Abstract
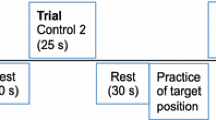
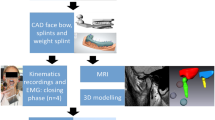
To study the effects of masseter muscle pain on jaw muscle electromyographic (EMG) activity during goal-directed tasks. Mandibular movement was tracked and EMG activity was recorded from bilateral masseter, and right posterior temporalis, anterior digastric, and inferior head of lateral pterygoid muscles in 22 asymptomatic subjects at postural jaw position, and during three tasks: (a) protrusion, (b) contralateral (left), (c) open jaw movement. Tasks were performed during three conditions: control (no infusion), test 1 [continuous infusion into right masseter of 4.5% hypertonic saline to achieve 30–60 mm pain intensity on 100-mm visual analog scale (VAS)], and test 2 (isotonic saline infusion; in 16 subjects only); the sequence of hypertonic and isotonic saline was randomized. The average EMG root-mean-square values at 0.5 mm increments of mid-incisor-point displacement were analysed using linear mixed effects model statistics (significance: P < 0.05). Right masseter hypertonic saline infusion resulted in significantly (P < 0.0005) more pain (mean ± SD VAS 47.3 ± 14.3 mm) than isotonic infusion (12.2 ± 17.3 mm). Although there was evidence of inter-subject variation, the principal EMG findings were that the significant effects of hypertonic saline-induced pain on EMG activity varied with the task in which the muscle participated irrespective of whether the muscle was an agonist or an antagonist in the tasks. The direction of the hypertonic saline-induced pain effect on EMG activity (i.e., whether the hypertonic saline-induced EMG activity was less than or greater than control EMG activity) could change with the magnitude of jaw displacement. Hypertonic saline infusion had no significant effect on postural EMG activity in any of the recorded jaw muscles. The data suggest that under constrained goal-directed tasks, the pattern of pain-induced changes in jaw muscle EMG activity is not clear cut, but can vary with the task performed, jaw displacement magnitude, and the subject being studied.



Similar content being viewed by others
References
Birch L, Christensen H, Arendt-Nielsen L, Graven-Nielsen T, Søgaard K (2000a) The influence of experimental muscle pain on motor unit activity during low-level contraction. Eur J Appl Physiol 83:200–206
Birch L, Graven-Nielsen T, Christensen H, Arendt-Nielsen L (2000b) Experimental muscle pain modulates muscle activity and work performance differently during high and low precision use of a computer mouse. Eur J Appl Physiol 83:492–498
Cairns BE, Sessle BJ, Hu JW (1998) Evidence that excitatory amino acid receptors within the temporomandibular joint are involved in the reflex activation of the jaw muscles. J Neurosci 18:8056–8064
Dworkin SF, LeResche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 6:301–326
Enoka RM, Fuglevand AJ (2001) Motor unit physiology: some unresolved issues. Muscle Nerve 24:4–17
Ervilha UF, Farina D, Arendt-Nielsen L, Graven-Nielsen T (2005) Experimental muscle pain changes motor control strategies in dynamic contractions. Exp Brain Res 164:215–224
Graven-Nielsen T, Svensson P, Arendt-Nielsen L (2003) Interaction between muscle pain and motor control. In: Johansson H, Windhorst U, Djupsjöbacka M, Passatore M (eds) Chronic work-related Myalgia: neuromuscular mechanisms behind work-related chronic muscle pain syndromes. Gävle University Press, Umeå, pp 141–154
Hannam AG, McMillan AS (1994) Internal organization in the human jaw muscles. Crit Rev Oral Biol Med 5:55–89
Hu JW, Tsai C-M, Bakke M, Seo K, Tambeli CH, Vernon H, Bereiter DA, Sessle BJ (1997) Deep craniofacial pain: involvement of trigeminal subnucleus caudalis and its modulation. In: Jensen TS, Turner JA, Wiesenfeld-Hallin Z (eds) Proceedings of the 8th World Congress on pain, progress in pain research and management, vol 8. IASP Press, Seattle, pp 497–506
Huang BY, Whittle T, Murray GM (2005) Activity of inferior head of human lateral pterygoid muscle during standardized lateral jaw movements. Arch Oral Biol 50:49–64
Johansson H, Sojka P (1991) Pathophysiological mechanisms involved in genesis and spread of muscular tension in occupational muscle pain and in chronic musculoskeletal pain syndromes: a hyopthesis. Med Hypotheses 35:196–203
Komiyama O, Arai M, Kawara M, Kobayashi K, De Laat A (2005) Pain patterns and mandibular dysfunction following experimental trapezius muscle pain. J Orofac Pain 19:119–126
Loeb GE, Gans C (1986) Electromyography for experimentalists. University of Chicago Press, Chicago
Lund JP (2001) Pain and movement. In: Lund JP, Lavigne G, Dubner R, Sessle BJ (eds) Orofacial pain: from basic science to clinical management. Quintessence, Chicago, pp 151–163
Lund JP, Sessle BJ (1994) Neurophysiological mechanisms. In: Zarb GA, Carlsson GE, Sessle BJ, Mohl ND (eds) Temporomandibular joint and masticatory muscle disorders. Munksgaard, Copenhagen, pp 188–207
Lund JP, Stohler CS (2007) Critical commentary 2: orofacial pain and jaw muscle activity: a new model. J Orofac Pain 21:282–283
Lund JP, Donga R, Widmer CG, Stohler CS (1991) The pain-adaptation model: a discussion of the relationship between chronic musculoskeletal pain and motor activity. Can J Physiol Pharmacol 69:683–694
Mense S (1993) Nociception from skeletal muscle in relation to clinical muscle pain. Pain 54:241–289
Mense S (2007) Critical commentary 1: orofacial pain and jaw muscle activity: a new model. J Orofac Pain 21:279–281
Mense S, Simons DG, Russell IJ (2001) Muscle pain: understanding its nature, diagnosis, and treatment. Lippincott Williams & Wilkins, Philadelphia
Mesqui F, Palla S (1985) Real-time non-inversion recording and display of functional movements. J Oral Rehabil 12:541–550
Miller AJ (1991) Craniomandibular muscles: their role in function and form. CRC Press, Boca Raton
Mogil JS (1999) The genetic mediation of individual differences in sensitivity to pain and its inhibition. Proc Natl Acad Sci USA 96:7744–7751
Møller E, Sheikholeslam A, Lous I (1984) Response of elevator activity during mastication to treatment of functional disorders. Scand J Dent Res 92:64–83
Mongini F, Tempia-Valenta G, Conserva E (1989) Habitual mastication in dysfunction: a computer-based analysis. J Prosthet Dent 61:484–494
Moseley GL, Hodges PW (2005) Are the changes in postural control associated with low back pain caused by pain interference? Clin J Pain 21:323–329
Murray GM, Peck CC (2007) Orofacial pain and jaw muscle activity: a new model. J Orofac Pain 21:263–278
Murray GM, Orfanos T, Chan JCY, Wanigaratne K, Klineberg IJ (1999) Electromyographic activity of the human lateral pterygoid muscle during contralateral and protrusive jaw movements. Arch Oral Biol 44:269–285
Phanachet I, Whittle T, Wanigaratne K, Murray GM (2001) Functional properties of single motor units in inferior head of human lateral pterygoid muscle: task relations and thresholds. J Neurophysiol 86:2204–2218
Pinheiro JC, Bates DM (2000) Mixed-effects models in S and S-Plus. Springer, New York
Ro JY, Svensson P, Capra NF (2002) Effects of experimental muscle pain on electromyographic activity of masticatory muscles in the rat. Muscle Nerve 25:576–584
Sae-Lee D, Wanigaratne K, Whittle T, Peck CC, Murray GM (2006) A method for studying jaw muscle activity during standardized jaw movements under experimental jaw muscle pain. J Neurosci Methods 157:285–293
Sae-Lee D, Whittle T, Peck CC, Forte ARC, Klineberg IJ, Murray GM (2008) Experimental jaw muscle pain has a differential effect on different jaw movement tasks. J Orofac Pain 22:15–29
Schwartz G, Lund JP (1995) Modification of rhythmical movements by noxious pressure applied to the periosteum of the zygoma in decerebrate rabbits. Pain 63:153–161
Sessle BJ (2000) Acute and chronic craniofacial pain: brainstem mechanisms of nociceptive transmission and neuroplasticity, and their clinical correlates. Crit Rev Oral Biol Med 11:57–91
Sohn MK, Graven-Nielsen T, Arendt-Nielsen L, Svensson P (2000) Inhibition of motor unit firing during experimental muscle pain in humans. Muscle Nerve 23:1219–1226
Sohn MK, Graven-Nielsen T, Arendt-Nielsen L, Svensson P (2004) Effects of experimental muscle pain on mechanical properties of single motor units in human masseter. Clin Neurophysiol 115:76–84
Stohler CS (1999) Craniofacial pain and motor function: pathogenesis, clinical correlates, and implications. Crit Rev Oral Biol Med 10:504–518
Stohler CS, Ashton-Miller JA, Carlson DS (1988) The effects of pain from the mandibular joint and muscles on masticatory behaviour in man. Arch Oral Biol 33:175–182
Svensson P (2007) Critical commentary 3: orofacial pain and jaw muscle activity: a new model. J Orofac Pain 21:284–286
Svensson P, Graven-Nielsen T (2001) Craniofacial muscle pain: review of mechanisms and clinical manifestations. J Orofac Pain 15:117–145
Svensson P, Arendt-Nielsen L, Houe L (1995) Sensory-motor interactions of human experimental unilateral jaw muscle pain: a quantitative analysis. Pain 64:241–249
Svensson P, Houe L, Arendt-Nielsen L (1997) Bilateral experimental muscle pain changes electromyographic activity of human jaw-closing muscles during mastication. Exp Brain Res 116:182–185
Svensson P, Arendt-Nielsen L, Houe L (1998a) Muscle pain modulates mastication: an experimental study in humans. J Orofac Pain 12:7–16
Svensson P, Graven-Nielsen T, Matre DA, Arendt-Nielsen L (1998b) Experimental muscle pain does not cause long-lasting increases in resting electromyographic activity. Muscle Nerve 21:1382–1389
Svensson P, Macaluso GM, De Laat A, Wang K (2001) Effects of local and remote muscle pain on human jaw reflexes evoked by fast stretches at different clenching levels. Exp Brain Res 139:495–502
Svensson P, Wang K, Arendt-Nielsen L, Cairns BE, Sessle BJ (2005) Pain effects of glutamate injections into human jaw or neck muscles. J Orofac Pain 19:109–118
Torisu T, Wang K, Svensson P, De Laat A, Fujii H, Arendt-Nielsen L (2006) Effects of muscle fatigue induced by low-level clenching on experimental muscle pain and resting jaw muscle activity: gender differences. Exp Brain Res 174:566–574
Travell JG, Rinzler S, Herman M (1942) Pain and disability of the shoulder and arm. Treatment by intramuscular infiltration with procaine hydrochloride. J Amer Med Assoc 120:417–422
van Dieën J, Selen LPJ, Cholewicki J (2003) Trunk muscle activation in low-back pain patients, an analysis of the literature. J Electromyogr Kines 13:333–351
Yu X-M, Sessle BJ, Vernon H, Hu JW (1995) Effects of inflammatory irritant application to the rat temporomandibular joint on jaw and neck muscle activity. Pain 60:143–149
Acknowledgments
The research was supported by the National Health and Medical Research Council of Australia (Grants #302005, 512309), the Dental Board of NSW, the Australian Dental Research Foundation, Inc, and by CIHR grant MT-4918. Dr. Daraporn Sae-Lee was the recipient of an International Postgraduate Research Scholarship (IPRS) sponsored by the Australian Government. Some of the data in this paper forms part of her PhD thesis. We also acknowledge the Department of Radiology, Westmead Hospital, for the CT scans. Dr Barry Sessle is the recipient of a Canada Research Chair.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sae-Lee, D., Whittle, T., Forte, A.R.C. et al. Effects of experimental pain on jaw muscle activity during goal-directed jaw movements in humans. Exp Brain Res 189, 451–462 (2008). https://doi.org/10.1007/s00221-008-1439-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-008-1439-0