete genome sequence of the apicomplexan, Cryptosporidium parvum. Science 304:441–445
Riggs MW, Perryman LE (1987) Infectivity and neutralization of Cryptosporidium parvum sporozoites. Infect Immun 55:2081–2087
Riggs MW, Stone AL, Yount PA, Langer RC, Arrowood MJ, Bentley DL (1997) Protective monoclonal antibody defines a circumsporozoite-like glycoprotein exoantigen of Cryptosporidium parvum sporozoites and merozoites. J Immunol 158:1787–1795
Riggs MW, Cama VA, Leary JR, Sterling CR (1994) Bovine antibody against Cryptosporidium parvum elicits a circumsporozoite precipitate-like reaction and has immunotherapeutic effect against persistent cryptosporidiosis in SCID mice. Infect Immun 62:1927–1939
Jones CM, Heinrichs AJ (2003) Feeding the newborn dairy calf. In: Agricultural Research and Cooperative Extension Publications. Pennsylvania State University, State College, PA. Available at: https://extension.psu.edu/feeding-the-newborn-dairy-calf
Morrill KM, Polo J, Lago A, Campbell J, Quigley J, Tyler H (2013) Estimate of serum immunoglobulin G concentration using refractometry with or without caprylic acid fractionation. J Dairy Sci 96:4535–4541. https://doi.org/10.3168/jds.2012-5843
Hernandez D, Nydam DV, Godden SM, Bristol LS, Kryzer A, Ranum J, Schaefer D (2016) Brix refractometry in serum as a measure of failure of passive transfer compared to measured immunoglobulin G and total protein by refractometry in serum from dairy calves. Vet J 211:82–87
Riggs MW, Schaefer DA, Kapil SJ, Barley-Maloney L, Perryman LE (2002) Efficacy of monoclonal antibodies against defined antigens for passive immunotherapy of chronic gastrointestinal cryptosporidiosis. Antimicrob Agents Chemother 46:275–282. https://doi.org/10.1128/AAC.46.2.275-282.2002
Arnold SLM, Choi R, Hulverson MA, Schaefer DA, Vinayak S, Vidadala RSR, McCloskey MC, Whitman GR, Huang W, Barrett LK, Ojo KK, Fan E, Maly DJ, Riggs MW, Striepen B, Van Voorhis WC (2017) Necessity of bumped kinase inhibitor gastrointestinal exposure in treating Cryptosporidium infection. J Infect Dis 216:55–63
Constable PD, Walker PG, Morin DE, Foreman JH (1998) Clinical and laboratory assessment of hydration status of neonatal calves with diarrhea. J Am Vet Med Assoc 212:991–996
Guy RA, Payment P, Krull UJ, Horgen PA (2003) Real-time PCR for quantification of Giardia and Cryptosporidium in environmental water samples and sewage. Appl Environ Microbiol 69:5178–5185. https://doi.org/10.1128/AEM.69.9.5178-5185.2003
Acknowledgments
This work was supported by USDA NIFA Animal Health Project number ARZT-5704180-A50-121, The Bill and Melinda Gates Foundation Contract 44418, NIH grants R01 AI 111341 and R01 HD 080670, and USDA NIFA grant 2014-67015-22106.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Science+Business Media, LLC, part of Springer Nature
About this protocol
Cite this protocol
Riggs, M.W., Schaefer, D.A. (2020). Calf Clinical Model of Cryptosporidiosis for Efficacy Evaluation of Therapeutics. In: Mead, J., Arrowood, M. (eds) Cryptosporidium. Methods in Molecular Biology, vol 2052. Humana, New York, NY. https://doi.org/10.1007/978-1-4939-9748-0_15
Download citation
DOI: https://doi.org/10.1007/978-1-4939-9748-0_15
Published:
Publisher Name: Humana, New York, NY
Print ISBN: 978-1-4939-9747-3
Online ISBN: 978-1-4939-9748-0
eBook Packages: Springer Protocols