Abstract
Background
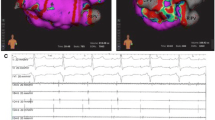
First experiences using a 64-electrode mini-basket catheter (BC) paired with an automatic mapping system (Rhythmia™) for catheter ablation (CA) of ventricular ectopy (VE) and ventricular tachycardia (VT) have been reported.
Objectives
We aimed to evaluate (1) differences in ventricular access for the BC and (2) benefit of this technology in the setting of standard clinical practice.
Methods
Patients (pts) undergoing CA for VE or VT using the Intellamap Orion™ paired with the Rhythmia™ automated-mapping system were included in this study. For LV access, transseptal and retrograde access were compared.
Results
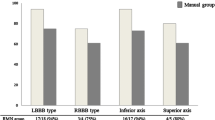
All 32 pts (29 men, age 63 ± 15 years) underwent CA for VE (17 pts) or VT (15 pts). For mapping of VE originating from the left ventricle (LV) in 10 out of 13 pts, a transaortic access was feasible. The predominant access for CA of VT was transaortic (5/7). Feasibility and safety seem to be equal. The total procedure time was 179.1 ± 21.2 min for VE ablation and 212.0 ± 71.7 min for VT ablation (p = 0.177). For VE, an acquisition of 1602 ± 1672 map points and annotation of 140 ± 98 automated mapping points sufficed to abolish VE in all pts. During a 6-month follow-up (FU) after CA for VE, a VE burden reduction from 18.5 ± 2.1% to 2.8 ± 2.2% (p = 0.019) was achieved. In VT pts, one patient showed recurrence of sustained VT episodes during FU.
Conclusion
Use of a high-resolution mapping system for VE/VT CA potentially facilitates revelation of VE origin and VT circuits in the setting of standard clinical practice. Feasibility and safety of a venous, transaortic, transseptal, or a combined approach seem to be equal.


Similar content being viewed by others
Abbreviations
- CA:
-
Catheter ablation
- VT:
-
Ventricular tachycardia
- VE:
-
Ventricular ectopy
- BC:
-
Mini-basket catheter
- LVEF:
-
Left ventricular ejection fraction
- ICD:
-
Internal cardioverter defibrillator
- LV:
-
Left ventricle
- RV:
-
Right ventricle
- RF:
-
Radiofrequency
- PVS:
-
Programmed ventricular stimulation
- FU:
-
Follow up
- AECG:
-
Automated electrograms
- AAD:
-
Antiarrhythmic drug therapy
- CHF:
-
Congestive heart failure
References
Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, et al. American College of Cardiology; American Heart Association Task Force; European Society of Cardiology Committee for practice guidelines. J Am Coll Cardiol. 2006;48:247–346.
Sacher F, Tedrow UB, Field ME, Raymond JM, Koplan BA, Epstein LM, et al. Ventricular tachycardia ablation: evolution of patients and procedures over 8 years. Circ Arrhythm Electrophysiol. 2008;1:153–61.
Dinov B, Fiedler L, Schönbauer R, Bollmann A, Rolf S, Piorkowski C, et al. Outcomes in catheter ablation of ventricular tachycardia in dilated nonischemic cardiomyopathy compared with ischemic cardiomyopathy: results from the prospective Heart Centre of Leipzig VT (HELP-VT) study. Circulation. 2014;129:728–36.
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the heart rhythm Society. J Am Coll Cardiol. 2018;72:e91–220.
Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36:2793–867.
Santangeli P, Frankel DS, Marchlinski FE. End points for ablation of scar-related ventricular tachycardia. Circ Arrhythm Electrophysiol. 2014;7:949–60.
Reddy VY, Reynolds MR, Neuzil P, Richardson AW, Taborsky M, Jongnarangsin K, et al. Prophylactic catheter ablation for the prevention of defibrillator therapy. N Engl J Med. 2007;357:2657–65.
Tung R, Mathuria NS, Nagel R, Mandapati R, Buch EF, Bradfield JS, et al. Impact of local ablation on interconnected channels within ventricular scar: mechanistic implications for substrate modification. Circ Arrhythm Electrophysiol. 2013;6:1131–8.
Tschabrunn CM, Roujol S, Dorman NC, Nezafat R, Josephson ME, Anter E. High-resolution mapping of ventricular scar: comparison between single and multielectrode catheters. Circ Arrhythm Electrophysiol. 2016;9:10.
Viswanathan K, Mantziari L, Butcher C, Hodkinson E, Lim E, Khan H, et al. Evaluation of a novel high-resolution mapping-system for catheter ablation of ventricular arrhythmias. Heart Rhythm. 2017;14:176–83.
Mantziari L, Butcher C, Kontogeorgis A, Panikker S, Roy K, Markides V, et al. Utility of a novel rapid high-resolution mapping-system in the catheter ablation of arrhythmias. JACC: Clini Electrophysiol. 2015;1:411–20.
Fernández-Armenta J, Penela D, Acosta J, Andreu D, Evertz R, Cabrera M, et al. Substrate modification or ventricular tachycardia induction, mapping, and ablation as the first step? A randomized study. Heart Rhythm. 2016;13:1589–95.
Martínez-Rubio A, Kuschyk J, Sierra G, Breithardt G, Borggrefe M. Programmed ventricular stimulation: influence of early versus late introduction of a third extrastimulus, a randomized, prospective study. Europace. 2002;4:77–85.
Pluta S, Lenarczyk R, Pruszkowska-Skrzep P, Kowalski O, Sokal A, Sredniawa B, et al. Transseptal versus transaortic approach for radiofrequency ablation in patients with cardioverter-defibrillator and electrical storm. J Interv Card Electrophysiol. 2010;28:45–50.
Tilz RR, Makimoto H, Lin T, Rillig A, Metzner A, Mathew S, et al. In vivo left-ventricular contact force analysis: comparison of antegrade transseptal with retrograde transaortic mapping strategies and correlation of impedance and electrical amplitude with contact force. Europace. 2014;16:1387–95.
Steven D, van den Bruck JH, Lüker J, Plenge T, Sultan A. 3-D mapping of ventricular tachycardia in patients with dilative cardiomyopathy. Herzschrittmacherther Elektrophysiol. 2017;28:206–11.
Kaiser L, Jularic M, Akbulak RÖ, Nührich J, Willems S, Meyer C. Catheter ablation of hemodynamically unstable ventricular tachycardia in ischemic cardiomyopathy using high-resolution mapping. Clin Case Rep. 2017;5:389–93.
Takigawa M, Frontera A, Thompson N, Capellino S, Jais P, Sacher F. The electrical circuit of a hemodynamically unstable and recurrent ventricular tachycardia diagnosed in 35 s with the Rhythmia mapping-system. J Arrhythm. 2017;33:505–7.
Maagh P, Christoph A, Müller MS, Dopp H, Plehn G, Meissner A. Point-by-point versus multisite electrode mapping in VT ablation: does freedom from VT recurrences depend on mapping catheter? An observational study. J Interv Card Electrophysiol. 2018;51:169–81. https://doi.org/10.1007/s10840.
Wolf M, Sacher F, Cochet H, Kitamura T, Takigawa M, Yamashita S, et al. Long-term outcome of substrate modification in ablation of post-myocardial infarction ventricular tachycardia. Circ Arrhythm Electrophysiol. 2018;11:e005635. https://doi.org/10.1161/CIRCEP.117.005635.
Andreu D, Penela D, Acosta J, Fernández-Armenta J, Perea RJ, Soto-Iglesias D, et al. Cardiac magnetic resonance-aided scar dechanneling: influence on acute and long-term outcomes. Heart Rhythm. 2017;14:1121–8.
Author information
Authors and Affiliations
Contributions
Arian Sultan, MD: concept/design, data analysis/interpretation, drafting article, statistics, data collection.
Barbara Bellmann, MD: concept/design, data analysis/interpretation, drafting article, statistics, data collection.
Jakob Lüker, MD: data analysis/interpretation, critical revision of article, data collection.
Tobias Plenge, MD: critical revision of article, data collection.
Jan-Hendrik van den Bruck: critical revision of article, data collection.
Karlo Filipovic, MD: critical revision of article, data collection.
Susanne Erlhöfer, MD: critical revision of article, data collection.
Liz Kuffer, MD: critical revision of article, data collection.
Zeynep Arica: critical revision of article, data collection.
Daniel Steven, MD: concept/design, data analysis/interpretation, data collection.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
- No differences were seen regarding safety, efficacy, or feasibility between a transseptal or transaortic LV access. The BC was able to reach all areas of the LV needed for CA and no complications occurred which were related to the BC.
- The use of a high-resolution mapping system for VT/VE ablation facilitates revelation of VT circuits or VE origin in the setting of challenging mapping conditions resulting in favorable acute and long-term success rates.
Rights and permissions
About this article
Cite this article
Sultan, A., Bellmann, B., Lüker, J. et al. The use of a high-resolution mapping system may facilitate standard clinical practice in VE and VT ablation. J Interv Card Electrophysiol 55, 287–295 (2019). https://doi.org/10.1007/s10840-019-00530-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00530-1